Hypoxic-Ischemic Encephalopathy
What is Hypoxic-Ischemic Encephalopathy (HIE)?
Brain Damages Caused by Conditions During Labor and Delivery
Hypoxic-Ischemic Encephalopathy is a brain injury caused by reduced oxygen in the blood and decreased blood flow to the brain. This usually occurs around the time a baby is born. But HIE can occur at any time during a woman’s pregnancy, labor and delivery, or after the baby is born.
Caring for a Child with Brain Damage
When brain cells are deprived of adequate oxygen and blood, they die. Irreversible brain damage is the result.
“Hypoxic Ischemic Encephalopathy due to fetal or neonatal asphyxia is a leading cause of death or severe impairment among infants.” - Cerebralpalsy.org
Babies with HIE usually have cognitive deficits, developmental delays, and serious disabilities like cerebral palsy. Their families face long-term and even lifetime consequences, including costly medical treatments, therapies, assistive devices and technology, and caregivers.

HIE is sometimes preventable. Doctors, nurses, midwives, and other medical staff should be aware of risk factors. Careful fetal monitoring and timely intervention could prevent or minimize brain damage for some infants. Failing to do so is medical malpractice.
And families of children harmed by medical malpractice often seek compensation for their child’s injuries from the parties that caused those injuries.
What Is Hypoxic-Ischemic Encephalopathy?
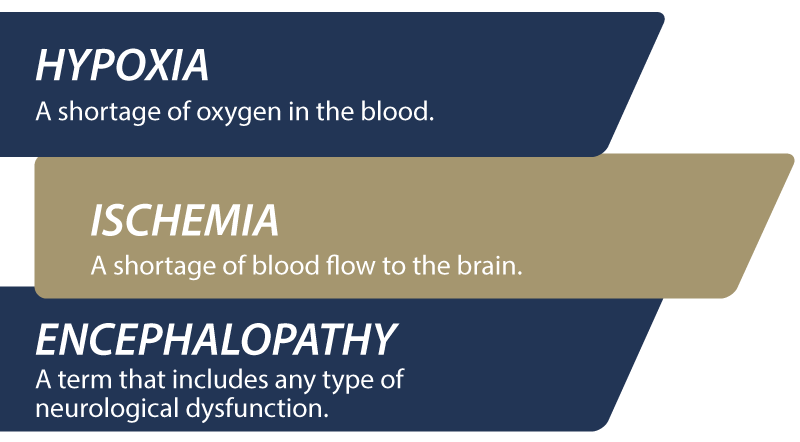
Hypoxic-ischemic encephalopathy (HIE) is a severe birth complication involving severe, permanent brain damage. It’s a complicated injury caused by a series of events. To understand what this condition is, we can start by knowing what each term means:
- Hypoxic – means there’s a shortage of oxygen in the blood
- Ischemic - means the blood flow is reduced
- Encephalopathy – means disease, damage, or malfunction of the brain
Medical professionals may use other terms related to HIE, including:
- Neonatal encephalopathy: Some medical professionals and researchers use this term in place of hypoxic-ischemic encephalopathy.
- Intrapartum asphyxia: This term means oxygen deprivation that occurs during labor. Evidence of intrapartum asphyxia is seen in fetal umbilical arterial blood, fetal bradycardia (low heart rate), lack of fetal heart rate variability with Category III tracings, and low Apgar scores.
- Birth asphyxia (also known as perinatal asphyxia and neonatal asphyxia): This term means the baby experienced breathing difficulties due to a lack of oxygen before, during, and after childbirth.
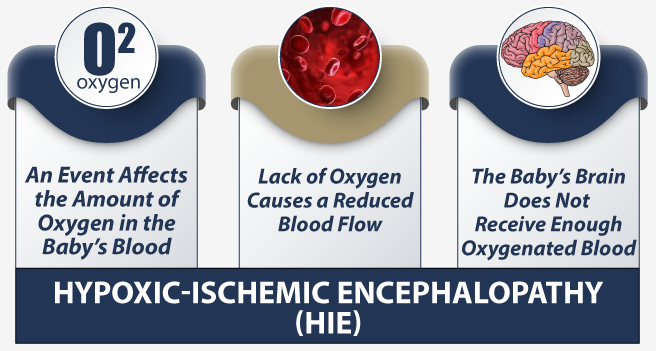
HIE begins when the baby suffers oxygen deprivation (hypoxia). The hypoxia starts a chain of events that can lead to fetal distress and brain damage. When the baby’s oxygen is low, the body tries to give all the available oxygen to the baby’s heart. But the baby still doesn’t have enough oxygen to support itself.
The baby’s heart then begins to show signs of fetal distress due to a lack of oxygen.

With less oxygen circulating in the baby’s blood, its brain and other organs begin to sustain damage. The baby’s liver, kidneys, and lungs may recover fully. And babies with mild brain damage due to HIE may recover somewhat with therapy. However, severe damage to the brain is usually irreversible.
And all this is happening while the mother is focused on delivering the baby. That’s why it’s so critical for medical professionals caring for mom and baby to watch closing for signs and symptoms of oxygen deprivation. They should have the knowledge and experience to properly monitor and treat complications as they arise. In many cases, HIE is preventable when babies and mothers receive proper care.
Symptoms of Hypoxic-Ischemic Encephalopathy
The signs and symptoms of hypoxic-ischemic encephalopathy (HIE) vary from mild to severe and can occur before, during, or after a baby is born. The severity of the brain injury depends in part on the type of injury and its timing.

During childbirth, the mother’s medical team should understand risk factors based on her medical history. For example, complications are more likely when mothers have underlying medical conditions like diabetes and high blood pressure. Doctors and nurses always monitor mothers and babies during childbirth, but at-risk pregnancies need a higher level of monitoring.
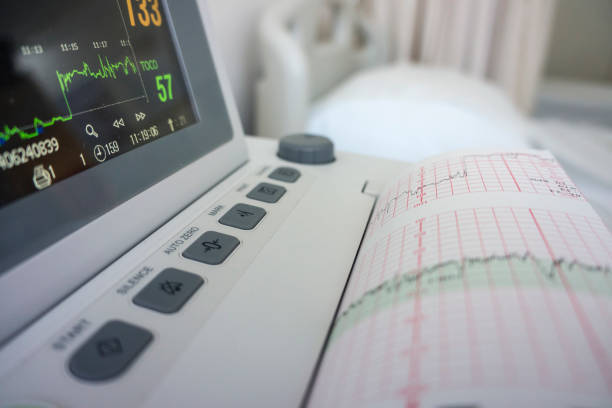
Signs that a baby’s oxygen supply is compromised during labor and delivery include an abnormal fetal heart rate. Certain types of fetal heart tracings indicate oxygen deprivation, shock, or infection:
- Too fast (tachycardia)
- Too slow (bradycardia)
- Poor or missing variability (how the baby’s heart reacts to the mother’s contractions)
After the baby is born, other signs indicate that the newborn has suffered or is continuing to suffer hypoxia (oxygen deprivation):
- Respiratory Difficulties: Neonatal resuscitation may become necessary for babies who have trouble breathing because of HIE.
- APGAR Scores: APGAR scores indicate a newborn’s overall health and wellbeing in the first moments of life. Babies with scores at or below five likely have suffered HIE at birth.
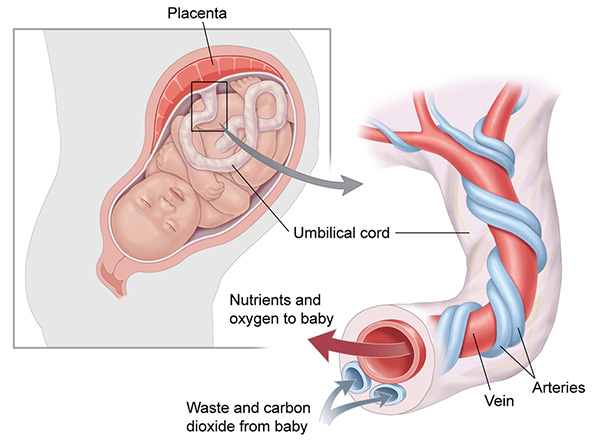
- Umbilical cord tests: Umbilical artery blood samples showing the baby’s blood is acidic (indicating metabolic issues or acidemia) increase the chance the baby has experienced HIE or is currently doing so.
- Meconium-stained fluid: Babies sometimes expel meconium (a waste product) from their intestines into the amniotic fluid. The baby then can breathe in the meconium, aspirate it into their lungs, and become very ill.
- Organ Dysfunction: Oxygen deprivation can damage multiple organs, including the heart, lungs, and liver.
- Mouth and Throat Weakness: A newborn’s inability to latch, suck, swallow or other feeding problems could be caused by weak throat and mouth muscles. They may also use a feeble cry. Such weakness can be the result of a birth injury like HIE.
- Seizures: Seizures that occur shortly after a baby is born are particularly concerning. They can be a sign that the newborn has a brain disorder that could have been hypoxic-ischemic in nature.
- Abnormal newborn reflexes: Newborns with brain damage may be unable to grasp objects and make abnormal movements. They also may fail to react to loud sounds and movements around them.
- Muscle Tone: Low muscle tone or floppiness (hypotonia) often indicates brain damage. Likewise, babies with tighter muscles than average (hypertonia) may have suffered hypoxic-ischemic encephalopathy.
Some of these symptoms can indicate problems other than hypoxic-ischemic encephalopathy (HIE). However, medical professionals have a duty to test newborns who are at risk or exhibiting signs of HIE to determine how to proceed.
Diagnosing Hypoxic-Ischemic Encephalopathy
Obstetricians, nurses, and other medical staff should be aware of a baby’s risk factors. Fetal heart monitoring during labor and delivery gives important clues that a newborn suffered oxygen deprivation (hypoxia). A baby’s insufficient oxygen supplies may have caused reduced blood flow to the brain (ischemia) that in turn caused encephalopathy (brain injury).

Doctors may sometimes identify HIE based on symptoms of a baby’s ischemic stroke. The symptoms of neonatal strokes can come and go very quickly. Transient ischemic attacks, for example, can sometimes only bring physical symptoms for a few hours before returning to normal. But while the baby may appear perfectly fine after a stroke, there can still be hidden signs of brain injuries.
Just suspecting that a baby might have had HIE based on obvious symptoms is not enough. Brain injuries are subtle and sometimes difficult to diagnose. Doctors presume a newborn has HIE should immediately start protective therapies until they perform more tests.
The baby’s doctor may call in a pediatric neurologist to examine the baby. Usually, the doctor or neurologist will review the infant’s medical records paying close attention to lab tests, fetal heart tracings, and other reports. Then, they might use neuroimaging to take a closer look at the baby’s brain:
HIE Brain Imaging
- Magnetic Resonance Imaging (MRI): This test can show whether brain damage occurred or not.
- Cranial ultrasonography: Doctors use this test almost exclusively on babies. It produces pictures of the brain and cerebrospinal fluid and evaluates blood flow.
- Computed Tomography (CT) scan: Although this test is used less often than MRIs, it can be useful when doctors suspect an acute hypoxic or ischemic event.
- Proton Magnetic Resonance Spectroscopy (MRS) – A noninvasive way to get information about metabolic activity in the baby’s brain.
- Electroencephalogram (EEG): A neonatal EEG can help evaluate a baby’s seizure disorder and encephalopathy.

Neuroimaging test results help physicians diagnose HIE and start early intervention to minimize brain damage.
The baby’s prognosis may become more apparent when results are combined with other information about the birth injury, including:
- Fetal heart tracings
- Low Apgar scores
- Umbilical cord gases
- Blood glucose tests
- The need for neonatal resuscitation
Medical professionals also evaluate potential HIE-related brain injury using the Sarnat staging criteria (or a similar staging method). Babies with suspected hypoxic-ischemic encephalopathy are categorized as:
Stages of Hypoxic-Ischemic Encephalopathy
- Stage 1: Baby exhibits hyper alertness, hyperreflexia (spasticity) and has a normal EEG.
- Stage 2: The baby may react slowly to its environment, have hypotonia (low muscle tone), and seizures. This stage sometimes follows Stage 1 but can also appear from birth.
- Stage 3: The baby is flaccid, stuporous (unconscious or unresponsive, and abnormal EEGs.
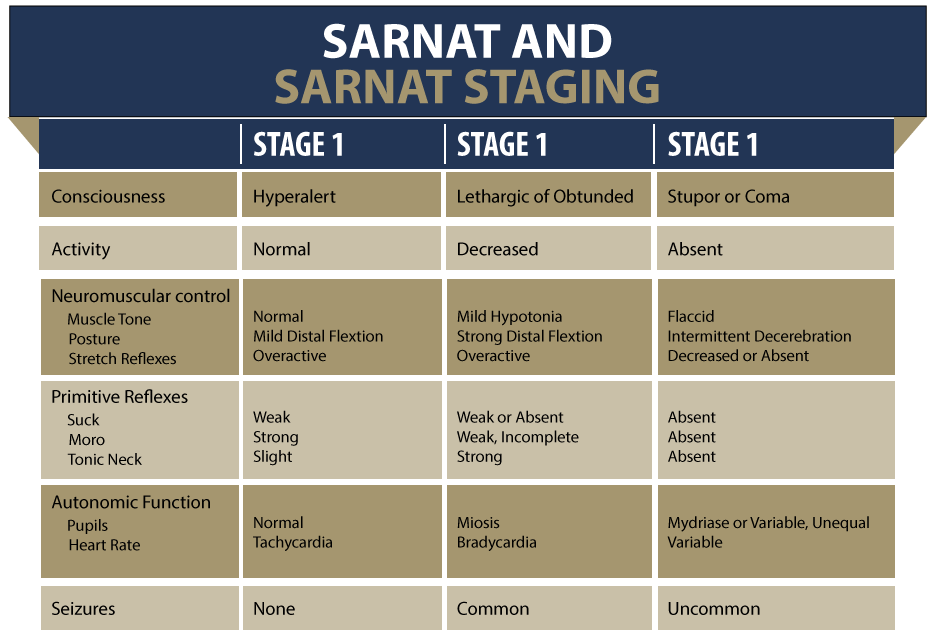
Babies in Stage 3 or Stage 2 that lasts more than five days have a worse prognosis than those in Stage 1.
This type of staging is often used to determine whether a baby should receive hypothermia cooling therapy. This treatment involves lowering the baby’s body temperature for several days to give cells time to recover from HIE.
Diagnosing a newborn with hypoxic-ischemic encephalopathy (HIE) and learning the extent of brain injury is the first step toward treatment.
Treating Newborns with Hypoxic-Ischemic Encephalopathy
When HIE is known or suspected, doctors may take the following action:
Hypothermia Therapy
Hypothermia therapy can reduce brain injury and may improve the baby’s neurological outcome. The therapy involves cooling the baby for 72 hours, and it must start within 6 hours of birth. Doctors use a cooling blanket and medication for hypothermia therapy.
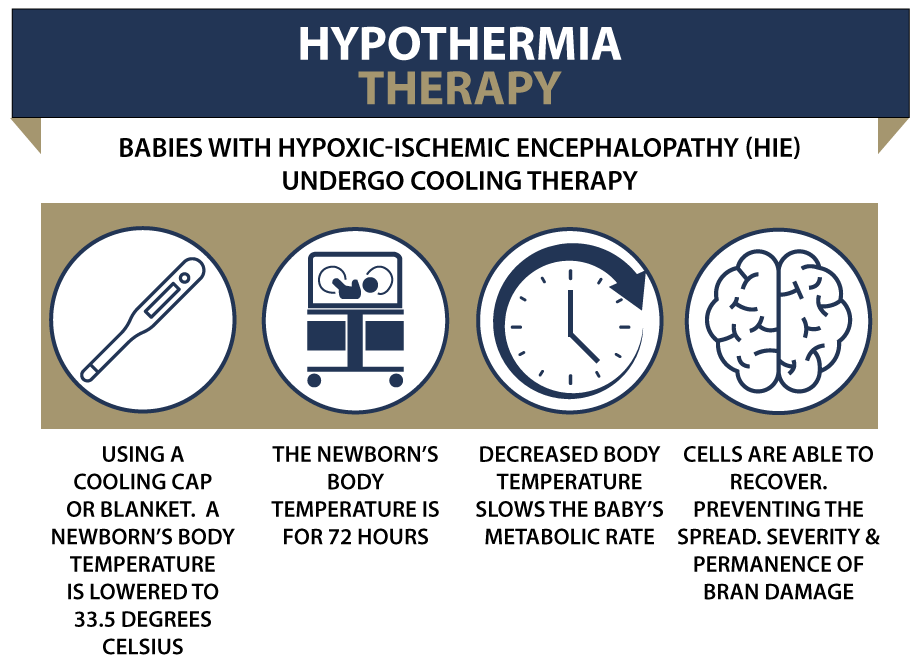
The baby’s medical providers must closely monitor the baby during hypothermia therapy. Specifically, they must watch the infant’s heart rate, breathing, and temperature. Electroencephalograms (EEGs) and cerebral function monitors are also used.
The baby is slowly rewarmed when the therapy ends.
ECMO
Extracorporeal membrane oxygenation (ECMO) therapy might be used for severely injured newborns. Specifically, it can be used for babies in cardiac and respiratory failure.

The machine used is similar to the heart-lung machine used during some surgeries. Tubes move blood from the baby to a part of the machine that functions like an artificial lung (membrane). The membrane adds oxygen to the baby’s blood and removes toxins like carbon dioxide before returning the blood to the infant.
Supportive HIE Treatments
Treatment may be limited to supportive treatments that can address damage to the baby’s:
- Heart and healthy blood pressure
- Kidney and liver function
- Respiration using mechanical ventilation
Some babies may also need medication for seizures caused by their HIE-related brain injury.
Unfortunately, supportive treatment usually does not prevent any ongoing brain injury that occurs in newborns.
Early intervention gives children with very mild HIE a better outcome. Treatments for HIE can prevent or minimize further brain damage. Failing to provide these proper treatments can be medical negligence or malpractice.
Causes and Risk Factors for HIE
With hypoxic-ischemic encephalopathy, brain damage occurs due to low oxygen and poor blood flow to the brain.
But what causes the lack of oxygen (hypoxia)? The exact cause is not always known. However, there are risk factors and conditions that make hypoxia likely. During a woman’s pregnancy, the fetus can be deprived of oxygen because of:
- Placental insufficiency, which can reduce the flow of nutrients and oxygen to the baby
- Preeclampsia, when the mother has high blood pressure and other signs of organ damage
- Existing maternal medical conditions, like diabetes, heart disease, or anemia
- Congenital infections, including viruses
- Drug or alcohol abuse
- Severe fetal anemia, when the baby does not have enough red blood cells to carry oxygen to the rest of the baby’s body
- Fetal lung conditions, like congenital pulmonary airway malformation

As childbirth begins, the baby can experience problems that cause intrapartum asphyxia (oxygen deprivation) and hypoxic-ischemic encephalopathy (HIE):
- Umbilical cord prolapse, compression, or wrapped around the baby’s neck
- Placental abruption, where the placenta pulls away from the uterus before birth
- Placenta previa that can cause severe bleeding during pregnancy or labor
- Uterine rupture that causes excessive bleeding
- Maternal low blood pressure
- Prolonged labor or arrested labor
- Fetal heart monitoring mistakes that miss signs of fetal distress
- Abnormal fetal presentation, like a breech position, that delays birth
- Cephalopelvic disproportion, where the baby is too big for the mother’s pelvis and may get stuck
- Shoulder dystocia, which happens when at least one of the baby’s shoulders is unable to make it through the birth canal
- Delayed C-section that prolongs a difficult birth or a baby’s fetal distress
- Anesthesia errors during childbirth or a C-section
- Assisted delivery when the doctor uses forceps or a vacuum extractor to deliver the baby
- Fetal stroke due to blood flow being blocked, sometimes by blood clots

Finally, newborn infants can be at risk for brain damage caused by HIE if they:
- Were premature
- Have heart or lung disease that limits blood circulation
- Have developed serious infections
- Sustained brain or skull trauma during birth, possibly because of medical negligence or errors
- Have very low blood pressure
Oxygen deprivation (hypoxia) leads to poor blood flow (ischemia), which can cause brain damage (HIE).
“Regardless of the specific cause of injury, the common underlying physiologic processes that result in HIE are diminished cerebral blood flow (ischemia) and reduced blood oxygenation (hypoxemia).”
- Radiological Society of North America
The severity of the hypoxia, how long it lasted, and which part of the brain was affected directly affect the baby’s future.

Can Hypoxic-Ischemic Encephalopathy (HIE) Be Prevented?
The best way to prevent hypoxic-ischemic encephalopathy (HIE) is by preventing asphyxia from occurring. It’s not always possible to do that, but medical professionals might minimize the damage by:
- Prenatal care and testing: The mother’s physician should be aware of high-risk pregnancies and the complications that could occur during labor and delivery. It’s important to get a complete medical history for the mom and conduct tests that pinpoint potentially serious conditions. Doctors can be ready for trouble if they know that it’s likely to occur
- Trying to stop premature births: Obstetricians can give medications like tocolytics and magnesium sulfate that might slow or stop contractions. Delaying delivery gives the baby time to mature. Doctors also administer corticosteroids to the mother to help strengthen the baby’s lungs
- Watch for signs of fetal distress: Closely monitor the baby’s heartbeat and react immediately to changes that indicate oxygen deprivation. Failing to monitor the heart rate or analyze the results is medical negligence and malpractice
- React quickly when fetal distress is suspected: Doctors might first try interventions like changing the mother’s position. Sometimes this helps stop what is harming the baby, like a compressed umbilical cord. If intervention fails, the baby must be delivered as quickly as possible.Delaying the C-section could worsen the baby’s hypoxia and lead to further brain damage
- Properly diagnosing and treating newborns with neonatal encephalopathy: Treatment for newborns suffering from hypoxic-ischemic encephalopathy (HIE) must start within a few hours after birth. Neonatal resuscitation is a first step, but babies with severe HIE might need additional treatment, including hypothermia therapy, to minimize brain damage

Sometimes brain damage from HIE is preventable. However, careful monitoring, close communication among medical professionals, and swift action are necessary. When medical staff fails to meet their standard of care for patients, they can be held accountable for medical negligence and malpractice.
Long-Term Consequences of HIE
Some babies with HIE recover fully. Organs like the heart, liver, and kidneys might recover from mild damage. However, children may not recover from the brain injuries caused by HIE. With early HIE diagnosis and intervention, children may advance as far as possible.

However, other newborns may suffer permanent, severe disabilities, including:
- Developmental delays: The baby will miss important development milestones that relate to average physical, social, language, and cognitive skills
- Cognitive impairment: Children who had HIE may have trouble with cognitive skills like learning, thinking, and problem-solving
- Cerebral Palsy: HIE can lead to cerebral palsy, a complicated condition that can include physical and cognitive disabilities
- Seizure Disorders: Brain damage can cause babies to have seizures
Families of children with hypoxic-ischemic encephalopathy (HIE) can face a lifetime of intense care. Depending on the severity of their child’s brain injury, they might need some or all of the following:
- Surgery
- Medication
- Therapy
- Assistive devices
- Special education and training
- Trained caregivers
Such care is physically, emotionally, and financially draining on families. Families may seek compensation through a birth injury lawsuit when medical professionals failed to provide the care needed to prevent HIE. The compensation a family receives from a birth injury lawsuit can pay for care and other expenses.
Is Your Child’s Brain Injury the Result of Medical Malpractice?
The parents of children who suffered birth injuries from hypoxic-ischemic encephalopathy (HIE) want answers. They want to know what happened to harm their child’s brain. Were there signs of fetal distress that the doctors and nurses failed to recognize and/or failed to respond to in a timely manner? Should their newborn have received treatments immediately after being born?
Our dedicated HIE injury lawyers want to help you find those answers.
We diligently investigate the facts and hold responsible parties accountable by pursuing medical malpractice claims against them. We are trained to review the fetal heart monitor strips with a fine-tooth comb—just like the medical providers should have been doing during your delivery. We have a team of nurses experienced in birth injury that assists us in not only reviewing the fetal monitor strips but the entire labor and delivery and newborn medical record chart.
When we find the necessary evidence, we pursue every means possible to obtain you and your child appropriate compensation. The compensation our clients receive helps them pay for their child’s current and future medical treatment, assistive technology and equipment, and the other expenses associated with caring for a child with brain injuries, seizure disorders, and cerebral palsy.
Sometimes families are nervous to talk to lawyers about their child’s case. Others may simply feel consumed by their circumstances and unable to participate in a lawsuit involving their child’s birth injury. We are here to take a large part of that burden off of you and your family.

Why Should You Talk with the Knowledgeable Attorneys at Miller Weisbrod Olesky?
The only way to find out if you have a birth injury case is to talk to an attorney who understands birth injury.
Our team of committed professionals uses our detailed case review process to assess your potential claim. They start by learning more about you and your child. Then we gather medical records to determine what happened before, during, and after your delivery. We call in skilled medical experts who review your records and let us know if they think medical errors could have caused your child’s injuries.
If we feel medical malpractice was present, we meet with you to discuss how you can receive compensation from the medical professionals who made the errors. At no point in our legal intake process will we ask you to pay anything. The medical review of your case and the consultation are free. We only receive payment when you do.
Contact Miller Weisbrod Olesky
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.