Uterine Rupture
Uterine Rupture During Childbirth
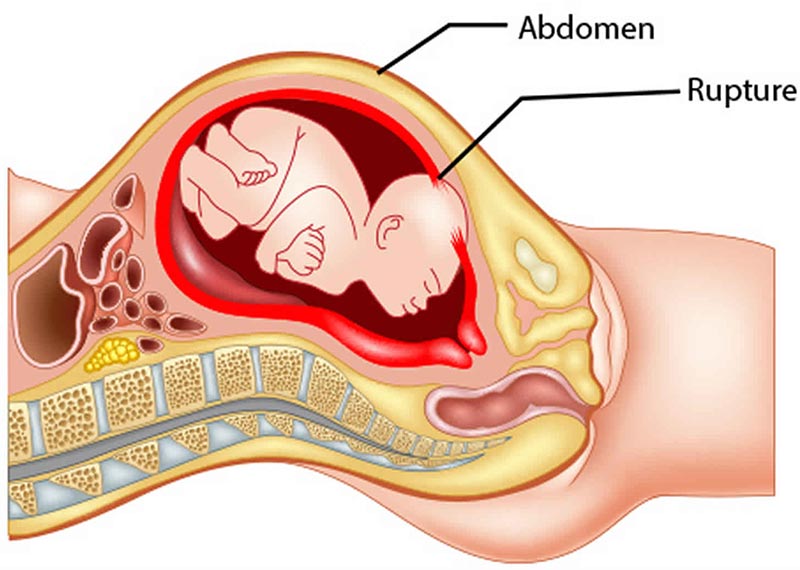
The uterus is the baby’s home during pregnancy, serving as a place to safely develop before birth. However, labor and delivery complications can threaten the uterus and risk severe injury to both the baby and their mother.

A uterine rupture is a rare, but life-threatening labor complication. Doctors and other healthcare professionals must treat it as a medical emergency that requires immediately delivering the baby.
Babies born after their mother’s uterine rupture could suffer severe, permanent physical and cognitive damage. Some may have a birth-related brain injury due to the restriction of oxygenated blood. The most common form of brain damage at birth is called hypoxic-ischemic encephalopathy, also known as HIE. Newborns with HIE will have life-long disabilities, including cerebral palsy and developmental delays.
OB-GYNs, maternal fetal medicine specialists, nurses, midwives, and other healthcare providers have a duty to protect their patients from harm. When they breach this duty (known as the “standard of care”) and cause preventable birth injuries, it constitutes medical malpractice.
Medical professionals must identify risks that can cause a uterine rupture and react immediately if it occurs. Failing to do so could mean they have committed medical malpractice that injured a mother and her newborn.
What Is a Uterine Rupture?

The uterus is a hollow, muscular organ that holds and nourishes unborn babies. The organ itself has three layers:
- Endometrium –the inner, epithelial layer
- Myometrium – the smooth, muscle layer
- Perimetrium – the serosal outer surface of the uterus
A mother’s uterus sometimes becomes scarred on these layers. Previous surgery for cancer, fibroids, or a past C-section can all cause this scarring. Even an unscarred uterus can have genetic weaknesses of the uterine wall or become overstretched.
Vaginal Birth After Cesarean Risks
The uterus can split or rupture through all three layers, whether scarred or unscarred. This usually happens when a mother with a previous C-section undergoes a Trial of Labor After Cesarean (TOLAC).
TOLAC occurs when the mother presents with a previous C-section and attempts a natural or vaginal birth. Doctors also refer to this as a VBAC –Vaginal Birth after Caesarean. Uterine ruptures are the number one serious risk of VBAC.
A uterine rupture endangers the mother and the baby.
What are Risk Factors for a Uterine Rupture?
During the mother's first prenatal testing visit, doctors and nurses get details of her medical history. Some of that history may indicate a higher risk for uterine rupture, including:
- Previous C-section delivery, especially if there was a classic up-and-down incision.
- Attempting a Vaginal Birth After C-Section (VBAC)
- Prior uterine surgeries, like for cancer or fibroid tumors.
- Diseases like Ehlers-Danlos and Loeys-Dietz.
Of these risk factors, a prior C-sections pose the highest risk for a mother's uterine rupture.

During labor, other factors could increase the likelihood of uterine rupture:
- Using labor-Inducing medications, which can make the contractions too hard and fast for the uterus to handle
- Trial of labor after cesarean (TOLAC)
- Multiparity (more than one fetus)
- Abnormal Fetal Position & Presentation (breech or transverse)
- Damage from internal podalic version and external cephalic version (changing the baby’s presentation)
- Macrosomia (a very large baby)
- Prolonged labor, especially with slow cervical dilation
- Uterine perforation from assisted delivery (using devices within the uterus during delivery)
Risk Factors Doctors Can Identify Before and During Labor
During labor, other factors could increase the likelihood of uterine rupture:
- Induction of labor, which can make the contractions too hard and fast for the uterus to handle
- Trial of labor after cesarean (TOLAC)
- Multiparity (more than one fetus)
- Fetal presentation (breech or transverse)
- Damage from internal podalic version and external cephalic version (changing the baby’s presentation)
- Macrosomia (a very large baby)
- Prolonged labor, especially with slow cervical dilation
- Uterine perforation from assisted delivery (using devices within the uterus during delivery)
Unexpected trauma could cause a uterine rupture at any point in the mother’s pregnancy, not just during delivery. Doctors must carefully monitor and treat expecting mothers who suffer abdominal trauma from accidents, falls, or violence.
Failing to diagnose and immediately treat a uterine rupture can lead to permanent, severe damage to the mother and baby.

What are the Signs and Symptoms of a Uterine Rupture?
Typically, a woman’s uterus ruptures during labor. Doctors and other medical staff caring for an at-risk mom should watch for certain signs and symptoms including:
- Fetal distress (non-reassuring fetal heart rate patterns, such as late decelerations)
- Severe abdominal pain and board-like rigidity
- Abnormal blood pressure or unstable blood pressure
- Drop in blood pressure
- Increased heart rate
- Shortness of breath
- Dizziness
Fetal Distress
Fetal distress remains the most important sign of a baby’s oxygen deprivation, which happens when a uterine rupture occurs.
When labor starts, nurses or other staff should start monitoring the mother and baby. A fetal monitor placed on the mother’s abdomen tracks the baby’s heart rate. It is especially important to see how the heart rate reacts to contractions.
Doctors may suspect fetal distress when fetal heart strips show late decelerations, reduced variability, tachycardia, or bradycardia.

An incomplete uterine rupture is considered difficult to diagnose. Complete ruptures are not, but careful monitoring and observation can reduce or even eliminate the risk of complications.
What are the Complications of a Uterine Rupture?
After a complete uterine rupture, the contents of the uterus can spill into the mother’s abdomen. Other complications the mom faces include:
- Severe bleeding
- Blood transfusions
- An emergency cesarean section (C-section) birth
- Hysterectomy
- Maternal mortality
Complications for the baby depend on several factors, including:
- Whether the rupture was full or partial, and
- How quickly doctors surgically intervene to remove the baby.
The worst-case scenario happens when the baby either partially or fully ejects from the mother’s ruptured uterus into her abdomen. Doctors must perform quick surgical intervention in these cases to save both mother and the baby.
After the uterine rupture occurs:
- The mother’s severe bleeding reduces blood flow to the baby.
- The baby also receives less oxygen and can suffer from hypoxia (reduced oxygen) or anoxia (total lack of oxygen). Either condition can cause brain and organ damage like HIE.
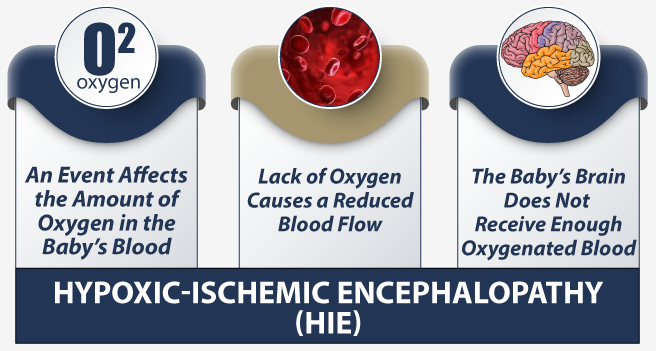
Hypoxic ischemic encephalopathy (HIE) is a serious birth injury that can result from birth asphyxia from uterine ruptures. Medical providers must recognize the signs of HIE and treat newborns immediately. Treatments like therapeutic hypothermia can help to stop or reduce progressive brain damage.
Reducing the risk of uterine rupture begins during a woman’s pregnancy.

How to Treat a Uterine Rupture?
Doctors must move quickly once they suspect a mother has suffered from a ruptured uterus. A baby in fetal distress due to a uterine rupture requires an immediate delivery via an emergency C-section. The mother is at great risk for extreme maternal hemorrhaging and even maternal death.

The American College of Obstetricians and Gynecologists (ACOG) ) recommends no more than a 30 minute wait for the initiation of the C-section.
However, studies have shown that delivering the baby within that 30-minute window does not always prevent serious damage like HIE. This is especially true when the baby has slips through the rupture into the mother’s abdomen.
Missing or ignoring the risks and signs of uterine rupture puts the baby and mother at risk. Mothers could go into shock, require transfusions, or die. And babies could suffer permanent brain injuries in the form of hypoxic-ischemic encephalopathy (HIE), cerebral palsy, and cognitive disabilities.

How to Prevent a Uterine Rupture?
Ideally, any mother at risk for uterine rupture should deliver in a facility that is able to conduct monitoring and emergency c-sections. In order to undergo a trial of labor for a VBAC delivery, the ability to do a c-section is mandatory. If doctors do not properly plan or arrange the procedure in advance, it can constitute medical malpractice.
Doctors, nurses, midwives, and other medical staff could also take the following steps to identify and treat uterine ruptures:
- Be wary of inducing labor with prostaglandins
- Observe mothers with a high-risk pregnancy more closely
- Scheduling a C-section before the mother’s due date instead of trying TOLAC
- Perform TOLACs for VBAC mothers in well-staffed and equipped hospitals
- Inform patients of the risks of vaginal birth after cesarean (VBAC)
- Watch for issues with abnormal fetal position & presentation
- Closely monitor the baby for signs of fetal distress

Uterine ruptures usually happen quickly and sometimes with little warning. However, doctors and other providers have a responsibility to watch for risk factors and warning signs. When they fail to do so, families must deal with the heartbreaking consequences.
Is Your Child’s Birth Injury the Result of Medical Malpractice?

The parents of children who suffered birth injuries after a uterine rupture often want answers. They want to know what happened to harm their child’s brain.
- Were there signs of fetal distress that the doctors and nurses failed to recognize or failed to recognized or failed to respond to?
- Did doctors attempt a VBAC when a c-section was more appropriate?
- Did the doctors and nurses fail to immediately react when they suspected a uterine rupture or when it actually occurred?
Our dedicated birth injury lawyers want to help you find the answers to these and many more questions.
We diligently investigate the facts, including a detailed examination of fetal heart rate monitoring strips and labor and delivery records. If this review shows the medical providers did not diagnose or respond to fetal distress, we hold responsible parties accountable by pursuing medical malpractice claims against them.
The compensation our clients receive helps them pay for their child’s current and future birth injury treatment. This may include assistive equipment and devices, and other expenses associated with treating brain injuries, seizure disorders, and cerebral palsy.
Sometimes families are afraid to talk to lawyers about their child’s case because they worry there is a fee. There is never a fee unless and until we make money recovery for our clients.
What is the Statute of Limitations in a Birth Injury Case?
A statute of limitations (SOL) is a law that sets a time limit on how long an injured person has to file a lawsuit after an accident. It is essential to understand statutes of limitations vary based on the type of case and state where you file. The birth injury claims deadline typically differs from other claims like injury to personal property, fraud, and collection of debts.
Generally, the clock starts ticking on the date the injury occurred. However, there are exceptions to this rule. In some cases, the statute of limitations starts when a person discovers or reasonably should have discovered an injury. When dealing with government agencies, SOLs can become even more complex.
For example, if the party that injured you was:
- A federal employee
- Employed by a military hospital, Veterans Administration facility, or a federally funded medical entity
You may need to file a birth injury claim under the Federal Tort Claims Act (FTCA). In FTCA cases, claimants must go through certain administrative procedures before filing a lawsuit. In some states, you may need to give a shorter notice of filing if:
- The negligent party was a local or state government hospital.
- The doctors and medical providers are employees of a governmental entity.
If you file your case outside of the statute of limitations, the courts will typically dismiss it. This means you will not be eligible to recover compensation for your injuries. Determining when a statute of limitations begins on your case can be tricky. If you're considering pursuing compensation for a birth injury, don't hesitate to contact an attorney as soon as possible.
How Our Dedicated Birth Injury Attorneys Can Help?

It takes an expert review of the facts of your child's birth before determining whether medical malpractice occurred.
Our Process
At Miller Weisbrod Olesky, our team uses a detailed medical negligence case review process to assess your birth injury case. We start by learning more about you and your child and the status of meeting/missing developmental milestones. Then we gather medical records to determine what happened before, during, and after your delivery. We call in skilled medical experts who review your records and examine what actions medical professionals took in response.
If we feel doctors mismanaged your uterine rupture and it led to preventable injuries, we meet with you to discuss. We will speak about how you can receive compensation from the medical professionals who made the errors.
At no point in our legal intake process will we ask you to pay anything. The medical review of your case and the consultation are free. We only receive payment when you do. The sooner you reach out, the sooner we can begin investigating and gathering the evidence needed to support your claim.
We work on a contingency fee basis, meaning you won't pay any legal fees unless we win your case. Contact us today to schedule your free legal consultation by calling our toll-free line at (888) 987-0005 or by filling out our online request form.
Contact Our National Birth Injury Lawyers
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.