Chorioamnionitis
What Is Chorioamnionitis?
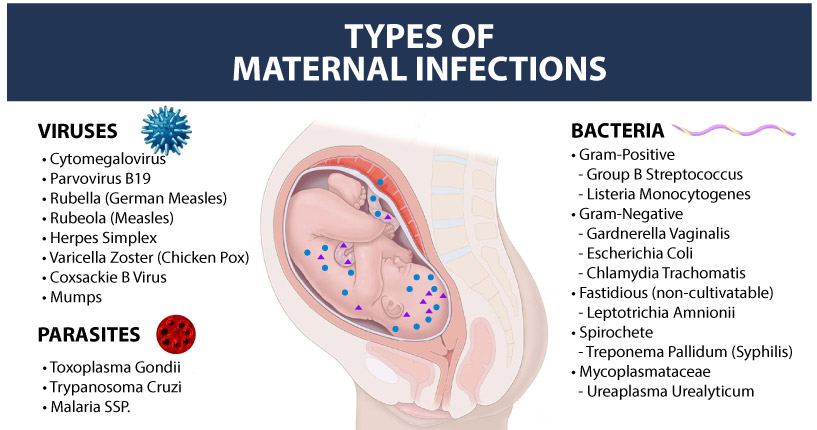
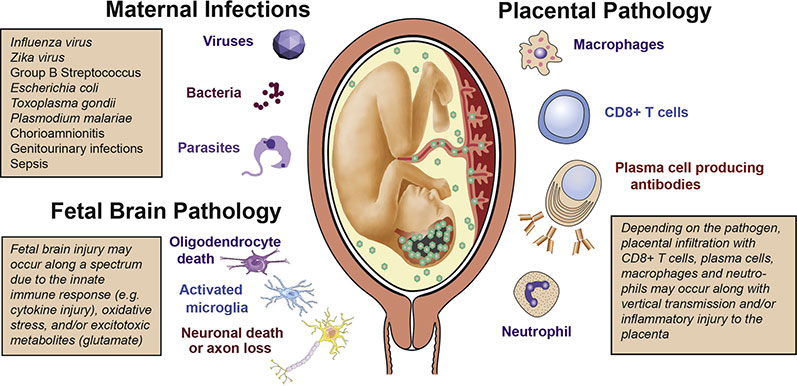
Chorioamnionitis is an acute bacterial infection of pregnancy that enters the mother’s uterus and invades the membrane and amniotic fluid that surrounds the baby. The most common bacteria causing chorioamnionitis are Group B Strep or E.Coli.
Chorioamnionitis typically occurs when the amniotic sac is broken for an extended period prior to birth. This situation is known as “premature rupture of membranes” or PROM. Another typical scenario where chorioamnionitis may develop is where the expectant mother has prolonged labor.
A delayed diagnosis or improper management of chorioamnionitis can lead to serious fetal complications, such as preterm birth, meningitis, neonatal sepsis, pneumonia, and cerebral palsy.
When chorioamnionitis is diagnosed, antibiotic therapy should be given to the mother as a preventative strategy to reduce the chances of transmission of the infection to the baby as well as reducing the chances of a birth injury due to the infection.
Medical providers should be prepared to perform an emergency cesarean section as part of the treatment of chorioamnionitis when necessary. Babies that are born to mothers with a chorioamnionitis infection will often require neonatal resuscitation and immediate antibiotic treatment. During the first hours after birth, doctors and nurses should carefully monitor these babies’ glucose levels and treatment any drops because they are at higher risk for neonatal hypoglycemia.

How To Diagnose Chorioamnionitis?
Typically, Chorioamnionitis is diagnosed based on clinical symptoms such as maternal fever, an examination of the changes to the umbilical cord and placenta (histopathological exam), or with a microbiological examination of the amniotic fluid culture.
Some of the important clinical findings related to chorioamnionitis include:
Maternal Fever
This is the most significant clinical sign, which should alert the medical team to the possibility of chorioamnionitis. During pregnancy, if the expectant mother’s body temperature exceeds 100.4°F and persists for at least one hour, or the fever is 101°F or higher, it warrants a prompt evaluation for chorioamnionitis followed by an appropriate medical intervention.
Maternal fever is found in almost 95 to 100% of patients with chorioamnionitis. When an expectant mother is administered epidural anesthesia, it can also induce fever (epidural fever) and mask the presence of chorioamnionitis. Therefore, medical providers should rule out the possibility of this serious infection instead of presuming that the patient’s fever is only related to epidural medications.
Some research studies have, in fact, shown that in expectant mothers who receive epidural anesthesia, the incidence of placental inflammation (chorioamnionitis) is higher (35% in the epidural group vs. 17% in the non-epidural group). This finding indicates that chorioamnionitis may be the pathologic basis (underlying cause) behind the occurrence of epidural fever.
Maternal and Fetal Tachycardia
Maternal tachycardia (heart rate of the expectant mother is higher than 100 beats per minute) is reported in up to 80% of the cases of clinical chorioamnionitis. Fetal tachycardia (the baby’s in-utero heart rate is greater than 160 BPM) is reported in up to 70% of the cases. Since tachycardia may also occur without chorioamnionitis, medical providers should carefully assess for other potential underlying causes as well.
Sometimes medications, such as antihistamimes, ephedrine and beta agonists may also contribute to an increased level of maternal or fetal tachycardia. But when tachycardia and maternal fever are seen together, it is a strong indicator of chorioamnionitis, and should be evaluated and treated accordingly.
Other Signs
While maternal fever and maternal/fetal tachycardia are more objective measurements, medical providers should also consider subjective signs, such as a foul odor in the amniotic fluid and uterine fundal tenderness (tenderness in the top part of the uterus). These subjective signs are reported in up to 25% of the cases of clinical chorioamnionitis.
Fundal tenderness should be carefully interpreted because it can sometimes get masked by analgesics during labor or complicated by the pain related to placental abruption.
When the chorioamnionitis infection is prolonged or severe, foul odor of the amniotic fluid is more likely to occur. When chorioamnionitis is present subclinically (which means the clinical signs are not seen), it may manifest as PROM or PPROM (preterm PROM).

What Tests Are Helpful In Diagnosing Chorioamnionitis?
Certain Lab Tests are important tools for doctors, like obstetricians and maternal fetal medicine specialists, to use to diagnose this serious infection. The most common lab tests are:
Complete Blood Count (CBC)
When the while blood cell (WBC) count is higher than 12,000/mm3, the condition is known as maternal leucocytosis. This usually supports the diagnosis of clinical chorioamnionitis because leucocytosis is found in up to 90% of the cases with this infection. But in absence of other symptoms, isolated leucocytosis has limited value because conditions such as labor or use of steroids may also induce its occurrence.
Amniotic Fluid Tests
Amniocentesis may be used to perform amniotic fluid testing to detect the presence of bacterial infection and diagnose chorioamnionitis. While the amniotic fluid culture test is highly reliable, its utility is limited by the fact that it takes up to three days to obtain culture results.
Secondly, amniocentesis is an invasive procedure, which may not be performed in most cases that occur around the time of labor. Some medical providers may use this invasive procedure at an earlier stage (when chorioamnionitis is suspected) in order to decide whether premature delivery is warranted.
Umbilical Cord and Placental Pathology
An examination of the amnionic membrane (outer tissue of the amniotic sac) and chorion membrane (inner tissue of the placenta) can reveal acute histologic changes (changes in the tissue caused by infection). This examination captures not only clinical but also sub-clinical chorioamnionitis (where external signs of the condition are not seen.)
Therefore, a placental pathologic exam should be performed for confirming the diagnosis even when amniotic fluid culture shows negative results. Similarly, a pathologic exam of the umbilical cord can reveal inflammation (condition known as funisitis).
Funisitis is even more medically concerning than isolated chorioamnionitis because it represents the baby’s inflammatory response to the maternal infection. (Note: Funisitis or inflammation of the umbilical cord is present in up to 60% of all cases of clinical chorioamnionitis.)
How Do You Treat Chorioamnionitis?
Antibiotics, such as erythromycin and ampicillin have been shown to improve health outcomes for the baby as well as a reduction in chronic lung disease and hypoxic-ischemic encephalopathy (which may lead to cerebral palsy.)
Antibiotics are the critical part of the treatment plan when chorioamnionitis is diagnosed. The medical provider will typically administer them through an IV (delivering medication directly into the vein through a needle).
In many cases, an emergency cesarean section can be performed to prevent additional complications for the mother and the baby. Immediately after birth, if the newborn is diagnosed with infection, they should also be given antibiotics to improve neonatal health outcomes.
Babies that suffer from chorioamnionitis often suffer from breathing difficulties at birth. As such, a neonatal resuscitation team should be called and prepared to act at birth. Delays in neonatal resuscitation can often cause more severe birth injuries than the infection itself.
Another common complication of babies with chorioamnionitis is neonatal hypoglycemia. Babies with infections may suffer dangerous drops in their glucose levels shortly after birth. If this glucose level is not corrected, it can lead to a brain injury.
Is Your Child’s Birth Injury the Result of Medical Malpractice?
Parents whose children suffer from birth injuries or birth complications associated with chorioamnionitis want and deserve answers as to cause of their child’s injury and whether mistakes by the doctors and nurses contributed to the injury.
- Were there signs of a birth injury during the pregnancy, labor, and delivery process, or presence of risk factors, which were either not recognized or properly treated?
- Did the medical team fail to order a series of tests to diagnose a suspected birth complication in a timely manner?
- Was the decision to perform a cesarean delivery delayed?
- During the labor and delivery, were there clear indications that their baby was suffering from fetal distress, but appropriate actions were not taken by the obstetrician or nurses?
- Did the neonatal resuscitation team delay in providing important breathing support after birth?
- Were serious neonatal conditions like hypoglycemia or jaundice missed or treated incorrectly?
- Should brain cooling (also called “hypothermia therapy”) have been offered to your baby, but the doctors and nurses failed to perform the appropriate tests or ignored the results of the tests?
The experienced birth injury lawyers at Miller Weisbrod Olesky, who have been through the legal battlefields before, will help you determine if mistakes of the medical providers caused a birth injury to your child, including Hypoxic-Ischemic Encephalopathy (HIE) or cerebral palsy. Our profound and proven birth injury attorneys have represented families all over the United States in their time of need after a birth injury.
We use our experience and expertise to obtain you and your child a medical malpractice settlement that will help provide specialized medical therapy in order to maximize the quality of life and independence of your child throughout their life.
Sometimes families are reluctant to contact a medical malpractice lawyer. It’s also not uncommon for parents to feel overwhelmed by the responsibilities they encounter in caring for their injured child and worried that they will not be able to help out in a lawsuit involving their child’s birth injury. Our birth injury attorneys and nursing staff will address these hesitations and concerns, so you can focus on your child and maximizing their care.
Registered Nurses and Nurse-Attorneys Are a Vital Part of Our Birth Injury Team…and Yours

Most birth injury law firms will employ one or two nurses to assist the review of cases and medical research. But Miller Weisbrod Olesky offers an unmatched number of nurses and nurse-attorney employees support to both the birth injury attorneys and our clients.
Our team of registered nursing staff and nurse-attorneys bring a deep level of medical and personal insight to every client’s case. Our nursing team includes both an experienced labor and delivery nurse as well as an ICU nurse. Working closely with the rest of the team, they investigate the reasons behind a birth injury and how medical professionals breached their standard of care.
Why Should You Talk with the Knowledgeable Attorneys at Miller Weisbrod Olesky?

The only way to find out if you have a birth injury case is to talk to a lawyer experienced in birth injury lawsuits. It’s not uncommon that a birth related complication results in a preventable birth injury, including cerebral palsy, but it takes a detailed expert review by a birth injury attorney of the medical records from your child’s birth to determine if the birth injury was the result of medical malpractice.
At Miller Weisbrod Olesky, a team of committed lawyers, nurses and paralegals uses our detailed medical negligence case review process to assess your child’s potential birth injury case. We start by learning more about you and your child and the status of meeting/missing developmental milestones. Then we gather medical records to determine what happened before, during, and after your delivery. We call in skilled medical experts who review your records and let us know if they think medical errors could have caused your child’s injuries.
If we feel medical negligence caused or contributed to your child’s injuries, we meet with you to discuss how you can receive compensation from the medical professionals who made the errors. Our birth injury attorneys have recovered millions of dollars in settlements for families of children that have suffered a birth injury.
At no point in our legal intake process will we ask you to pay anything. The medical review of your case and the consultation are free. We only receive payment when you do.
Contact Our Birth Injury Lawyers
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.