Forceps and Vacuum Extraction Injury
What Are Forceps and Vacuum Extraction Injuries?
Two Methods of Assisted Vaginal Delivery
Sometimes mothers are unable to deliver their babies through no fault of their own. Complications can arise that make natural vaginal delivery dangerous for both mom and baby.

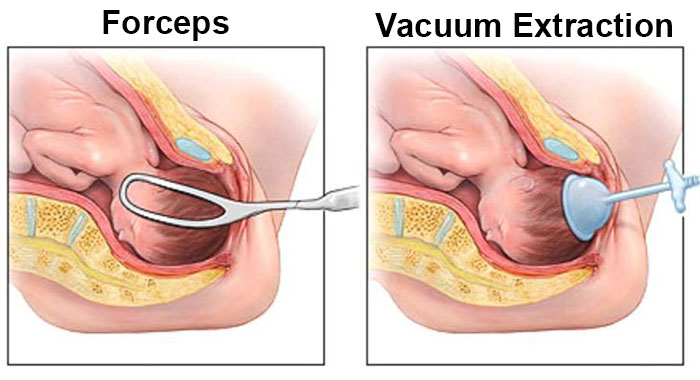
Physicians sometimes recommend assisted vaginal delivery to deliver a baby when unassisted delivery is unlikely or impossible. Forceps and vacuum extraction are two types of equipment used for assisted vaginal delivery.
The theory behind forceps and vacuum extraction may seem sound, but the practice is often flawed. The very medical providers a mother trusts to help bring her child into the world may negligently cause irreparable harm through mismanagement and misuse of these methods.
Understanding a Forceps Delivery

Although several types are available, forceps generally consist of a handle, lock, shank, and blade. Some types are known to cause higher rates of complications, both maternal and fetal. Obstetricians and other medical providers performing an assisted delivery should be aware of the increased risk.
During a forceps delivery, the doctor inserts the forceps into the mother’s vagina. The forceps are then positioned around the baby’s head. The doctor then applies traction, pulling on the baby’s head while the mother pushes. Adjusting the baby’s position usually happens between contractions.
Assisted vaginal delivery is not recommended for all women in labor. Physicians must consider certain criteria before attempting a forceps delivery, including:
- Is the mother’s pelvis large enough for a successful vaginal birth, assisted or natural?
- Is the mother’s cervix fully dilated?
- Have her membranes ruptured?
- Has the baby’s head dropped into the mother’s pelvis?
- What is the baby’s estimated weight?
- Where is the baby located in the birth canal (what is the baby’s “station”)?
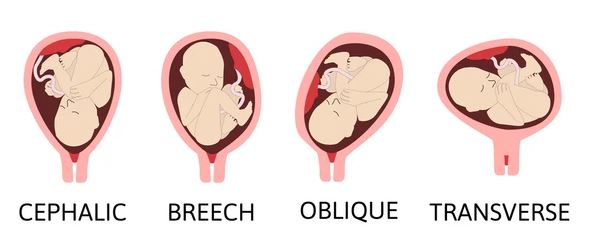
- What are the baby’s position and presentation?

After carefully assessing the mother, doctors may recommend forceps delivery because of:
- Prolonged labor: The mother is pushing, but labor has stalled or the mother is too tired to or for other reasons cannot effectively push.
- Fetal distress: The baby has an abnormal heartbeat on the electronic fetal monitor that could signal problems like hypoxic-ischemic encephalopathy (HIE). This is an acceptable use of forceps only if it is determined that forceps will allow faster delivery than an emergency c-section.
- Maternal medical conditions: Doctors may advise mothers with high blood pressure or heart disease to limit their time pushing.
Doctors, including obstetricians, must be prepared to abandon a forceps delivery and move to a c-section (including an emergency c-section) if the forceps delivery is not quickly successful.
However, assisted vaginal delivery using forceps can be risky or dangerous for the mother and her unborn child if:
- The baby is presenting shoulder or arms first
- Cephalopelvic disproportion is present, which means the baby’s head is too large to pass through the mother’s pelvis
- The unborn child suffers from serious blood or bone disorders
- The baby’s head is too high in the birth canal (“high forceps delivery”)
- The pregnancy is less than 34 weeks—due to the risk of causing an brain bleed
It’s also important to consider potential complications. During or after a forceps delivery, mothers may experience the following:
- Uterine rupture
- Tears to the lower genital tract
- Increased pain and recovery time
- Urinary or fecal incontinence
Newborns delivered through forceps also can be injured. Minor facial lacerations may heal in a few days, but injuries like the following can have a longer-lasting effect:

After a forceps delivery, newborns should be monitored closely for signs of complications. Breathing difficulties and suspected brain damage sometimes need more intense neonatal care. Babies may benefit from neonatal resuscitation or hypothermia therapy (cooling) to prevent or minimize brain damage like hypoxic-ischemic encephalopathy (HIE). HIE is a leading cause of cerebral palsy.
Another form of assisted vaginal delivery appears to be gaining in popularity. However, this method – vacuum extraction – also poses risks when mismanaged or misused.
Understanding a Vacuum Extraction Delivery

A vacuum extractor consists of a metal or soft cup attached to a vacuum pump. The suction cup is applied to the top of the baby’s head in the birth canal. As with forceps delivery, vacuum-assisted vaginal delivery involves the use of traction to pull the baby into the world. This technique is useful in some deliveries, but only if specific criteria are met.
Physicians and other medical professionals caring for a woman in labor may recommend vacuum extraction delivery because:
- The mother’s labor is prolonged or arrested in the second stage. A longer labor places unacceptable stress on the unborn child
- The mother may be too exhausted to continue pushing. Her doctor may also limit her time pushing due to serious health conditions
- The baby’s heart rate is non-reassuring. This indicates fetal distress that could be caused by reduced blood flow and oxygen to the baby’s brain. Hypoxic-ischemic encephalopathy (HIE) can result from such reduced flow. But this choice is only acceptable if the baby cannot be delivered quicker using an emergency c-section

The American College of Obstetricians and Gynecologists (ACOG) recommends that physicians use the following criteria to determine eligibility for vacuum extraction delivery:
- The mother’s cervix is fully dilated
- Her membranes (waters) have ruptured
- The baby’s head is engaged in a vertex presentation
- The doctor knows the fetal position and fetal presentation in the uterus (headfirst, feet first, occiput posterior or anterior)
- An estimate of the baby’s weight has been taken
- The mother’s pelvis is large enough to accommodate the baby
- The mother’s bladder has been emptied
- Healthcare providers have explained the risks and benefits of vacuum extraction delivery
- The doctors have a plan for delivery if vacuum extraction fails
- The mother’s time for pushing is limited because of a maternal health condition
Even if the mother appears eligible for assisted vaginal delivery, doctors must consider the risk to the baby. Vacuum extraction is NOT recommended in some situations, including:
- Macrosomia: The baby is larger than average
- Prematurity: This procedure is too risky for premature babies
- Cephalopelvic disproportion: The baby’s head is too large to pass through its mother’s pelvis
- Abnormal fetal position: The baby must be headfirst and must have progressed into the mother’s birth canal. This technique poses a danger to unborn babies that need to be rotated
- Fetal medical conditions: Vacuum extraction should not be done when the fetus has a bleeding disorder
- Fetal scalp sampling: Medical professionals may take blood samples from the baby’s scalp or attach internal fetal monitors. In either case, vacuum extraction should be avoided

Vacuum extraction should last no more than 20 minutes. This assisted vaginal delivery method should be stopped if the cup detaches multiple times from the baby’s head. Also, doctors should stop immediately if they see signs of trauma to the baby’s scalp. When a vacuum extraction fails, an emergency c-section is often required.
In addition to minor lacerations, newborn babies may experience the following complications after vacuum extraction:
- Caput succedaneum: Babies with this condition – also called scalp edema – have swelling that causes a cone-headed appearance
- Cephalohematoma: Blood pools between the baby’s skin and skull
- Intracranial hemorrhage: This type of bleeding occurs inside the skull, causing pressure on the brain itself. Unless treated quickly, the baby could suffer permanent brain damage or die
- Retinal hemorrhage: Babies born through assisted vaginal delivery (instrumental deliveries) are far more likely to suffer retinal hemorrhages
- Hyperbilirubinemia: The bruises caused by vacuum extraction can lead to increased bilirubin and jaundice. Left untreated, jaundice can develop into a life-threatening condition called kernicterus
- Skull fractures: Vacuum extraction can cause skull fractures and neurological injuries. The fetal skull is very soft, so the cup must be carefully placed in the correct position to avoid skull or brain damage

Complications for the mother tend to be minor pain, lacerations, and hematomas. But newborns may sustain injuries that last for a lifetime. For example, brain damage due to vacuum extraction can lead to cerebral palsy, cognitive disability, developmental delays, and seizure disorders.
When these injuries are caused by medical malpractice or medical negligence, families may be entitled to compensation that provides a better quality of life.
Forceps vs. Vacuum Extraction
These two methods of assisted delivery have some very distinct differences. Physicians who choose the wrong method without careful attention to eligibility criteria and proper guidelines place their patients at unacceptable and unnecessary risk.
Generally, forceps offer a higher rate of successful vaginal delivery than vacuum extraction. However, vacuum extraction is easier to learn and may offer faster delivery than forceps.
Newborns delivered with forceps are less likely to suffer certain neonatal injuries, including cephalohematoma and retinal hemorrhage than those delivered by vacuum extraction. But those born by vacuum extraction sustain fewer craniofacial injuries than those delivered with forceps.
The American College of Obstetricians and Gynecologists (ACOG) has clearly stated that doctors cannot use more than one assistive device during a delivery—meaning it is never appropriate to switch to forceps after a failed vacuum extractor delivery or vice-versa.
Another consideration is the mother’s comfort. Forceps deliveries cause less genital trauma and postnatal discomfort. Recovery may be more comfortable for the mom when her baby is delivered by forceps.
Currently, more physicians and patients are choosing vacuum extraction over forceps. Forceps are used in about 0.5 percent of vaginal births, while vacuum extractions account for 2.6 percent of vaginal births.
What About C-Sections?

It is safer to deliver the baby by cesarean section (C-section) than by assisted vaginal delivery in many situations. Physicians should perform a C-section if delivery by forceps or vacuum extraction fails.
However, medical providers must plan ahead. Assisted vaginal births should only be performed in facilities equipped for emergency C-sections. To do otherwise places the baby and mother at an unacceptable level of risk. In cases where the baby shows signs of continued fetal distress, an emergency C-section must be done in order to prevent a birth injury that could cause brain damage including HIE and cerebral palsy.
Where Medical Professionals Can Go Wrong with Assisted Vaginal Delivery
Forceps and vacuum extraction deliveries can be the best way to birth a baby before a birth injury or brain damage occurs but only under certain conditions. But medical caregivers – including doctors, midwives, nurses, and hospitals – sometimes fail.
In fact, they may fail their patients in many ways, including:
- Failing to explain the risks and benefits of a procedure to a patient
- Failing to obtain informed consent before beginning the procedure
- Performing assisted vaginal delivery in a facility that is not equipped to handle an emergency C-section
- Attempting forceps or vacuum extraction with insufficient training or experience
- Failing to monitor mother and baby before, during, and after delivery
- Failing to abandon the procedure when it lasts too long or has not been successful
- Failing to recognize the signs of fetal distress during the procedure
- Using excessive traction on the baby’s head during the procedure
- Using the forceps or vacuum extractor when a c-section should have been performed instead

Doctors, nurses, midwives, hospitals, and other medical caregivers sometimes do not meet their duty of care. Mothers, babies, and their families then face lifelong consequences when a birth injury occurs like brain damage, cerebral palsy, seizure disorders, cognitive disabilities, and developmental delays. You may not realize your baby’s condition was caused by medical negligence and malpractice unless you speak with an experienced birth injury lawyer.
Is Your Child’s Birth Injury the Result of Medical Malpractice?
The parents of children who suffered birth injuries often want answers. They want to know what happened to harm their child.
- Did doctors choose the right type of delivery for the situation?
- Did the doctors and other medical professionals use the forceps or vacuum extractor too long or inappropriately?
- Did doctors, midwives, and nurses fail to notice signs of complications after the baby was born?
Were there signs of fetal distress that the doctors and nurses failed to recognize and/or failed to respond to in a timely manner?
Our dedicated birth injury lawyers want to help you find those answers.
We diligently investigate the facts, including a detailed examination of the fetal heart rate monitoring strips and labor and delivery records. If this review shows the medical providers did not diagnose or respond to fetal distress, we hold responsible parties accountable by pursuing medical malpractice claims against them. The compensation our clients receive helps them pay for their child’s current and future medical treatment, assistive technology and equipment, attendant care, and the other expenses associated with caring for a child with brain injuries, seizure disorders, and cerebral palsy.
Sometimes families are afraid to talk to lawyers about their child’s case because they worry there is a fee. There is never a fee unless and until we make money recovery for our clients.

Why Should You Talk with the Knowledgeable Attorneys at Miller Weisbrod?
The only way to find out if you have a birth injury case is to talk to an attorney who understands birth injury.
At Miller Weisbrod, a team of committed professionals uses our detailed case review process to assess your potential claim. They start by learning more about you and your child. Then we gather medical records to determine what happened before, during, and after your delivery. We call in skilled medical experts who review your records and let us know if they think medical errors could have caused your child’s injuries.
If we feel medical malpractice was present, we meet with you to discuss how you can receive compensation from the medical professionals who made the errors.
At no point in our legal intake process will we ask you to pay anything. The medical review of your case and the consultation are free. We only receive payment when you do.
Contact Miller Weisbrod Olesky
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.