Neonatal Infections
Infections in Newborns
A neonatal infection can put a newborn child at serious risk for birth complications, birth injuries, and even death. These risks are amplified when medical providers make preventable errors when diagnosing or treating these infections.

Free Legal Consultation
Birth Complication Lawyers
(888) 987-0005Our Birth Injury Lawyers are available to meet you in your home or the hospital.
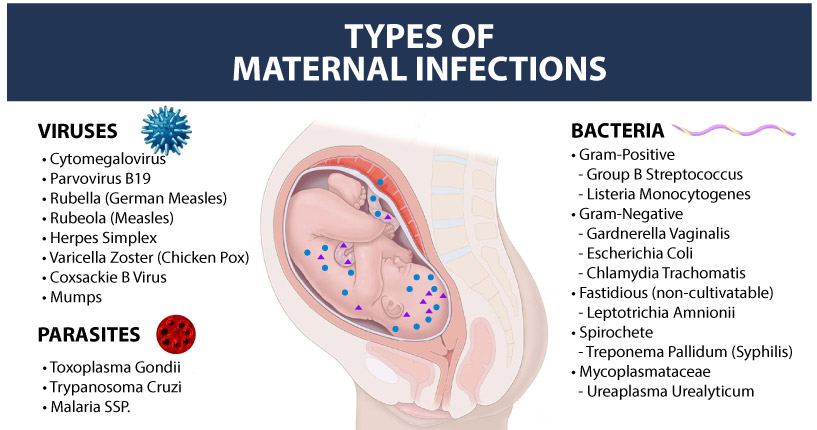
A child can contract an infection from their mother in the womb, during the process of labor and delivery, or from bacteria and viruses in the delivery room or neonatal intensive care unit (NICU). Babies born with immune system deficiencies are especially at risk for contracting infections at birth.
Neonatal infections can affect all parts of the baby’s body, including the brain. Infections like encephalitis can cause brain inflammation and threaten a child’s oxygen supply to the brain, putting them at a higher risk for hypoxic-ischemic encephalopathy (HIE) and other hypoxic brain injuries. HIE is the leading cause of cerebral palsy.
What Increases a Newborn’s Risk for Infection?
Multiple risk factors are attributed to increasing a baby’s likelihood of contracting an infection. These include:
- Premature Birth: Babies born prematurely will have a less developed immune system, weakening their abilities to fight off infections.
- Low Birth Weight: Babies with a low birth weight (possibly from prematurity or intrauterine growth restriction) will typically have weakened immune systems as well, making it more difficult for them to resist infections.
- Length of Hospital Stay: Babies with extended hospital stays in the neonatal intensive care unit (NICU) have a higher likelihood of contracting infections from unsterilized hospital equipment, interactions with other sick patients, or from contact with infected healthcare workers.
- Maternal Infections: An expecting mother with a maternal infection has a high likelihood of passing it to her child in the womb through the placenta or when she gives birth (known as a congenital infection in the child).
What Are the Most Common Infections at Birth?
Group B Strep
Group B streptococcus (Group B Strep or GBS) is one of the most common bacterial infections occurring in the genitourinary (genital and urinary) or gastrointestinal (digestive) tract. It is the most common and preventable infection transmitted to babies by their mothers.
When GBS bacteria spreads from the gastrointestinal tract to other parts of the body (such as the bloodstream), it is known as invasive Group B Strep and can have very serious effects on the newborn’s health. Babies that suffer from an untreated case of invasive Group B strep are at high risk for birth injuries, including neonatal sepsis and meningitis. A 2020 research study found that infants diagnosed with GBS were at a higher risk for cerebral palsy.

Once the baby is suspected to have a group B strep infection, they must be given immediate supportive care and urgent antibiotic administration. The “gold standard” is that the time lag between the decision to treat the baby and the actual administration of antibiotics should be no longer than one hour. This must occur even if the culture results have not come back yet from the lab to prevent serious birth complications. Not following this standard will increase the baby’s risk of harm and can constitute medical malpractice if it causes a preventable birth injury.
Encephalitis
Encephalitis is an infection that causes inflammation of the brain tissue. It is typically caused by a different bacterial or viral infection in the body. Encephalitis can have catastrophic effects for both newborns and people of all ages due to its impact on the brain.
Infected newborns can first present with flu-like symptoms, but then more serious symptoms will begin to develop, including:
- Swelling of the head
- Body stiffness
- Loss of vision or hearing
- Seizures
- Loss of consciousness (coma)
Cases of neonatal encephalitis have been linked to lifelong neurological disorders such as hypoxic-ischemic encephalopathy and cerebral palsy. Immediate treatment is required to prevent permanent brain injury and developmental delays.
Listeriosis
Listeriosis is a foodborne illness caused by the bacteria L. monocytogenes, known plainly as listeria. The CDC estimates that around 1600 people in the U.S. are infected each year, with pregnant women being at the highest risk because of their naturally suppressed immune system.
A newborn is at risk for listeriosis if their mother contracts a case while pregnant. They can acquire the infection while in the womb or during or after delivery. Doctors can perform a blood test to confirm a case of listeriosis.
If doctors suspect a pregnant woman has been infected with listeriosis, it is critical they act fast because it can cause severe harm if it spreads to her baby. A child who has been infected is at risk for multiple long term complications, including blindness, paralysis, seizures, developmental delays, or impairment to the brain, heart and kidneys.
Birth-Acquired Herpes
Congenital herpes simplex, also known as birth-acquired herpes, is a viral infection that can be transferred from the mother to her child during pregnancy. If a mother has an unhealed genital herpes outbreak during labor, it can infect the child as they pass through the vaginal cavity during delivery.
There are two main types of herpes: HSV-1, which can present as skin lesions/blisters around the eyes and mouth, or HSV-2, which affects areas on or around the genitals. For newborns, however, herpes can be identified from other symptoms outside of blistered skin, including low-grade fevers, breathing difficulties, blue appearance around the skin, or extreme irritability with high-pitched cries.
When herpes goes untreated and spreads throughout the baby’s body (known as a disseminated herpes infection), it can cause serious complications beyond just skin rashes. The infection can increase the newborn’s risk for blindness, inflammation, seizure disorders, and can even cause neonatal sepsis if the infection enters the bloodstream.
Congenital Syphilis
Congenital syphilis refers to a case of syphilis (a sexually transmitted bacterial infection) that gets passed from a pregnant woman to her child in the womb through the placenta. Severe cases can cause bone deformities, skin rashes, and nerve and brain damage in neonates.
Babies born with congenital syphilis can be treated by administering penicillin either through injections or intravenously.
Syphilis is curable and expecting mothers can be treated during pregnancy with injections of penicillin. If treated early enough, it can cure any fetal infection that has occurred as well.
Chorioamnionitis Bacterial Infection
Chorioamnionitis is an acute bacterial infection of pregnancy that enters the mother’s uterus and invades the membrane and amniotic fluid surrounding the baby. The most common bacteria causing chorioamnionitis are Group B Strep and E.coli.
Chorioamnionitis typically occurs when the amniotic sac is broken for an extended period prior to birth. This situation is known as “premature rupture of membranes” or PROM. Another typical scenario where chorioamnionitis may develop is when the mother has a prolonged or arrested labor.
A delayed diagnosis or improper management of chorioamnionitis can lead to serious birth complications, such as preterm birth, meningitis, neonatal sepsis, pneumonia, and cerebral palsy.
Neonatal Sepsis
Neonatal sepsis is a severe blood infection that is caused when a different bacterial or viral infection such as Group B Strep or chorioamnionitis enters the bloodstream. This causes inflammation and blood clotting, which can damage the child’s organs and cause serious health complications. Neonatal sepsis is one of the leading causes for infant death.
Babies born prematurely will have developed less antibodies to fight off bacteria, which puts them at a higher risk for an infection that leads to sepsis. Other high-risk groups include children with low APGAR scores and children born to a mother who has a maternal infection.
A quick response is key when treating septic newborns as untreated cases can cause organ failure, respiratory distress, neonatal meningitis, encephalitis (which can cause HIE and cerebral palsy), developmental delays, and even death. Newborns with sepsis are immediately treated using intravenous (IV) antibiotics and may be held in the neonatal intensive care unit (NICU) for multiple weeks while healthcare professionals monitor their recovery.
Neonatal Meningitis
Meningitis is an infection of the thin membranous outer covering of the brain and spinal cord. It is typically caused by another bacterial infection like Group B Strep or E. coli.

According to the National Meningitis Association, there are approximately 1,000 cases of meningitis annually, 80% of which affect infants. While meningitis affects people in all age groups, babies with less developed immune systems are particularly susceptible to developing this condition. A premature birth or low birth weight may also contribute to a newborn’s risk of infection.
When left untreated, neonatal meningitis may cause infants to lose their hearing and suffer from brain damage, cerebral palsy, hypoxic-ischemic encephalopathy (HIE), spinal cord injuries, experience seizures, and diminished mental capacity. It can also cause infants to go into sepsis if the infection travels to the bloodstream.
Medical professionals must provide optimal prenatal care to ensure a healthy delivery, especially during the third trimester. If a doctor fails to recognize and treat the infection promptly, an infected newborn will often require treatment in a neonatal intensive care unit (NICU). Resulting birth injuries from undiagnosed or untreated meningitis can affect a child's quality of life and place a substantial financial burden on the child's family.
Pneumonia
Neonatal pneumonia is an infection of the lungs, often presenting as a symptom of neonatal sepsis. It can be caused from other bacterial infections such as Group B Strep and E. coli. The premature rupturing of fetal membranes can also cause pneumonia in utero.
A pneumonia infection can put infants in a state of respiratory distress and may require them to go on a ventilator for assisted breathing treatments in the neonatal intensive care unit. Intravenous antibiotics are typically administered to fight the infection.
When left untreated, neonatal pneumonia can cause pulmonary hypertension (when the blood vessels in the lungs constrict), which can cause vascular damage and hemorrhaging. The infection can also spread into the bloodstream and into other parts of the body like the intestines, putting the newborn at risk for necrotizing enterocolitis (a rare but severe complication of neonatal pneumonia). Babies with pneumonia must be hospitalized and closely monitored to ensure that their symptoms don’t intensify.
Staph Infection
A staph infection is caused by staphylococcus aureus bacteria that gets under the skin and causes irritation and blistering. A baby can contract it through skin-to-skin contact (if the mother is infected) or from unsterilized hospital settings and equipment. A staph infection will typically present as one tender red bump on the body, but it can also manifest as a full body rash.

The primary concern with a neonatal staph infection is that it will develop into sepsis or neonatal meningitis, which are both very serious infections that can cause brain damage, cerebral palsy, developmental disabilities, and wrongful death. A mild staph infection can sometimes heal on its own, but antibiotics are usually prescribed because newborns have less developed immune systems. It can take between one to three weeks for the infection to clear up and for any blisters or skin lesions to heal.
Cytomegalovirus
Cytomegalovirus (CMV) is a viral infection that can infect people of all ages, but it can be passed through saliva or from mother to child in the womb. The CDC estimates that one in 200 babies is born with a congenital CMV infection. Babies with congenital CMV are at a higher risk for hearing loss, seizure disorders, and developmental disabilities. They may show initial signs of rash or jaundice at birth, which are common symptoms.

Once infected with CMV, the virus stays in a person’s body for life and can reactivate. But compared to most other viral and bacterial infections, the risk of long-term harm to newborns from CMV is relatively low. Most people with a CMV infection show zero signs or symptoms, and they often are unaware that they have it. Quick treatment is required for newborns, however, due to their underdeveloped immune system.
Rubella
Rubella is a viral infection that can have dangerous effects to fetal development when contracted in the womb. The infection is rare in the United States due to the prevalence of the rubella vaccine. Babies born with congenital rubella may have a rash of dark blue or purple marks on their skin or dark red patches (a type of rash known as purpura). Newborns with congenital rubella may also have a case of microcephaly (small head size) due to the infection’s effects on fetal growth in the womb.

Rubella that infects the baby in utero (especially early in the pregnancy) can increase their risk for congenital heart disease and other birth defects such as an enlarged liver or spleen, hearing loss, or developmental delays. While there is no cure for rubella, healthcare teams can develop treatment plans for an infected newborn to manage and mitigate the risk of any symptoms from it.
E. Coli
Escherichia coli (or E. Coli) is a group of bacteria that has certain toxic strains to humans (known as Shiga toxin-producing E. coli or Enterohemorrhagic E. coli). While most people likely have heard about E. Coli infection from food poisoning, it can also be passed from a pregnant woman to her child during labor.
Babies infected with E. Coli are at higher risk for developing a case of sepsis or meningitis, which can be life-threatening. They may display mild symptoms of illness beforehand such as fever, vomiting, diarrhea or jaundice. Neonatal E. coli infections can be confirmed with a blood test and are treatable with antibiotics. A timely response is required to prevent the risk of the infection traveling to the bloodstream.
Conjunctivitis
Conjunctivitis, or neonatal pinkeye, is a bacterial infection that causes inflammation of the clear membrane covering the white part of the eye (the conjunctiva). It is typically caused by another infection that is already present in the child’s body, such as group B strep or staph infection.
Symptoms include redness and swelling of the eyes and eyelids, as well as discharge from the eyes. The newborn’s eye may be tender and painful, which they may express through persistent crying or irritability. Neonatal conjunctivitis is cured with antibiotics and can clear up within 48-72 hours of treatment. The antibiotics may be administered through eye drops or intravenously if there are other infections present within the newborn.
What Are the Common Signs and Symptoms of an Infection?

Many neonatal infections often have the same or similar symptoms. Sometimes the only definitive way to diagnose an infection is with a blood test. Other tests, such as a lumbar puncture (spinal tap to test cerebrospinal fluid), may become necessary depending on the type of infection.
The most common signs and symptoms of a neonatal infection include:
Physical Symptoms
- Rashes, blisters or lesions to the skin
- Redness or discoloration of the skin
- Jaundice
- Lumps or swelling around the infected area
- Fever
- Abrupt swings in body temperature
- Difficulties with breathing
- Vomiting
- Diarrhea
- Abnormal heart rate
- Low blood sugar
Behavioral Symptoms
- Poor feeding
- Listlessness (lack of energy/drowsiness)
- Persistent crying
- Persistent irritability
- Inability to move or appearing “floppy”
If a newborn exhibits one or more of these symptoms, it may indicate an infection or other complication that warrants a hospital visit. Almost all neonatal infections can be treated with antibiotics, but some can become more severe or even fatal when treatment is delayed. This is why it is critical for doctors, nurses, and other specialized healthcare teams to be able to identify the signs and symptoms of a neonatal infection as quickly as possible.
What Does Medical Malpractice Look Like in Neonatal Infection Cases?
There are numerous medical errors that healthcare professionals must avoid when treating newborns suffering from an infection. The most common errors include:
- Failure to diagnose and treat a maternal infection prior to birth, resulting in a preventable congenital infection in the newborn.
- Insufficient sterilization of the delivery room (hospital bed, delivery instruments, scrubs, masks, gloves, etc.) that leads to a maternal or neonatal infection.
- Failure to apply antiseptic to the umbilical cord during labor and delivery, causing a bacterial infection from amniotic fluid.
- Inadequate cleaning and washing of the newborn after birth, resulting in a bacterial infection.
- Failure to identify and diagnose a neonatal infection.
- Failure to administer proper medication (eye drops, ointments, antibiotics, etc.) to a newborn after an infection, resulting in a preventable birth injury or birth complication.
- Inadequate cleaning and care after a C-section delivery, resulting in a bacterial infection.
It’s important to note that it requires a detailed review of the specific facts and timeline of a mother’s birth before making a definitive judgement as to whether medical malpractice played a factor in the child’s infection-related birth injury.
What do These Common Neonatal Infection Terms Mean?
| TERM | DEFINITION | EXAMPLES |
|---|---|---|
| Neonatal Infection | Any infection that occurs within the first 28 days of life. | Group B Strep, Cytomegalovirus, Any infection within 28 days after birth |
| Bacterial Infection | An infection caused by bacteria cells that enter the body and trigger a harmful immune response like rashes or sickness. | Group B Strep, E. coli, Meningitis, Staph Infection, Chorioamnionitis |
| Viral Infection | An infection caused by a virus that enters the body and uses the body’s cells to multiply, causing illness. | HSV (Herpes), HIV (Human Immunodeficiency Virus), Influenza, Hepatitis |
| Congenital Infection | An infection that is present at birth, passed from mother to child either in the womb or during birth. | Congenital Syphilis, Birth-Acquired Herpes, Any infection present at birth |
| Parasitic Infection | An infection caused by a parasitic organism that enters the “host” body and feeds off the nutrients from it, weakening the infected baby. | Malaria, Toxoplasmosis, Tapeworm infection, Lice |
| Fungal Infection (Mycosis) | An infection caused by a fungus, which are microscopic organisms that serve as decomposers. | Ringworm, Yeast infection, Fungal Pneumonia |
Was My Child’s Infection at Birth Mishandled?

Many common neonatal infections are easily treatable with proper medical care. Medical negligence, such as a misdiagnosis or failure to catch early symptoms an infection, or even operating errors during delivery that directly caused an infection, can worsen a newborn’s health and expose them to preventable birth injuries and complications.
If a family believes medical negligence contributed to a child’s infection-related injury, legal support may be an option. A specialized birth injury attorney can review the medical records and circumstances to assess whether a claim exists.
Parents whose children suffer from the long-term effects of birth complications, as well as parents who have suffered the loss of their baby, deserve to know whether it could have been prevented. Our dedicated birth injury lawyers want to help you find those answers and obtain the funds necessary to improve the quality of life for your child.
If your child has been diagnosed with a birth injury and you suspect this may have been caused in part by medical mistakes, Miller Weisbrod Olesky will thoroughly investigate the facts and hold the responsible medical providers accountable by pursuing medical malpractice claims against them.
Sometimes families are hesitant to reach out to a medical malpractice attorney or law firm. They may feel overwhelmed by their circumstances or are worried that a law firm will not be able to help them. But the only way to find out if you have a case is to talk to an attorney who understands how birth injuries can lead to developmental delays and other complications that require long-lasting medical support.
What Is the Statute of Limitations in a Birth Injury Lawsuit?
A statute of limitations (SOL) is a law that sets a time limit on how long an injured person has to file a lawsuit after an accident. It is essential to understand that statutes of limitations vary based on the type of case and the state where it is filed. For instance, the deadline for birth injury claims is typically different from other claims, such as injury to personal property, fraud, contract disputes, and collection of debts.
Generally, the clock starts ticking on the date the injury occurred. However, there are exceptions to this rule, and in some cases, the statute of limitations starts when a person discovers or reasonably should have discovered an injury. When dealing with government agencies, SOLs can become even more complex.
For example, if the party that injured you was:
- A federal employee
- Employed by a military hospital, Veterans Administration facility, or a federally funded medical entity
You may need to file a birth injury claim under the Federal Tort Claims Act (FTCA). In FTCA cases, claimants must go through certain administrative procedures before filing a lawsuit. In some states, if the negligent party was a local or state government hospital or the doctors and medical providers are employees of a governmental entity, the time period in which you must give "notice" may be shorter.
If your case is filed outside of the statute of limitations, it will typically be dismissed, and you will not be eligible to recover compensation for your injuries. Determining when a statute of limitations begins on your case can be tricky. If you're considering pursuing compensation for a birth injury, contacting an attorney as soon as possible is in your best interest.
How The Birth Injury Attorneys at Miller Weisbrod Olesky Can Help

Birth injuries that trace back to a neonatal infection can be prevented in many cases, but it takes a detailed expert review of the facts and circumstances of your pregnancy and your child's birth to determine whether the injury was the result of medical malpractice.
Our Process
At Miller Weisbrod Olesky, a team of committed birth injury malpractice attorneys, nurses and paraprofessionals uses our detailed medical negligence case review process to assess your potential birth injury case. We start by learning more about you and your child and the status of meeting/missing developmental milestones. Then we gather medical records to determine what happened before, during, and after your delivery. We call in skilled medical experts who review your records and let us know if they think medical errors could have caused you or your child's injuries.
If we feel medical negligence caused or contributed to complications with your pregnancy or your child's injuries, we meet with you to discuss how you can receive compensation from the medical professionals who made the errors.
At no point in our legal intake process will we ask you to pay anything. The medical review of your case and the consultation are free. We only receive payment when you do. The sooner you reach out to us, the sooner we can begin investigating your case and gathering the evidence needed to support your claim.
We work on a contingency fee basis, meaning you won't pay any legal fees unless we win your case. Contact us today to schedule your free consultation by calling our toll-free line at (888) 987-0005 or by filling out our online request form.
Contact Miller Weisbrod Olesky
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.