Umbilical Cord Problems
Types of Umbilical Cord Complications
Umbilical cord complications can endanger a baby’s life, especially if medical providers fail to catch them in time.

Attached to the placenta in the mother’s uterus, the umbilical cord acts as the baby’s lifeline during pregnancy. It is the vessel by which blood, oxygen, and other nutrients travel from the mother to the baby.
When umbilical cord complications disrupt this flow of nutrients, it puts the baby at risk for developing serious birth complications. Disruptions in oxygenated blood flow can cause hypoxic (lack of oxygen) and ischemic (lack of blood flow) brain injuries. The most common form of brain damage at birth from umbilical cord problems is hypoxic ischemic encephalopathy (HIE).
Neonatal Hypoxic Ischemic Encephalopathy
Hypoxic ischemic encephalopathy is the most common brain injury in newborns. It occurs when the baby lacks sufficient levels of oxygen and blood flowing to their brain.
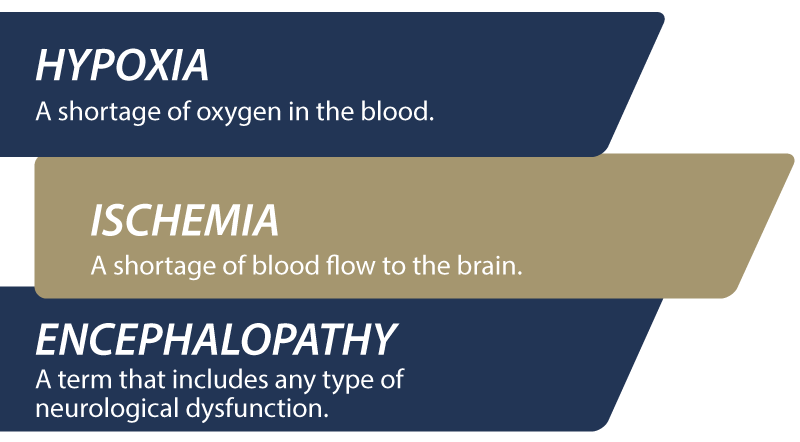
HIE injuries are permanent and can lead to seizure disorders, vision impairments, and developmental delays. It is also the leading cause of cerebral palsy in young children.
The umbilical cord plays a critical role in delivering both oxygen and blood to the newborn. Complications like knots, compression, or nuchal cord can cause HIE when they restrict oxygenated blood flow for too long.
Medical providers must understand how umbilical cord complications occur, how to treat them, and how to prevent them. If they fail to do this, babies may suffer from severe birth injuries like HIE that permanently impact their lives. When preventable medical errors cause lifelong injuries and limitations, it counts as medical malpractice.
Birth Injury Malpractice Attorneys
Our top rated birth injury attorneys specialize in identifying how umbilical cord problems can cause or worsen a child’s birth injuries. If you or someone you know suffered from the effects of mismanaged cord complications, don’t hesitate to contact our firm. We can answer difficult legal and medical questions and investigate the facts on your behalf.
Free Legal Consultation
Birth Injury Lawyers
(888) 987-0005Our Birth Injury Lawyers are available to meet you in your home or the hospital.
Our vast network of medical experts and in-house nursing staff and nurse-attorneys gives us the edge over our competition. When we take your case, we assign you with an entire medical team. This team not only consists of attorneys but also nursing advocates and medical experts.
Your team is available to assist with any day-to-day treatment you or your child may need. This includes assistance with medical records, scheduling doctors’ appointments, providing transportation, and any other problems that may arise.
We offer all of this on a contingency fee basis. This means you will not pay any fees until after we win your case and secure a settlement. Miller Weisbrod Olesky’s unmatched track record of birth injury results sets us apart from other birth injury law firms.

Recent Birth Injury Settlement:
Birth Injury settlement against a hospital in which nurses and physicians failed to properly monitor the mother's blood pressure during delivery causing an HIE event resulting in neonatal seizures and cerebral palsy at birth. Our team of top-rated birth injury lawyers recovered $13,750,000 for the family to help with future medical expenses and developmental therapy.
What Does the Umbilical Cord Do?
Most of the umbilical cord interior consists of a gel-like connective tissue called Wharton’s jelly. This jelly protects and surrounds two umbilical arteries and a large umbilical vein.

The umbilical cord does not actually connect the baby directly to their mother. Instead, the placenta acts as a sort of middle messenger. The placenta takes in nutrients from the mother and then supplies it to the unborn child via the umbilical cord.
Oxygenated blood flows through the umbilical vein from the placenta to the child. After passing through the baby, the umbilical arteries carry out deoxygenated blood (blood containing carbon dioxide) back to the placenta. After they’re born, most babies have a respiratory system that’s developed enough for them to breathe on their own.
Doctors, midwives, nurses, and other healthcare professionals should be aware of potential umbilical cord complications. They must be familiar with them so they can quickly and accurately diagnose an issue and provide treatment.
When medical professionals are unaware of common umbilical cord problems, it’s easier for them to miss the signs. Delayed treatment can mean the difference between life and death for an unborn baby in fetal distress.
What Are Common Umbilical Cord Complications?
Most umbilical cord complications involve one of three factors:
- Length (a cord that’s either too long or too short)
- Positioning (a cord with knots, compression, or one that’s wrapped around the baby’s neck)
- Placental Insertion (a cord that’s only partially attached to the placenta, or not attached at all)
Other issues like vasa previa and umbilical cord infection can also complicate a mother’s pregnancy and the delivery.
Doctors can identify most umbilical cord problems during prenatal testing appointments, giving them time to prepare and plan. However, some complications occur during labor and delivery. In these cases, labor and delivery medical teams must detect and address problems immediately to prevent irreparable damage.
Some umbilical cord complications will prevent the child from safely exiting through the mother’s birth canal. When this happens, doctors must prepare to perform an emergency c-section or use external tools like forceps and vacuum extractors.
Nuchal Cord
A nuchal cord is an umbilical cord that wraps around the baby’s neck. This complication is fairly common, occurring in between 20% and 30% of all pregnancies.

A nuchal cord can develop from a baby’s increased movement and turning while in utero. Certain factors like a mother’s low blood sugar or excess amniotic fluid in the womb can increase her baby’s movement. As the child turns, spins, and flips around, they can inadvertently wrap the umbilical cord around their neck.
In many nuchal cord cases, the cord is loose enough for the baby to slip out of naturally. Sometimes the doctor can even unwrap it themselves during delivery. But more serious cases of nuchal cord can cut off blood flow to the child’s brain.
When doctors identify a nuchal cord complication before labor, they must closely monitor the unborn baby’s heart rate. They can do this using electronic fetal heart rate monitors or nonstress tests (NSTs).
Abnormal fetal heart rates can indicate the baby is in fetal distress. If this happens, doctors may need to perform an emergency cesarean section delivery (C-section) to prevent brain damage at birth.
Short Umbilical Cord
A typical umbilical cord in a full-term infant is about 20 inches long and 0.75 inches in diameter.
Cords that are 14 inches or shorter can increase the risk of dangerous labor and delivery complications. Excessive fetal movement with short cords can pull too hard on the mother’s placenta, increasing her risk for placental abruption. It can also put the umbilical cord at risk of tearing or rupturing, which would have catastrophic effects. Tears to the umbilical cord or the placenta can cause internal bleeding and put the mother’s life at risk.
Research suggests that babies with short umbilical cords are more likely to require a C-section delivery. They are also more at risk for fetal distress, birth asphyxia, hypoxic ischemic encephalopathy, low Apgar scores, and NICU admission.
Long Umbilical Cord
Cords measuring more than 80 centimeters (roughly 31.5 inches) are unusually long. Doctors will normally first observe a long cord through ultrasounds during scheduled prenatal testing checkups.
An abnormally long cord doesn’t inherently harm the child. But it can sometimes increase the risk for other umbilical cord complications. A baby is more likely to wrap a longer umbilical cord around their neck while moving in the womb. Longer cords also increase the risk of umbilical cord prolapse (when the cord exits the birth canal before the baby).
Doctors, nurses, and other healthcare providers must be aware of the risks a long umbilical cord can pose. They must anticipate complications and prepare to intervene should the cord cause any complications during the mother’s delivery.
True Knot
As the name implies, this umbilical cord complication involves knots that form on the baby’s umbilical cord. Doctors should carefully review ultrasounds to check for knots. However, some knots develop during labor and delivery.
An umbilical cord true knot can form from the baby’s natural movement and repositioning within the womb. But other factors can increase the risk of one forming, including polyhydramnios, a gestational diabetes diagnosis, or unusually long cords.
True knots can be dangerous to the baby. The knot can compress the blood vessels in the cord, compromising the baby’s supply of blood, oxygen, and nutrients. Depending on the timing, this can result in poor fetal development (intrauterine growth restriction), fetal distress, and brain injuries.
A decrease in fetal activity and movement can be a sign of a true knot in the baby’s umbilical cord. Medical professionals must actively monitor the child’s heart rate in the critical weeks leading up to the mother’s due date. In some cases, true knots that block the flow of oxygenated blood and nutrients can require an emergency c-section delivery.
Umbilical Cord Prolapse
Normally, the baby exits the womb before or with the umbilical cord. Complications arise when one or more loops of the cord slip through the cervix before the baby. The prolapse often completely compresses the cord, which reduces or stops the flow of blood and oxygen to the baby.

When this happens, doctors, nurses, and midwives need to consider it an obstetrical emergency and take immediate action. Failing to perform an emergency C-section could damage the baby’s brain or even be fatal.
Umbilical Cord Compression

A mother’s uterine contractions during labor will naturally and temporarily compress the umbilical cord. However, when compression goes on too long, the baby’s heart rate may exhibit signs of fetal distress and birth trauma.
Umbilical cord compression is a serious complication, whether it happens before or during childbirth. The blood, oxygen, and nutrients flowing through the cord are essential to the baby’s development and wellbeing.
Sometimes another existing umbilical cord complication can cause compression. This includes problems like a true knot, a nuchal cord, or a prolapsed umbilical cord during labor.
Doctors and nurses reading fetal monitors should recognize the signs of umbilical cord compression and intervene immediately. If intervention does not quickly decrease compression, the mother may need an emergency C-section.
Marginal Cord Insertion
Normally, the umbilical cord attaches to the center of the placenta. This is the thickest and most secure spot for attachment.
Marginal cord insertion (MCI) is an abnormal type of cord insertion where the umbilical cord attaches to the edges of the placenta. The placenta’s edges are thinner and can slow the delivery of vital nutrients.
Marginal cord insertion can stunt a child’s growth if it blocks them from receiving sufficient blood, oxygen, and nutrients. This will increase their risk for complications like low birth weight and difficulties with breathing.
Velamentous Cord Insertion
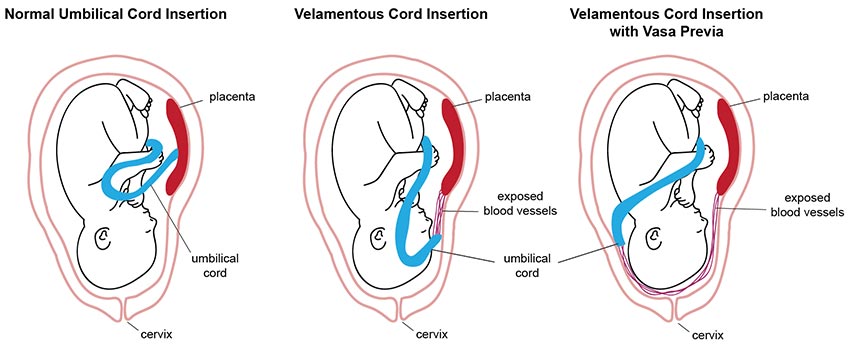
In rare cases, the umbilical cord doesn’t insert into the placenta at all. Instead, it inserts directly into the fetal membranes outside of the placenta. This is an umbilical cord abnormality called velamentous cord insertion (VCI).
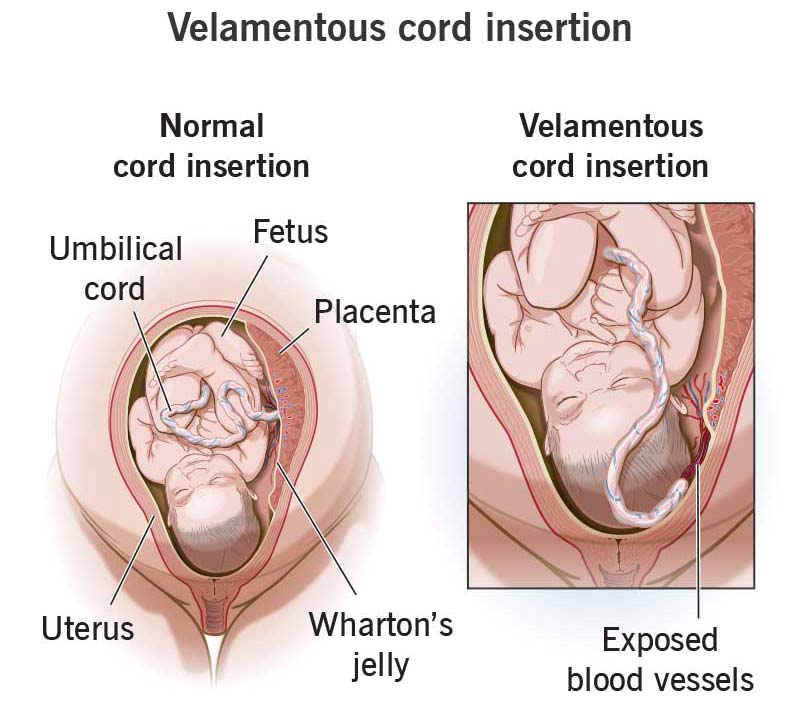
While rare, velamentous cord insertion is more common in twin pregnancies, especially monochorionic diamniotic twins (twins sharing the same placenta). Other risk factors include in vitro fertilization and placenta previa (where the placenta attaches lower than regular in the uterus).
Velamentous cord insertion forces blood vessels to travel much farther without the protection of Wharton’s jelly. Exposed umbilical cord blood vessels are more likely to burst and bleed, harming both the mother and her baby.
In some cases of velamentous cord insertion, a doctor may deem it necessary to conduct a planned emergency c-section. They make this decision when they suspect injury to the cord or the baby to be likely.
Vasa Previa
Vasa previa is a pregnancy complication where one or more of the umbilical cord blood vessels exists outside the cord. The exposed blood vessels are either run or are close to running across the mother’s cervical opening. Velamentous cord insertion is a common risk factor for vasa previa.

The main concern with vasa previa is that these exposed vessels could rupture, especially when the mother’s water breaks. This can cause severe internal hemorrhaging for the mother and blood loss for the baby, which can result in death.
Doctors can identify vasa previa during regular prenatal testing ultrasounds and before labor commences. If they fail to detect or ignore the complication, it can result in fetal distress or infant wrongful death.
Umbilical Cord Infections

Intrauterine infections like chorioamnionitis affect a pregnant woman’s placenta. The infection can disrupt the baby’s supply of oxygen and nutrients, damaging their heart, lungs, brain, and other organs.
Additionally, the umbilical cord can contract an infection known as funisitis. This typically occurs after infected fetal membranes spread to the umbilical cord. Umbilical vasculitis is an infection of the cord blood vessels. This is typically the same bacteria responsible for other common maternal infections (Group B strep, listeria, etc.).
These types of umbilical cord infections can cause fetal distress and increase the risk of brain injuries like HIE.
How to Diagnose Umbilical Cord Complications?

Doctors and medical providers can use ultrasound to diagnose many conditions affecting the umbilical cord. When caught early, medical intervention could prevent a minor issue from becoming a life-threatening complication.
Prenatal monitoring of the fetal heart rate is also important. Abnormal fetal heart monitor results can indicate an unborn baby is suffering hypoxia (reduced oxygen) or birth asphyxia (oxygen cutoff).

Medical staff routinely attach two electronic fetal monitors to the mother during labor and delivery. One monitors the mother’s contractions. The other monitor tracks the baby’s heart rate, especially when reacting to contractions. A decreased heart rate could indicate cord compression or other umbilical cord complications. Additionally, unusually long contractions or too many contractions over a given time (hyperstimulation) can cause cord compression and hypoxia.
A doctor should be able to detect prolapsed umbilical cords when conducting physical examinations of the mother during labor.
Failing to monitor mothers undergoing labor and delivery is medical negligence, especially when signs of umbilical complication are present. A top rated birth injury lawyer can help families who experienced medical negligence explore potential medical malpractice claims.
Can Doctors Fix Umbilical Cord Problems in Utero?
Doctors will only be able to keep an eye on some complications, like a known nuchal cord or vasa previa. For these complications, they will only be able to act in emergency situations by delivering the baby.

Doctors can treat infections as soon as they identify them by prescribing and administering antibiotic or antiviral medications. They must carefully monitor the mother for any adverse reactions while administering these medications.
When a baby is in fetal distress from umbilical cord compression, doctors and nurses can try changing the mother’s position. They should then analyze electronic fetal monitor results to see if the baby’s heart rate has recovered. If not, they must move forward with more critical treatment.
An emergency C-sectionis necessary in some situations, including umbilical cord prolapse and extreme prolonged compression. Otherwise, the baby could suffer from hypoxic-ischemic encephalopathy due to the lack of oxygenated blood flow to their brain.
Where Medical Providers Go Wrong
Proper medical care begins with regular prenatal testing visits. During these visits, medical professionals should inquire about and log the expecting mother’s complete medical history.

Blood and urine testing can give healthcare providers a clearer picture of the mother’s health. Ultrasounds help identify potential problems with the unborn baby. Additional tests may be necessary when umbilical cord complications or other pregnancy complications are possible.
Doctors can catch some umbilical cord complications early. After detection, doctors should monitor at-risk mothers and babies more closely. Otherwise, life-threatening situations could arise that cause brain damage, cerebral palsy, developmental delays, and seizure disorders.
Finally, umbilical cord issues may arise during labor and delivery. Medical professionals must closely observe their patients and meet their duty of care to recognize and respond to fetal distress.
Possible examples of medical malpractice regarding umbilical cord complications include:
- Failing to conduct adequate prenatal checkups and missing an umbilical cord complication.
- Failing to recognize an umbilical cord complication as a threat, leading to further injury to the mother or her child.
- Delaying or failing to conduct an emergency c-section in the event of an umbilical cord complication during labor and delivery.
- Injuring the mother or her child with forceps and vacuum extractors in the event of an umbilical cord complication during delivery.
Did Doctors Mismanage My Umbilical Cord Problem?

Umbilical cord complications can cause devastating birth injuries like HIE that permanently alter a child’s life trajectory. Birth injury negligence can make these tragic outcomes more likely.
If a family believes medical negligence caused or worsened a child’s injuries, legal support may be an option. A specialized birth injury attorney can review the medical records and circumstances to assess whether a claim exists.
Families who have experienced the effects of brain injuries from umbilical cord complications deserve to know whether they were avoidable. Our top rated birth injury lawyers will help you find those answers and obtain the necessary funds to secure treatment.
Our team at Miller Weisbrod Olesky will thoroughly investigate the facts, holding responsible parties accountable by pursuing medical malpractice claims.
What is the Statute of Limitations in a Birth Injury Lawsuit?
A statute of limitations (SOL) is a law that sets a time limit on how long an injured person has to file a lawsuit after an accident. It is essential to understand that statutes of limitations vary based on the case and the state where you file. For instance, the deadline for birth injury claims is typically different from other claims, such as injury to private property.
Generally, the clock starts ticking on the date the injury occurred. However, there are exceptions to this rule. In some cases, the statute of limitations starts when a person discovers or reasonably should have discovered an injury. When dealing with government agencies, SOLs can become even more complex.
For example, if the party that injured you was:
- A federal employee
- Employed by a military hospital, Veterans Administration facility, or a federally funded medical entity
You may need to file a birth injury claim under the Federal Tort Claims Act (FTCA). In FTCA cases, claimants must go through certain administrative procedures before filing a lawsuit.
In some states, you may have less time to give notice if:
- The negligent party was a local or state government hospital.
- The doctors and medical providers are employees of a governmental entity.
If you file your case outside of the statute of limitations, the court will typically dismiss it. This means you will not be eligible to recover compensation for you or your child’s injuries.
Determining when a statute of limitations begins on your case can be tricky. If you are considering pursuing compensation for a birth injury, contact an attorney as soon as possible.
How Can Our Birth Injury Attorneys Help?

Umbilical cord problems do not always result in birth injuries. Many negative consequences of umbilical cord complications are preventable with proper medical care. However, it takes an expert review of the facts of your birth to determine whether medical professionals made preventable errors.
Our Process
Our team of committed birth injury attorneys, nurses and paraprofessionals works to answer these questions and seek compensation. We use our detailed medical negligence case review process to assess your potential birth injury case.
We start by learning more about your pregnancy by gathering records to determine what happened during and after your delivery. This includes a detailed review of the treatment doctors provided or failed to provide during prenatal testing appointments.
We will call in skilled medical experts who review your records and provide insight into where medical professionals went wrong. If we feel medical negligence caused or worsened your umbilical cord complication, we meet with you to discuss further.
At no point in our legal intake process will we ask you to pay anything. The medical review of your case and the consultation are free. We only receive payment once you do. The sooner you reach out, the sooner we can investigate your case and gather the evidence to support your claim.
We work on a contingency fee basis, meaning you will not pay any legal fees until we win your case. We do not purse any medical malpractice cases unless we fully believe we can win.
Contact us today to schedule your free consultation by calling our toll-free line at (888) 987-0005. You can also reach us by filling out our online request form.
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.