Brachial Plexus (Erbs Palsy)
Brachial Plexus Commonly Known as Erb's Palsy
Birth injuries can profoundly shape a child's future, impacting their ability to enjoy independent and fulfilling lives. One of the most serious and common types of birth injuries that newborns may suffer during childbirth is a type of brachial plexus injury known as Erb's palsy.

The brachial plexus is a complex network of nerves that extends from the neck across the shoulder to the arms and hands. If these nerves are stretched or torn during childbirth, it can cause a newborn to suffer several debilitating medical conditions, that result in a lifetime of disability. Erb's palsy is a condition that results from birth trauma damage to this network of nerves, and in its most severe form, it can leave the affected infant's arm, elbow, and hand completely immobile.
Erb's palsy and other brachial plexus birth injuries during childbirth often result from preventable mistakes made by obstetricians and/or other medical professionals during childbirth. If your child has suffered a birth injury during childbirth and you suspect that medical negligence may be to blame, it is crucial to consult with one of our dedicated birth injury malpractice attorneys at Miller Weisbrod Olesky. We are committed to fighting for your child's rights and securing the maximum compensation your family deserves.
Free Consultation
National Birth Injury Lawyers
(888) 987-0005
What is Brachial Plexus (Erb's Palsy)?
The brachial plexus is a set of nerves that passes from the spinal cord through the neck's vertebrae and into the arm. This complex network of nerves is composed of four cervical nerve roots (C5-C8) and the first thoracic nerve root (T1). These roots merge to form three trunks:
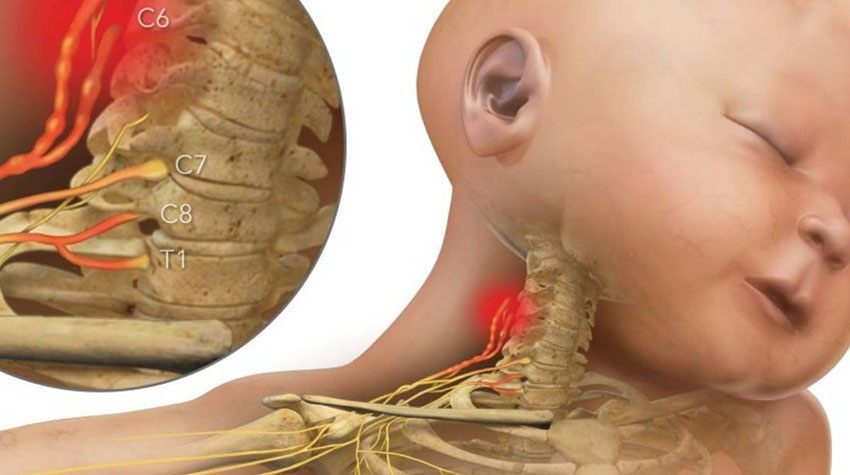
- Upper Trunk (C5, C6)
- Middle Trunk (C7)
- Lower Trunk (C8, T1)
Each trunk splits into divisions, with one-half responsible for flexor muscles (those that lift and bend the arm) and the other half for extensor muscles (those that straighten the arm and bring it down). These nerves are responsible for providing feeling and controlling movement in the shoulders, arms, hands, and fingers.
During an especially difficult delivery, these nerves can be compressed from birth trauma, becoming stretched, or torn away from the spinal cord. When these nerves are damaged, it can cause a range of physical impairments, including weakness, numbness, and paralysis in the affected limb in severe cases. Brachial plexus birth injuries are particularly common in newborns, occurring in approximately 1 to 2 out of every 1,000 births.
In most cases, brachial plexus injuries heal on their own within the first few months of a newborn's life; however, for more involved injuries, physical therapy or even surgery may be required. Physical therapy and surgery play a significant role in the treatment of brachial plexus injuries, providing hope and a potential path to recovery for affected families.
Generally, brachial plexus injury at birth takes one of two forms. Erb's palsy is the most common form of brachial plexus injury caused by damage to the C5 and C6 nerves. Injuries to the upper nerves in the brachial plexus affect the muscles of the shoulder and upper arm.
The birth complications associated with Erb's palsy may include weakness or numbness in specific muscles of the arm or shoulder, stiff joints, and inability to flex the elbow or lift an arm. Depending on the extent and location of the nerve damage, an infant with Erb's palsy may experience partial or complete paralysis in the affected shoulder and upper arm.
The second, less common form of brachial plexus injury is Dejerine-Klumpke (Klumpke's) palsy. This injury occurs as a result of damage to the lower brachial plexus, specifically the C8 and T1 nerves. In infants with Klumpke's palsy, symptoms may include difficulty with gripping objects, a reduced ability to move their fingers, or even a "claw hand" deformity, where the fingers remain bent due to muscle weakness.

Damage to all five brachial plexus nerves (C5, C6, C7, C8, and T1) is called global palsy. Infants with global palsy may experience complete paralysis and loss of sensation in the entire arm, extending from the shoulder to the hand.
Four Types of Brachial Plexus Nerve Injuries
Brachial plexus injuries that occur at birth are often classified based on the type of nerve damage and the specific nerves that are affected. These injuries can vary in severity, from mild stretching of the nerves that heals naturally to more severe damage that requires medical intervention. Understanding the type of nerve injury is essential for healthcare providers to determine the appropriate treatment plan and predicting the potential for recovery.
The four types of brachial plexus nerve injuries are:
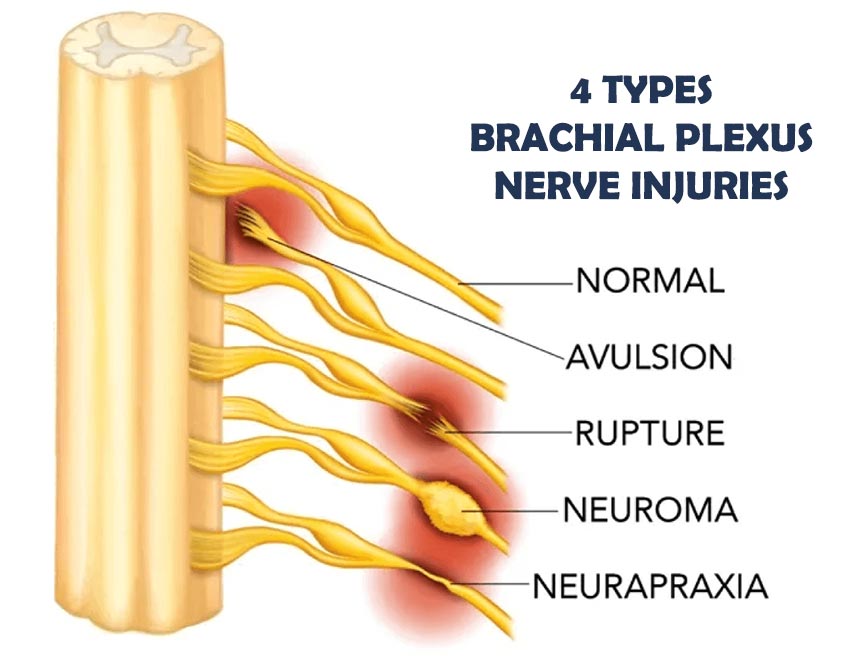
Neurapraxia (Stretch Injury)
Neurapraxia, the most common and least severe form of brachial plexus injury, offers hope for recovery. It occurs when the nerve is stretched but not torn, often due to excessive pulling or stretching during delivery. While this can disrupt the normal transmission of electrical signals along the nerve, leading to weakness, numbness, or limited movement in the affected arm or shoulder, the nerve fibers remain intact.
Fortunately, neurapraxia is often temporary, and most infants recover completely without needing surgery within 3 to 6 months. In many cases, physical therapy can support the recovery process by helping to improve strength, range of motion, and coordination in the affected limb.
Neuroma

A condition that typically occurs after a nerve, such as through overstretching, tearing, or surgical trauma is damaged and as the body attempts to repair the damage, it forms scar tissue (Neuroma) around the affected nerve. While this is a natural part of the healing process, the buildup of scar tissue can prevent the regrowth of nerve fibers. This scar tissue can also exert pressure on the surrounding healthy nerve fibers, disrupting their ability to send signals to the muscles.
In some cases, the scar tissue may form a painful mass or knot on one of the brachial plexus nerves. Treatment for neuromas often involves surgical intervention to remove the scar tissue and reduce pressure on the surrounding nerves. To prevent the formation of another neuroma, the surgeon may either cap the nerve or attach it to another nerve. Capping the nerve involves covering the exposed end to protect it from further injury. In some instances, nerve grafts or transfers may be used to reconnect the affected nerve to healthy nerves, promoting the growth of new fibers and reducing the risk of further scar tissue formation.
Rupture

A Brachial Plexus Rupture occurs when the nerve is subjected to a more forceful stretch, causing it to tear either partially or completely. In these types of injuries, the nerve is torn but not where it attaches to the spinal cord. Instead, the injury typically occurs outside the spinal cord, in the area between the nerve root and its peripheral branches.
Depending on the severity and location of the rupture, it can cause weakness in the shoulder, arm, or hand, and may even result in the loss of function in certain muscles. A rupture will not heal on its own. However, surgery may be required to repair the damaged nerve.
Surgical options often involve nerve grafts or nerve transfers, where healthy nerve tissue bridges the gap and restores the connection between the injured nerve and the muscles it controls. In some cases, surgeons may also use a nerve from another part of the body to replace the damaged one. While surgery can significantly improve outcomes, its success depends on factors such as the extent of the nerve damage and the timing of the surgery.
Avulsion

This is the most severe form of brachial plexus injury that occurs when the nerve is completely torn away from its connection to the spinal cord. Compared to other types of brachial plexus nerve injuries, avulsions are relatively rare accounting for only about 10 to 20% of all cases. These injuries are typically caused by motorcycle or car accidents and can lead to permanent weakness, paralysis, and loss of feeling in the affected arm, hand, or shoulder. In addition to functional impairments, Brachial Plexus Avulsion injuries can cause a range of other complications. For example, damage to the nerve roots that control the diaphragm can lead to respiratory issues.
Additionally, damage to the sympathetic nerves may result in Horner's Syndrome, a condition that causes symptoms such as drooping eyelids and constricted pupils. Unlike a nerve rupture, it is not possible to repair an avulsion from the spinal cord directly. Instead, restoring some function in the affected limb may be possible by surgically replacing (nerve transfer) the detached nerve with a healthy nerve from another part of the body. Even with surgery, avulsion injuries may result in permanent impairments that require long-term management and rehabilitation.
Birth-related brachial plexus injuries can occur at the same time in the same infant and affect one or more (sometimes all four) of the nerves. While symptoms like loss of feeling and paralysis are common across all types of nerve injury, the severity of these symptoms and the potential for recovery vary greatly depending on the type and extent of the injury.
For example, less severe injuries, like neurapraxia, often resolve on their own over time, and many infants regain full function within a few months. However, more severe injuries, such as ruptures or avulsions, can result in permanent loss of function and require surgical intervention to help restore some level of functionality in the affected limb. Ultimately, with early diagnosis, timely intervention, and support many infants can experience significant improvements in their motor skills, strength, and overall quality of life.
Risk Factors Brachial Plexus Injuries
Understanding the risk factors that can increase the likelihood of a newborn suffering from Erb's palsy or other brachial plexus injuries can assist healthcare providers in anticipating potential birth complications and taking the necessary steps to reduce the risk of nerve damage. While some risk factors are unavoidable, others can be managed or mitigated with proper prenatal care and fetal monitoring during delivery.
Some of the most common risk factors for brachial plexus injuries include:
- Shoulder Dystocia
- Large Baby (Macrosomia)
- Breech Presentation
- Prolonged Labor
- Maternal Obesity
- Gestational Diabetes
- Uterine tachysystole
- Cephalopelvic disproportion (CPD)
- Multiple Births (Twins or More)
- A previous delivery with a brachial plexus injury
- Misuse of birth-aiding tools like vacuum extractors or forceps
- Improper use of labor-inducing medications
When a doctor or other medical professional fails to adhere to the appropriate standard of care during childbirth and it results in preventable harm to a newborn, the consequences can be devastating. In these cases, parents and caregivers of the birth-injured infant have the right to seek compensation for ongoing medical expenses, therapy or treatment costs, and compensation for pain and suffering. A skilled birth injury attorney can help families secure the justice and resources they need to provide the best possible care for their child's recovery and quality of life.
Signs and Symptoms of Brachial Plexus Injuries
Since newborns are unable to verbally communicate their pain or discomfort, it is up to their parents to recognize signs of a brachial plexus injury, like Erb's palsy. While some symptoms may resolve on their own, others may require medical intervention to prevent long-term complications and promote the best possible recovery.
Identifying these symptoms early can lead to a more accurate diagnosis and help healthcare providers tailor an effective treatment plan that meets your child's specific needs.

If you suspect that your child may have Erb's palsy or another brachial plexus injury, the following are some common signs and symptoms you should be on the lookout for.
- Weakness or numbness in the affected arm
- An arm that hangs limply or is oddly twisted
- Decreased grip strength in the affected hand
- Partial or complete paralysis of the arm
- Impaired circulation in the affected arm
- Limited range of motion in the shoulder, elbow, wrist, or hand
- Pain or discomfort when the affected arm is touched or moved
- Facial paralysis on the same side as the affected limb
- Lack of control over certain muscles in the arm, shoulder, or hand
- Difficulty reaching developmental milestones, such as crawling or sitting up unassisted
Symptoms of brachial plexus injuries, including weakness or limited movement in the affected arm or hand can significantly impact a child's ability to perform basic tasks like grasping objects or feeding themselves. Moreover, a restricted range of motion in the affected arm can delay the development of essential gross motor skills, such as crawling, sitting up, and standing on their own.

In cases of Erb's palsy caused by a difficult delivery, the signs and symptoms are typically easy to identify. The affected arm will typically hang limp from the infant's shoulder and be noticeably smaller than the unaffected arm. Nerve damage is responsible for slowing the growth of muscles and bones in the affected arm and creating a size difference that will become more noticeable as the child ages.
This disparity can also make it more difficult for the child to reach the necessary milestones to achieve greater independence and improve their quality of life. If you believe your newborn may have suffered a brachial plexus injury, you should consult with a healthcare provider as soon as possible for an accurate diagnosis.
Diagnosing and Treating Brachial Plexus Injuries
Erb's palsy and other brachial plexus nerve injuries are typically diagnosed by a pediatrician who will conduct a physical examination, evaluate the baby's medical history, and assess whether there are any signs of weakness or loss of movement in the affected arm. Your child's doctor may also order an X-ray, ultrasound, or other imaging test, such as a magnetic resonance imaging (MRI) scan, to evaluate any potential damage to the bones, joints, or soft tissues in the neck and shoulder.

In some cases, the pediatrician may also order additional tests like Electromyography (EMG) or nerve conduction studies (NCS) to assess the severity of the injury and guide treatment decisions. A nerve conduction study measures how well electrical impulses travel through the nerves and helps doctors determine if and where nerve damage may have occurred. An EMG, on the other hand, records electrical activity in the muscles and provides important information about whether the muscles are receiving signals from the nerves.
Since most babies with a brachial plexus injury begin to show signs of recovery within the first month to six weeks after birth, the doctor will carefully monitor your baby's progress during this period and schedule follow-up visits. If your child's recovery is progressing as expected, no immediate intervention may be necessary; however, if your baby is not showing signs of improvement. The pediatrician may refer you to a pediatric orthopedist or a brachial plexus specialist for further evaluation and treatment.
Treatment Options for Erbs Palsy and Other Brachial Plexus Injuries
While the majority of brachial plexus injuries like Erb's palsy heal on their own, approximately 10% lead to lifelong conditions and permanent disabilities. An essential part of keeping the child's affected joints, tendons, and muscles limber is having them participate in physical therapy.

Therapy should be done as often as possible during the day and begin as early as 3 weeks after delivery. Range of motion exercises (ROM) and gentle stretching can help restore strength, flexibility, and range of motion to the damaged areas. Because babies cannot move their affected arm on their own, parents/caretakers must take an active role in performing this exercise at home with their child and ensuring their joints and muscles are moving frequently.
Botox injections are another non-surgical treatment option that has proven beneficial to some children with Erb's palsy. This treatment works by temporarily blocking certain nerve signals that cause muscle contraction, helping to relax overactive muscles and reduce muscle spasticity. Although Botox is not a permanent solution, it can improve the child's ability to participate in rehabilitation exercises and reduce the discomfort caused by muscle tightness.
If physical therapy or other non-surgical treatments do not lead to an improvement in symptoms over the first 3 to 6 months of a child's life, surgery may be necessary.
Depending on the severity of the injury, a doctor may recommend one or more of the following procedures:
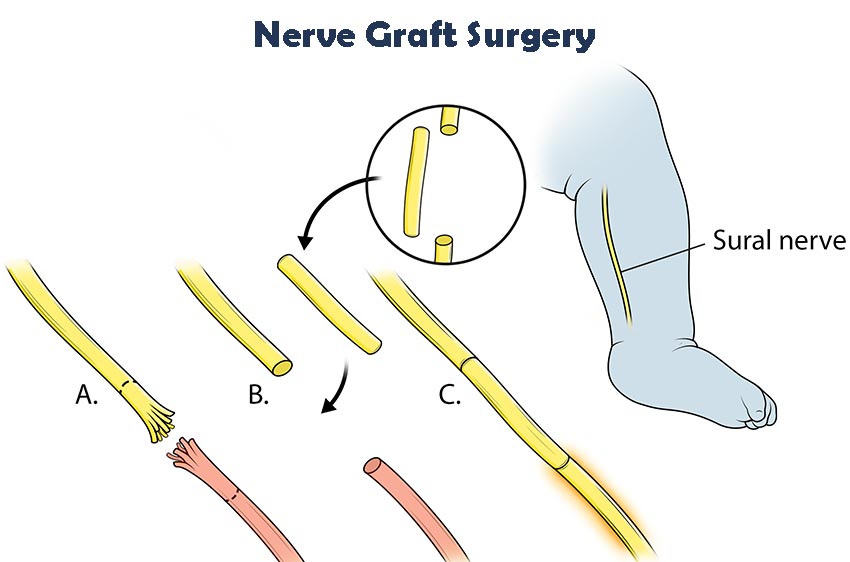
Microsurgery, or nerve surgery, is the first type of surgery recommended by doctors for children with Erb's palsy when recovery remains insufficient after 6 months. In microsurgery, surgeons often use high-powered microscopes and specialized instruments to repairs or reconstruct injured nerves. In treating Erb's palsy, microsurgery typically consists of a combination of nerve grafting and nerve transfer.
- Nerve Graft: If the nerve is ruptured or severely damaged, a nerve graft may be used to repair the injury. This involves a surgeon splicing the damaged nerve with a healthy nerve tissue taken from another part of the child's body. Nerve grafting is one of the most successful surgical options for children with Erb's palsy, and the best results are generally seen when the procedure is performed at the youngest age possible.
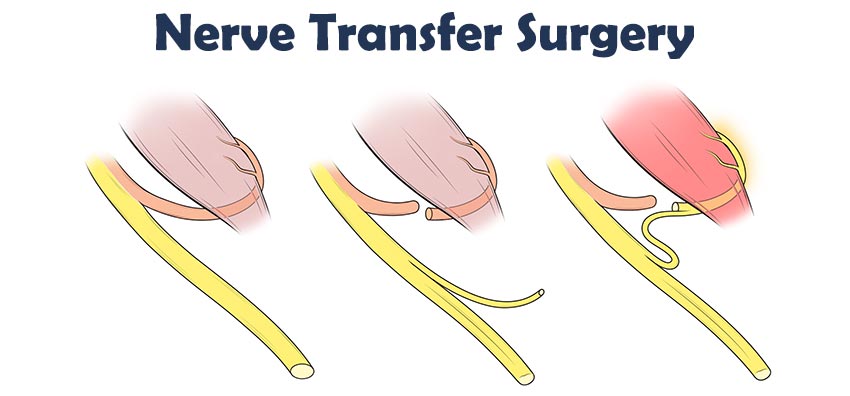
- Nerve Transfer: In cases where nerve grafting alone cannot restore function, a nerve transfer may be considered. This involves moving a healthy nerve from one muscle to another to help restore function in the affected limb. Although full recovery may not always be possible, nerve transfer can re-establish some level of movement and strength in the affected area.
After microsurgery, many children with brachial plexus injuries like Erb's palsy continue to experience some weakness in the shoulder, arm, hand, or fingers. Other surgical options that may be considered to address complications that exist after nerve surgery include:
- Neuroplasty: This minimally invasive surgery involves a surgeon removing the scar tissue that may have formed around the damaged nerves. This procedure aims to improve nerve function by relieving pressure on the affected nerve roots and allowing for better nerve regeneration.
- Dorsal Root Entry Zone (DREZ) Surgery: This technique is often used to alleviate chronic pain in cases of avulsion injuries. DREZ surgery involves removing or cauterizing the affected nerve tissue in the dorsal root entry zone. By targeting the area where sensory nerve fibers enter the spinal cord, this procedure is particularly useful in providing significant relief for individuals experiencing severe, ongoing pain that does not respond to other treatments.
- Release of Joint Contractures: Over time, brachial plexus injuries can cause the muscles and soft tissues around the shoulder and elbow joints to become stiff and form contractures. If left untreated, joint contractures can lead to permanent deformities, making it difficult for the child to move the affected arm. In such cases, surgical intervention may be necessary to release the contractures and restore movement. The procedure typically involves cutting through the tight tissues, including muscles, tendons, and ligaments, to relieve the stiffness and allow the joint to move more freely.
- Tendon Transfer: A tendon transfer is a surgical procedure that involves relocating a functioning tendon from its normal attachment in the body and reattaching it to a new location. Tendon transfers are most commonly performed around the shoulder to improve the child's ability to raise their arm. However, depending on the injury's location and severity, tendon transfers may also be done in the forearm, wrist, or hand.
For example, a healthy tendon may be moved from a muscle in the upper arm to the shoulder to help raise the arm. The goal of tendon transfers is to restore movement and strength in the affected limb by transferring a healthy tendon to replace a damaged one. After the procedure, children are typically required to wear a cast for four to six weeks. This cast stabilizes the surgical site, allowing the relocated tendon to heal properly in its new position. - Joint Reduction Surgery: When thickened or stiff tissues around a joint cause it to come out of place, especially in the shoulder, surgery may be needed to put the joint back in place. An open reduction of the shoulder joint (capsulorrhaphy) involves repositioning the humeral head within the joint and surgically tightening or repairing loose or damaged tissues around the area.
 This procedure is often performed alongside other treatments, such as tendon transfers or soft tissue releases to address the persistent muscle weakness that has caused the joint instability or dislocation. Recovery time can vary depending on the severity of the injury, however, with proper care, the child can regain strength, flexibility, and mobility in the affected joint.
This procedure is often performed alongside other treatments, such as tendon transfers or soft tissue releases to address the persistent muscle weakness that has caused the joint instability or dislocation. Recovery time can vary depending on the severity of the injury, however, with proper care, the child can regain strength, flexibility, and mobility in the affected joint. - Osteotomy: This procedure involves a surgeon cutting and reshaping bones to correct alignment issues and improve the function of the affected limb in children with brachial plexus or peripheral nerve conditions. Typically performed on the humerus (upper arm bone) or forearm, this procedure addresses deformities or misalignments that may restrict movement or cause discomfort. Recovery typically involves a period of immobilization with a cast or brace followed by physical therapy to rebuild strength and restore the full range of motion in the affected limb.
Nerves recover slowly, and it may take several months or even years for a child to experience a notable improvement in function and movement in the affected limb. After surgery, your doctor's child will discuss various follow-up treatment and rehabilitation options based on your child's unique situation.
Not every child with Erb's palsy will fully recover; however, when treatment begins as early as possible, a child's odds of experiencing the most meaningful improvement in strength, flexibility, and function are higher. Your child's doctor will continue to evaluate your child's development and may adjust their treatment plan as needed.
Who Can Be Held Liable for Brachial Plexus Injury?
Depending on the facts of your situation, a birth injury medical malpractice claim may not be limited to the attending physician who delivered your child. There is a wide range of healthcare professionals, such as nurses or anesthesiologists, who may also be held at fault in a birth injury case.

Here are some examples of medical professionals that could be held liable for your child's facial nerve paralysis:
- Doctors and surgeons
- Nurses
- Anesthesiologists
- Hospitals
- Healthcare institutions
- Other hospital staff
A medical malpractice lawsuit brought against a hospital usually involves hospital employees such as nurses, anesthesiologists, and technicians. A hospital would typically not be held liable for the negligent actions of a doctor who works at a hospital as an independent contractor. In situations where a doctor is employed by the hospital directly, however, the hospital may be held vicariously liable for malpractice by a doctor.
In the context of medical malpractice actions, a hospital can also be held directly liable for its own negligence if it fails to make reasonable inquiries into a member of its medical staff's education, training, and licensing. A hospital may also be found directly responsible for negligence if it fails to protect patients from harm by ensuring there is always enough registered nurses and other staff on duty to provide care as needed. A qualified birth injury malpractice attorney can discuss the specifics of your case with you, help you identify who should be held responsible for your child's birth injury, and bring a lawsuit against all negligent parties.
Recoverable Compensation for a Brachial Plexus Birth Injury
Taking legal action against a negligent doctor, hospital, or other healthcare professional may allow you to recover compensation for birth injury-related expenses you've incurred. Damages in a birth injury lawsuit fall into two categories: economic and non-economic damages.
Economic damages account for any monetary losses you've sustained as a result of the birth injury. Non-economic are awarded to compensate the victim for subjective, non-financial losses such as the pain and emotional suffering they endured due to the injury. A medical malpractice attorney can evaluate your case and help you determine the compensation you may be eligible to recover.
Here are some examples of recoverable damages in a birth injury case:

Economic Damages
- Medical and Life Care expenses (past and future)
- The cost of physical, occupational, or speech therapy (past and future)
- Parent's lost income due to tending to their child's needs (past and future)
- The cost to modify a home/vehicle and make it accessible
- The child's reduced ability to work and earn income in the future
- The cost of nursing and personal home care by trained professionals
Non-economic Damages
- Psychological and emotional trauma
- Physical pain and discomfort
- Loss of enjoyment of life
- Paralysis, scarring, and disfigurement
In addition to economic and non-economic damages, punitive damages may be awarded in cases where a doctor or other healthcare provider has committed grossly negligent or reckless acts. These damages are intended to punish the at-fault party for their egregious behavior and serve as a warning to discourage others from engaging in similarly negligent behavior.
Even though the immediate costs of dealing with a birth injury can be financially devastating, the long-term costs of caring for a child with Erb's palsy can be even greater. The settlement amount you will receive will depend on several factors, including the severity of your child's injuries, how long the condition is expected to last, and the type of treatment your child needs.
For example, if your child requires only a few check-ups while their brachial plexus injury heals on its own, your medical bills are likely to be lower, and you can expect a lower settlement award. However, if their congenital birth injury is severe and your child is unable to use muscles for the rest of their life, this will be taken into consideration, and the settlement amount will typically be higher. An experienced birth injury attorney will work with you to figure out the extent of your child's condition and see what damages may arise from your case.
Calculating how much your birth injury claim might be worth will typically require us to draw on the experience and knowledge of our vast network of financial and qualified medical experts. If you have questions about compensation, reach out to one of our birth injury lawyers as soon as possible so we can inform you of your legal options and create an action plan moving forward.
The Importance of Working with an Experienced Birth Injury Lawyer
When your child suffers a birth injury, it can leave you feeling overwhelmed and confused. In navigating the complex legal system, working with an experienced birth injury lawyer who specializes in these cases is crucial to securing compensation for harm caused during childbirth.
If you have questions about your next steps, our birth injury lawyers are available to answer them. We'll keep you informed about any developments in your case and help you understand your options for securing the compensation you and your child need.
Contact Our Birth Injury Attorneys Today

Our team of trained and compassionate professionals at Miller Weisbrod Olesky understands that your child's health and happiness are your top priorities as a parent. That's why we are dedicated to fighting for families of children whose birth injury is caused by medical errors and have successfully represented clients in more than 20 states.
For the past 30 years, our nationally recognized birth injury legal team has secured multi-million-dollar results for families like yours to help victims of birth injuries access the care they need. We are passionate about fighting for the justice our clients deserve, and we'll be here for you every step of the way.
If you believe that your child's facial nerve palsy was caused by medical malpractice, reach out to us now to learn what we can do for you. Call us today toll-free at (888) 987-0005 or fill out our online case evaluation form to schedule your free consultation.
Birth Injury Free Consultation
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.