Birth Injuries from Medical Procedures
Medical Procedures During Pregnancy
When pregnancy complications or labor and delivery complications arise, an expecting mother may need to undergo a medical procedure to protect her or her baby’s wellbeing. In some cases, a newborn child may require a medical procedure when they are born with birth complications.
Whether it’s the mother or her newborn, healthcare professionals must exercise extreme caution when operating because the effectiveness of an emergency medical procedure can be the deciding factor between an infant’s life or death.

Some medical procedures are more invasive than others; an expecting mother’s risk for injury, as well as the risks of birth injury her baby will face, can fluctuate depending on the type of complication and the nature of the procedure.
However, one thing is for certain: when healthcare professionals make preventable errors during prenatal appointments, during labor, or while administering emergency neonatal care, the risk of a birth injury and sustaining permanent bodily damage increases dramatically.
Both an expecting mother and her newborn child can sustain devastating injuries when medical malpractice occurs. For example, a delayed C-section (one of the most common procedural errors) can prolong the time a baby goes without oxygen and blood flowing to the brain, increasing their risk for severe hypoxic (lack of oxygen) and ischemic (lack of blood flow) brain injuries.
Among the most severe is hypoxic-ischemic encephalopathy (HIE), a permanent brain injury that affects a child's cognitive and physical development and often leads to developmental delays. HIE is the leading cause of cerebral palsy.
Free Legal Consultation
Birth Injury Lawyers
(888) 987-0005Our Birth Injury Lawyers are available to meet you in your home or the hospital.
We have decades-long proven track record of results for children and families across the United States who have suffered from all types of medical procedures that were conducted improperly. Our team of specialized birth injury attorneys and registered nurses can review the unique circumstances of you or your family’s case to deliver the treatment, care, and financial resources you deserve.
We work on a contingency fee basis, meaning you won't pay any fees unless we win your case. Contact us today to schedule your free legal consultation by calling our toll-free line at (888) 987-0005 or by filling out our online request form.
What are Common Maternal Medical Procedures?
Cesarean Section Delivery

Cesarean delivery (C-section) is a surgical procedure used to deliver a baby through incisions in the mother’s abdomen and uterus. A doctor will order a C-section procedure for an expecting mother when her child’s risk of injury becomes too high for a vaginal birth.
There are many different pregnancy complications that can lead to a C-section. For example, conditions like macrosomia or cephalopelvic disproportion may indicate that the baby is too large to safely fit through the mother’s birth canal. Or sometimes the baby is in an abnormal fetal position that makes it unsafe to deliver, like if their feet are pointed out toward the cervix (known as breech position).
Sometimes a C-section is required when there is a problem with the baby’s umbilical cord, like if it’s wrapped around their neck and cutting off their oxygen supply.
In general, whenever a complication arises that puts the baby in a state of fetal distress, a C-section is likely the safest method for delivery. Doctors should be monitoring the baby for fetal distress during labor and delivery through fetal heart rate monitoring strips to ensure the birth is progressing safely.
How Quickly Should a C-section be Done?
The American College of Obstetricians and Gynecologists (ACOG) recommends that the interval between the decision and initiation of the C-section should be no more than 30 minutes. But ACOG also recognizes that some C-sections must be performed faster depending upon the emergency condition. Examples of conditions that would require more urgent action include a mother’s uterine rupture, a placental abruption, or a severe lack of oxygen in the baby.
What Mistakes can Medical Professionals Make During a C-section?
A C-section is a serious medical procedure that carries substantial risk to the mother’s and newborn’s wellbeing. It requires a mix of both urgency and caution from medical providers to decide on and start the procedure without delay, while at the same time not foregoing the necessary safety steps and precautions. Examples of medical negligence can include:
- Not recognizing the signs of a high-risk pregnancy and failing to order a C-section.
- Delaying a C-section procedure past the point of what’s safe, resulting in a birth complication or injury.
- Making an improper incision into the mother’s abdomen or uterus, resulting in a punctured organ or excessive bleeding.
- Making anesthesia errors when administering too much or not enough regional or general anesthesia to the mother before the procedure.
- Improper handling when removing the child from the mother’s womb, such as using excessive force that leads to bruising or a bone fracture.
- Scheduling and performing a C-section before the baby is ready, resulting in a premature birth and increasing the risk of Respiratory Distress Syndrome (RDS).
It’s important to note that it requires a detailed review of the specific facts and timeline of a mother’s C-section delivery and the action taken shortly after it before making a definitive judgement as to whether medical malpractice played a factor in her child’s birth injury.
Vacuum Extraction and Device-Assisted Delivery
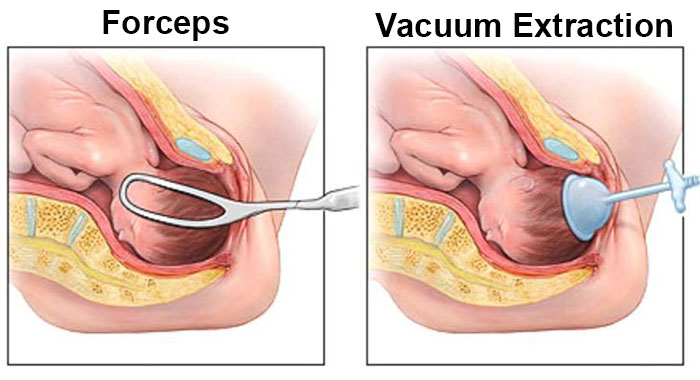
When a child becomes stuck in their mother’s birth canal during delivery, the option for a C-section delivery has typically already passed and become unsafe. To avoid the dangerous risks that come with a prolonged or arrested labor, doctors may use birth-assistive medical devices to get them unstuck and delivered safely. The two most commonly used tools are forceps and vacuum extractors.
During a forceps delivery, the doctor inserts the forceps into the mother’s vagina. The forceps are then positioned around the baby’s head. The doctor then applies traction, pulling on the baby’s head while the mother pushes. Adjusting the baby’s position usually happens between contractions.
A vacuum extractor consists of a metal or soft cup attached to a vacuum pump. The suction cup is applied to the top of the baby’s head in the birth canal. As with forceps delivery, vacuum-assisted vaginal delivery involves the use of traction to pull the baby into the world.
When Should Doctors Use Birth-Assistive Tools?
Physicians and other medical professionals caring for a woman in labor may recommend an assisted delivery using forceps or vacuum extraction in cases when:
- The mother’s labor is prolonged or arrested in the second stage, placing unacceptable stress on the unborn child.
- The mother is too exhausted to continue pushing, or if her doctor limits her time pushing due to serious health conditions.
- The baby’s heart rate is non-reassuring, indicating fetal distress that could be caused by reduced blood flow and oxygen to the baby’s brain.
The American College of Obstetricians and Gynecologists (ACOG) recommends that physicians use the following criteria to determine eligibility for vacuum extraction delivery:
- The mother’s cervix is fully dilated
- Her membranes (waters) have ruptured
- The baby’s head is engaged in a vertex presentation
- The doctor knows the fetal position and fetal presentation in the uterus (headfirst, feet first, occiput posterior or anterior)
- An estimate of the baby’s weight has been taken
- The mother’s pelvis is large enough to accommodate the baby
- The mother’s bladder has been emptied
- Healthcare providers have explained the risks and benefits of vacuum extraction delivery
- The doctors have a plan for delivery if vacuum extraction fails
- The mother’s time for pushing is limited because of a maternal health condition
The same criteria must be met for physicians to use forceps as well. For an assisted delivery using forceps, they must also assess where the baby is located within the birth canal (also referred to as the baby’s “station”).
If an expecting mother doesn’t meet all the above criteria, a C-section delivery may be the safer birthing method. C-sections are recommended when doctors detect abnormalities in fetal size (such as macrosomia or cephalopelvic disproportion) that will place known challenges upon vaginal birth.

When vaginal birth is attempted in these scenarios, it can cause an arrested labor or result in other labor and delivery complications like shoulder dystocia (when the child’s head delivers, but their shoulders become stuck behind the mother’s pubic bone).
Using birth-assistive medical devices is also not recommended in cases of premature birth and in known cases of abnormal fetal positioning. In general, when doctors know ahead of time that a mother’s make vaginal birth poses a threat to her wellbeing, they should order a planned C-section delivery rather than have her risk getting injured. Using birth-assistive tools should be reserved for unplanned emergencies and unforeseen labor and delivery complications.
What Mistakes Can Medical Professionals Make When Using Birth-Assistive Devices?
When a physician misuses instruments like forceps or vacuum extractors, it can leave scratches on an infant's scalp. Minor bruising and scratches usually heal on their own unless they become infected. Serious injuries caused by brain swelling and brain bleeds, like cephalohematoma, intracranial hemorrhage, and subgaleal hemorrhages are commonly caused by trauma to the head resulting from improper use of these birth-aiding tools.
Specific examples of negligence when using these tools can look like:
- Failing to explain the risks and benefits of using birth-assistive tools to the mother.
- Failing to obtain informed consent before beginning the procedure.
- Performing assisted vaginal delivery in a facility that is not equipped to handle an emergency C-section.
- Attempting forceps or vacuum extraction with insufficient training or experience.
- Failing to monitor mother and baby before, during, and after delivery using birth-assistive tools.
- Failing to abandon the procedure when it lasts too long or has not been successful.
- Failing to recognize the signs of fetal distress during the procedure.
- Using excessive traction on the baby’s head during the procedure, leading to cerebral compression or skull fractures.
- Attempting a vaginal birth that will require birth-assistive devices when a c-section should have been performed in the first place.
While these mistakes are likely examples of medical malpractice, a mother’s delivery and the use of birth-assistive tools during it must be investigated before determining whether medical malpractice played a factor in her child’s birth injury.
Prenatal Testing

While not commonly thought of as a “procedure,” prenatal testing is comprised of many small procedures that play a vital role in preventing birth complications through identifying and treating potential issues early on. Some of the basic procedures that medical providers are expected to conduct during prenatal testing include:
- Ultrasounds during each trimester.
- Blood tests to check for abnormalities like Rh and ABO incompatibility.
- Fetal heart rate monitoring to detect fetal distress.
- Glucose tests to check for gestational diabetes.
- Culture tests for common maternal infections like Group B Strep.
- Amniotic fluid index (AFI) tests to check for abnormalities like polyhydramnios and oligohydramnios.
These tests and procedures are crucial steps in preventing pregnancy complications from causing harm to the mother or her child. When doctors, nurses, and other healthcare professionals fail to conduct these tests or fail to read the results properly, it can worsen an expecting mother’s conditions and be counted as medical malpractice if it results in a birth injury or birth complication.
Surgical Thrombectomy
A blood clot during pregnancy can be dangerous for both the expecting mother and her child. While minor clots can usually be treated using approved anticoagulant (blood-thinning) medications, more severe clots may require surgery to treat. This procedure is known as a thrombectomy, and it involves the surgeon making an incision into the mother’s blood vessel and manually removing the clot.
Why Are Blood Clots More Common During Pregnancy?
During pregnancy, a woman’s body produces higher levels of estrogen, which triggers an increased production of proteins like thrombin and fibrinogen. These proteins thicken the blood and increase the likelihood of blood clotting. Additionally, a pregnant woman’s blood vessels will clot more easily as a natural bodily response intended to lessen blood loss during labor and delivery.
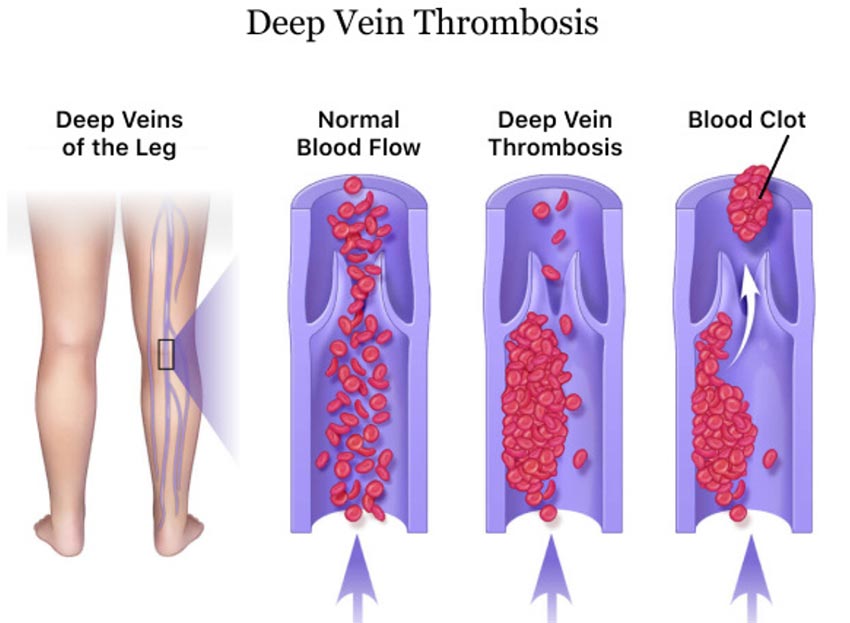
Expecting mothers are more likely to develop blood clots in the legs because of the increased pressure from the growing child on the pelvic blood vessels. This can restrict blood flow to the legs and increase the chance of clotting.
Healthcare professionals must be aware of these risks and carefully monitor expecting mothers so they can administer appropriate information and treatment to safeguard them from the dangers blood clots present.
What Mistakes Can Medical Providers Make During a Thrombectomy?
Like all medical procedures, surgical thrombectomies carry the risk of harming the mother when healthcare professionals make negligent errors. Examples of mistakes that can constitute medical malpractice include:
- Ordering a thrombectomy procedure in cases where anticoagulant medication would work instead.
- Failing to remove the full blood clot, resulting in a fragment (embolus) breaking off and travelling through the bloodstream.
- Puncturing a nearby blood vessel, resulting in excessive bleeding.
- Failing to recanalize the blood vessel (meaning failure to restore blood flow within the blocked vessel).
A mother’s thrombectomy procedure and the action taken shortly after must be closely analyzed before making a definitive judgement as to whether a medical malpractice claim exists.
What are Common Newborn Medical Procedures?
Neonatal Resuscitation
Neonatal resuscitation is a medical procedure performed on newborns who have difficulties with breathing on their own. A newborn may need resuscitation when they show signs of fetal distress before birth, have low APGAR scores, have a weak cry, are showing symptoms of respiratory distress syndrome, or are born prematurely.

At least 10% of newborns need help with respiration and breathing in the moments and hours after they are born. About 1% of newborns need extensive neonatal resuscitation to avoid or minimize birth-related brain injuries, including hypoxic-ischemic encephalopathy (HIE).
How Does Neonatal Resuscitation Work?
The American Academy of Pediatrics (AAP) developed the Neonatal Resuscitation Program in 1987. This program uses an “evidence-based approach to newborn resuscitation and facilitates effective team-based care for providers who attend to newborns at the time of delivery".
All medical staff involved in a child’s delivery are required to be NRP certified. When determining if a newborn needs resuscitation, the medical team must ask themselves the following questions:
- Was the infant born after a full-term gestation?
- Is the amniotic fluid clear of meconium and evidence of infection?
- Is the infant breathing or crying?
- Does the infant have good muscle tone?
If the answer is “yes” to all four questions, then the baby does not need resuscitation. However, even if only one question receives a “no” answer, it means the baby will need at least some form of neonatal resuscitation. Generally, the team should provide the baby with one or more of the following actions done in sequence:
- Stabilization: They should provide warmth, position the baby to make breathing easier, clear the baby’s airway of any blockages like mucous or debris, stimulate the baby, and reposition them if necessary.
- Ventilation: If the baby’s breathing has not improved, the team then provides additional ventilation. For example, they may give supplemental oxygen or provide positive pressure ventilation (PPV).
- Chest compressions: The team may move on to chest compressions if their previous efforts have not worked.
- Medication: Epinephrine can stimulate breathing and heart rate. Other medications help with volume expansion.
What Mistakes Can Medical Providers Make During Neonatal Resuscitation?
Knowing the protocols is only the first step in adequately resuscitating a baby who cannot breathe sufficiently. Medical providers only have seconds to make the decision to resuscitate and move forward with procedures. Common medical mistakes during this process can include:
- Failure to detect fetal distress prior to birth through improper or insufficient fetal heart rate monitoring.
- Waiting too long to resuscitate, increasing the risk of infant death.
- Failing to detect debris in the newborn’s airway passages such as mucous, vomit, or meconium.
- Providing insufficient ventilation, either through improper use of equipment or failure to perform ventilation long enough to be effective.
- Using excessive force when performing chest compressions, resulting in bruising, rib cage fractures, or any other injury.
- Prescribing the wrong medication or the incorrect dosage of a heart rate medication like Epinephrine.
- Failure to closely monitor or follow up on a newborn’s status after performing neonatal resuscitation.
While these mistakes can sometimes signal that medical malpractice occurred, no two births are the same. A thorough examination with all the facts and details of the newborn’s birth is required before determining if a legal claim exists.
Therapeutic Hypothermia (Brain Cooling)
Therapeutic hypothermia is a medical procedure done shortly after birth to reduce the effects of brain injuries like hypoxic-ischemic encephalopathy in infants. The therapy involves cooling the baby’s core temperature to around 92.3 degrees Fahrenheit. After 72 hours, medical staff begin to gradually rewarm the baby while simultaneously monitoring the baby’s vital signs. Cooling or rewarming too quickly can harm the baby’s brain and other organs.
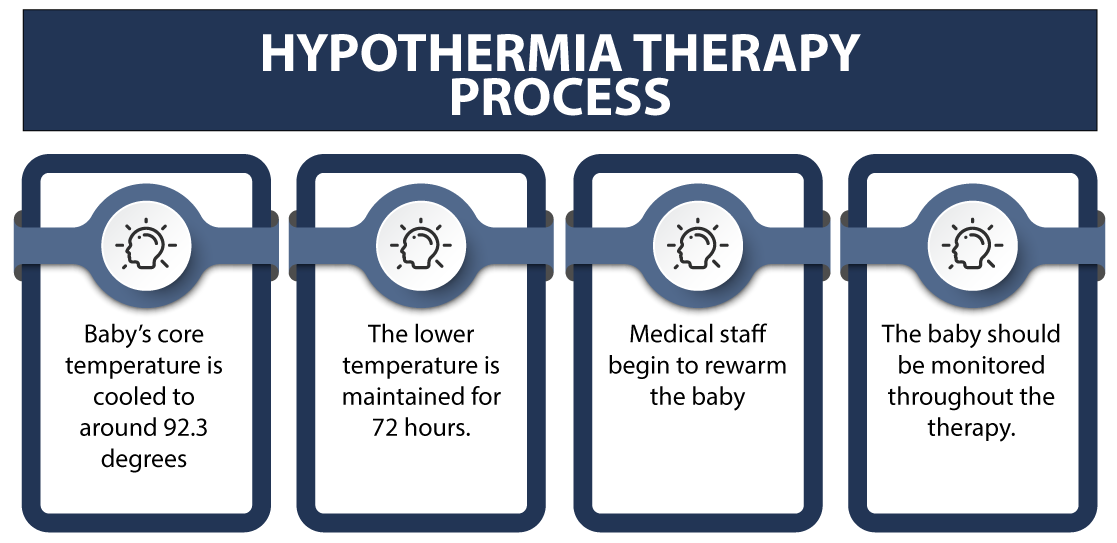
How Does Therapeutic Hypothermia Help Newborns?
A number of complex processes occur or are suppressed during therapeutic hypothermia treatment, particularly in the baby’s brain. The procedure, when conducted properly, aims to have the following effect on the infant:
- Reduction of the cerebral metabolism that slows cell depolarization.
- Reduction of the accumulation of excito-toxic neurotransmitters.
- Suppression of oxygen-free radical release.
- Suppression of expected cell death (apoptosis).
It’s crucial that doctors and other healthcare providers carefully assess the events that caused their potential brain damage in connection with current test results. Failing to provide this treatment could worsen the baby’s brain injury, causing lifelong disabilities or death.
What Mistakes Can Medical Providers Make During Therapeutic Hypothermia?
The therapeutic hypothermia procedure involves collaboration between many types of healthcare professionals, including neonatologists, nurses, radiologists, and lab technicians. These experts must work closely together to observe and analyze the newborn’s symptoms, diagnose a brain injury, and initiate the cooling treatment within minutes following the child’s birth.

Examples of potential mistakes or lapses in medical care can include:
- Failing to identify a newborn’s brain injury upon birth.
- Identifying a brain injury but delaying the therapeutic hypothermia treatment past the window of where it would be an effective treatment.
- Failure to inform parents that their child needs or is having brain cooling treatment.
- Performing the treatment incorrectly using improper equipment or ending it prematurely.
- Performing the treatment for over 72 hours, risking adverse effects on the newborn such as seizures or worsening of their brain injuries.
Medical malpractice is not always black or white; it takes a detailed review of the facts and timeline of a child’s birth and subsequent medical procedure before determining whether a legal claim exists.
G-Tube Placement
Sometimes a child is born with birth complications that make them unable to breastfeed or bottle-feed. In these situations, G-tube insertion may needed to ensure these children receive the necessary nutrients to grow and thrive.

A gastrostomy tube (referred to commonly as a G-tube) is a type of feeding tube that is surgically inserted into the child’s stomach. Medicines, fluids, and foods (in liquid form) travel through the tube and are directly delivered to the child’s stomach so they can properly take in and digest vital nutrients.
What Does the G-tube Procedure Look Like?
Inserting a G-tube requires a short surgical procedure that usually takes under an hour to complete. The patient is put to sleep with general anesthesia for the duration of the surgery.
The G-tube is typically inserted using one of two methods:
- PEG Procedure: A percutaneous endoscopic gastrostomy (PEG) procedure is the most common G-tube insertion method. To guide the G-tube, the surgeon uses a tool called an endoscope. An endoscope is a type of medical camera that is typically inserted through the mouth and guided down the esophagus and into the stomach.
A small incision is made into the child’s abdomen as the surgeon uses the endoscope camera feed to find the prime spot to attach the G-tube. The stomach is also inflated with air so it can be closer to the abdominal wall for attachment. - Laparoscopic Surgery: A laparotomy is very similar to the PEG procedure. The surgeon makes a few incisions (usually 2 or 3) to the child’s abdomen to access their abdominal cavity. Instead of an endoscope, the surgeon uses a laparoscope (a thin tube with a light and camera) to guide the G-tube in.
Unlike an endoscope, the laparoscope is inserted directly into one of the abdominal incisions. A laparoscope generally gives the surgeon a better visualization of the abdomen for placement, but the surgery has a longer recovery period than the PEG procedure due to the multiple incisions made to the baby’s belly.
In addition to these two methods, a G-tube can also be inserted through open surgery, where the surgeon makes a single large incision to access the stomach directly without using a medical camera. While open surgery was once the traditional standard method for G-tube insertion, laparoscopic and endoscopic procedures are more common now due to their minimally invasive nature and faster recovery periods.
What Mistakes Can Medical Providers Make With G-tube Insertion?
There are many different errors that healthcare teams can make when inserting a G-tube and caring for children afterward. Examples of medical negligence can include:
- Failure to identify a child’s need for a feeding tube, resulting in a delay of care that leads to further complications to their health.
- Failure to conduct proper testing before a g-tube procedure (x-rays of the child’s gastrointestinal/digestive system.
- Making a surgical error during the g-tube insertion procedure, resulting in tube displacement, breakage or leakage, tube malposition, knotting, or puncturing of the organs or intestinal tract.
- Errors while administering anesthesia during a g-tube insertion procedure.
- Failure to properly educate families of children with g-tubes on how to use it or clean it, resulting in a complication.
- Failure to schedule timely checkups and follow-ups for children with g-tubes to monitor their progress.
- Premature removal of the g-tube, resulting in further injury or complications.
While these medical mistakes may rise to the level of medical malpractice, it requires a thorough review of each child’s circumstances before knowing for certain if they have a case.
About Newborn G-tube Insertion
Did Medical Malpractice Occur My Child’s Medical Procedure?

A medical procedure is supposed to save an expecting mother’s or newborn’s life, not to cause further harm. When doctors, obstetricians, nurses, and all other healthcare professionals make preventable errors during procedures, it can become more harmful than helpful and increase a baby’s odds of birth injuries and even death.
If a family believes medical negligence contributed to a mother’s or her child’s injuries, legal support may be an option. A specialized birth injury attorney can review the medical records and circumstances to assess whether a viable claim for medical malpractice exists.
Parents whose children suffer from the long-term effects of birth complications, as well as families who have suffered the loss of their baby or the tragic death of the mother, deserve to know whether it could have been prevented. Our dedicated birth injury lawyers want to help you find those answers and obtain the funds necessary to improve the quality of life for your child.
If your child has been diagnosed with a birth injury and you suspect this may have been caused in part by an error during a medical procedure, Miller Weisbrod Olesky will thoroughly investigate the facts and hold the responsible medical providers accountable by pursuing medical malpractice claims against them.
Sometimes families are hesitant to reach out to a medical malpractice attorney or law firm. They may feel overwhelmed by their circumstances or are worried that a law firm will not be able to help them. But the only way to find out if you have a case is to talk to an attorney who understands how birth injuries can lead to developmental delays and other complications that require long-lasting medical support.
What Is the Statute of Limitations in a Birth Injury Lawsuit?
A statute of limitations (SOL) is a law that sets a time limit on how long an injured person has to file a lawsuit after an accident. It is essential to understand that statutes of limitations vary based on the type of case and the state where it is filed. For instance, the deadline for birth injury claims is typically different from other claims, such as injury to personal property, fraud, contract disputes, and collection of debts.
Generally, the clock starts ticking on the date the injury occurred. However, there are exceptions to this rule, and in some cases, the statute of limitations starts when a person discovers or reasonably should have discovered an injury. When dealing with government agencies, SOLs can become even more complex.
For example, if the party that injured you was:
- A federal employee
- Employed by a military hospital, Veterans Administration facility, or a federally funded medical entity
You may need to file a birth injury claim under the Federal Tort Claims Act (FTCA). In FTCA cases, claimants must go through certain administrative procedures before filing a lawsuit. In some states, if the negligent party was a local or state government hospital or the doctors and medical providers are employees of a governmental entity, the time period in which you must give "notice" may be shorter.
If your case is filed outside of the statute of limitations, it will typically be dismissed, and you will not be eligible to recover compensation for your injuries. Determining when a statute of limitations begins on your case can be tricky. If you're considering pursuing compensation for a birth injury, contacting an attorney as soon as possible is in your best interest.
How Can Our Birth Injury Attorneys Can Help?

Injuries and fatalities from a medical procedure can usually be prevented, but it takes a detailed expert review of the facts and circumstances of an infection case determine whether the injury was the result of medical malpractice.
Our Process
At Miller Weisbrod Olesky, a team of committed birth injury malpractice attorneys, nurses and paraprofessionals uses our detailed medical negligence case review process to assess your potential birth injury case. We start by learning more about you and your child and the status of meeting/missing developmental milestones. We then gather medical records to determine what happened before, during, and after your delivery. We call in skilled medical experts who review your records and let us know if they think medical errors could have caused you or your child's injuries.
If we feel medical negligence caused or contributed to complications with your pregnancy or your child's injuries, we meet with you to discuss how you can receive compensation from the medical professionals who made the errors.
At no point in our legal intake process will we ask you to pay anything. The medical review of your case and the consultation are free. We only receive payment when you do. The sooner you reach out to us, the sooner we can begin investigating your case and gathering the evidence needed to support your claim.
We work on a contingency fee basis, meaning you won't pay any legal fees unless we win your case. Contact us today to schedule your free legal consultation by calling our toll-free line at (888) 987-0005 or by filling out our online request form.
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.