Blood Clots During Pregnancy
Dangerous Blood Clots During Pregnancy
During pregnancy, a woman’s body produces higher levels of estrogen, which triggers an increased production of proteins like thrombin and fibrinogen. These proteins thicken the blood and increase the likelihood of blood clotting. Additionally, a pregnant woman’s blood vessels will clot more easily as a natural bodily response intended to lessen blood loss during labor and delivery.

Free Legal Consultation
Birth Injury Lawyers
(888)987-0005Our Birth Injury Lawyers are available to meet you in your home or the hospital.
Expecting mothers are more likely to develop blood clots in the legs because of the increased pressure from the growing child on the pelvic blood vessels. This can restrict blood flow to the legs and increase the chance of clotting.
Healthcare professionals must be aware of these risks and carefully monitor expecting mothers so they can administer appropriate information and treatment to safeguard them from the dangers blood clots present.
While everyone is at risk for developing a blood clot, pregnancy increases that risk fivefold.” – Center For Disease Control (CDC), May 2024
How Can Blood Clots Affect Pregnancy?

An expecting mother’s health is top of mind during pregnancy, and it is critical that any health risks blood clots pose to her or her child are caught early enough before complications arise.
Given that pregnant women are at an increased risk of developing blood clots, it’s important they are informed of how clotting can impact their pregnancy and what to look out for. Blood clots can complicate pregnancy and delivery in multiple ways:
- Restricted Blood Flow: The main concern with blood clots during pregnancy is that they can cut off blood flow, which is very important to the child’s development during gestation.
Blood clots that develop in the placenta are especially dangerous as it is the main organ responsible for delivering oxygen and nutrients to the fetus. A placental blood clot can lead to placental abruption (when the placenta detaches from the uterine walls) or cause other placental insufficiencies that can result in a miscarriage or stillbirth. - Birth Injuries/Complications: In less extreme cases, placental blood clots can cause intrauterine growth restriction (IUGR) which leads to lower birth weights. Developmental delays can also occur from blood clots in cases where oxygen was cut off from the child’s brain for a prolonged period.
Damage to the placenta (from blood clots or other factors) can increase the risk of amniotic fluid (liquid in the uterus surrounding the fetus during pregnancy) entering the bloodstream.
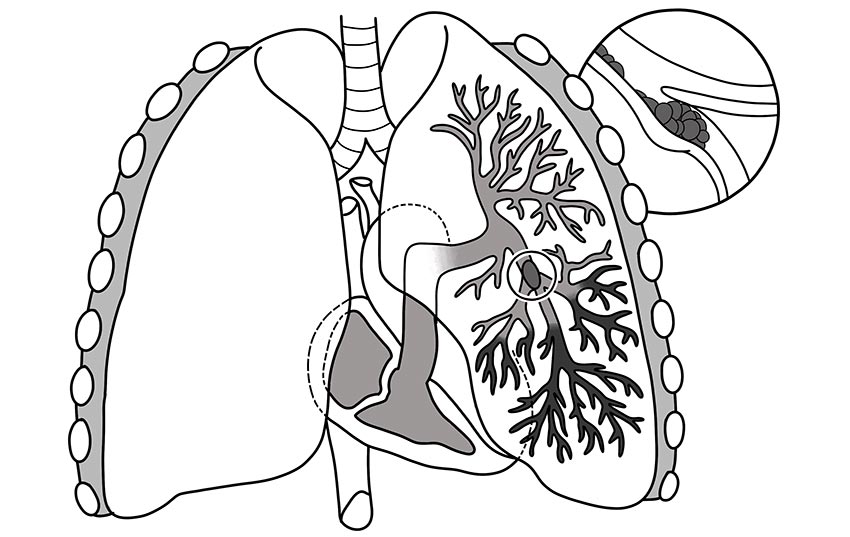
This can cause an amniotic fluid embolism (AFE) which affects the flow of blood and oxygen to the child and can result in brain injuries, asphyxia, fetal distress and even fetal death in extreme cases. - Risk of Pulmonary Embolism: Blood clots in the mother’s arms and legs pose a smaller, but still significant health risk to her health during pregnancy. Should any fragment of a DVT clot break off from within the limbs and travel into the lungs, it can threaten the mother’s oxygen supply and put both her and her child’s lives in jeopardy.
A 2023 study published in the National Library of Medicine cited pulmonary embolisms as a leading cause of maternal morbidity and mortality in Western countries.
Though generally rare, pulmonary embolisms pose a severe risk to the mother’s oxygen supply and overall health, meaning that all DVT cases in the arms and legs should be treated with serious care to prevent it from developing into something more serious.
How To Prevent Blood Clots During and After Pregnancy?
Women are more likely to develop blood clots during pregnancy, but the elevated risk doesn’t end immediately after childbirth. New mothers are still extra susceptible to developing blood clots for around three months post-partum.
That risk increases if the mother gave birth through c-section. There are several preventative measures that new and expecting mothers can take to reduce their chances of forming a blood clot during pregnancy and for the months following:

- Adequate Movement/Mobility After Delivery: Prolonged immobility can lead to reduced blood flow in the legs, increasing chances for a blood clot. The stress on the body during pregnancy deprives women of their normal energy levels, which often makes it harder for them to get enough movement in the day for healthy blood circulation.
Following delivery, it’s important for new mothers to break up their bed rest recovery with minimal amounts of standing and walking so blood can still circulate properly in the legs. - Adequate Fluids Intake: Dehydration can increase the chances of developing a blood clot, so it’s critical that pregnant women ensure they are drinking enough fluids during pregnancy and afterward during their recovery.
- Taking Proper Medications and Treatments: Taking prescribed blood-thinning medication under medical supervision can be critical in aiding the body’s ability to dissolve blood clots and to prevent future clotting.
- Maintaining a Healthy Weight: Being overweight or obese during pregnancy is a risk factor for developing blood clots. During pregnancy, the mother’s healthcare provider should set an appropriate expectation for weight gain during pregnancy (depending on their body mass index). Pregnant women should consult with their doctor should they have any concerns with weight management.
- Wearing Compression Stockings: Compression stockings are tight-fitting hosiery socks that apply pressure to the legs. They are worn to improve circulation and reduce swelling in the legs. A doctor may prescribe compression stockings during or after pregnancy to reduce the risk of blood clots forming.
- Avoiding Smoking and Alcohol: Behaviors like drinking alcohol or smoking cigarettes increase the chances of forming a blood clot, as well as contributing to other adverse health affects for the fetus. It is generally recommended to avoid drinking and smoking during pregnancy and in the months following giving birth.
What are the Most Common Types of Blood Clots During Pregnancy?

The scientific term to describe the abnormal formation of a blood clot is thrombosis. Thrombosis can be arterial (clotting within an artery) or venous (clotting within a vein), and pregnant women are at a heightened risk for both.
When a piece of the blood clot (or thrombus) breaks off and travels through the bloodstream, that fragment is known as an embolus, and the blockage it causes is called an embolism. Just like thrombosis, an embolism can also be arterial or venous and is typically named after the area affected.
The following blood clots are the most common during pregnancy:
- Deep venous Thromboembolism (DVT): DVT is a type of blood clot formed in a vein that’s deep below the skin and into the muscles. This type of blood clot typically forms in the lower leg or thigh veins but can also occur in other deep veins located in the arms or the pelvis.
Pregnant women have a higher risk of developing DVT in the legs due to increased pressure on the pelvis from the fetus, which can restrict blood flow to the lower half of the body.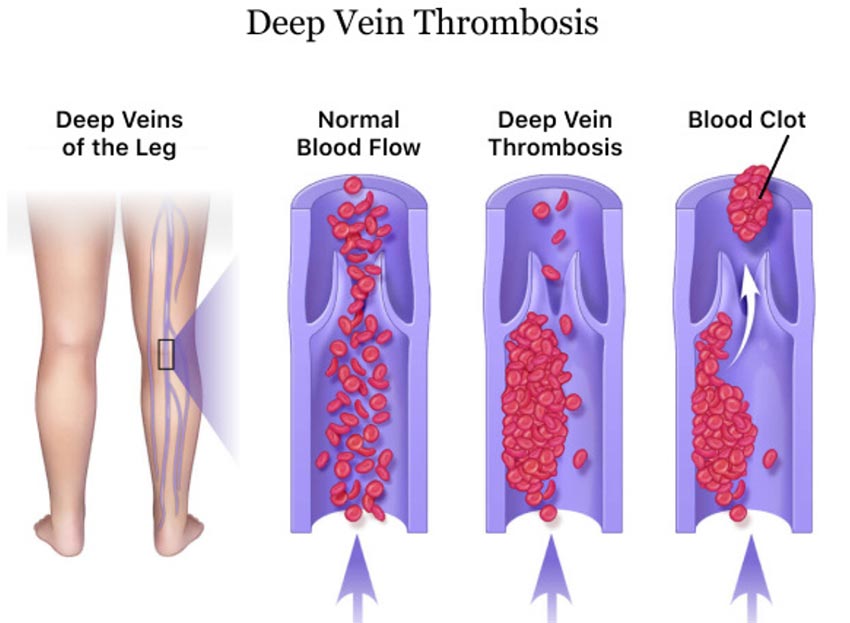
- Pulmonary Embolism: A pulmonary embolism occurs when a fragment of a blood clot breaks off and travels through the blood stream and into the lung arteries. Pulmonary embolisms are life-threatening because they can block oxygen from making it into the lungs, which can cause permanent lung damage and even damage to other organs such as the heart and brain.
| Type of Blood Clot | Area Affected |
|---|---|
| Deep Venous Thromboembolism (DVT) | Lower leg, Ankle, Foot, Arms, Thigh, Pelvis |
| Pulmonary Embolism | Lungs |
| Coronary Embolism | Heart |
| Cerebral Embolism | Brain |
| Cerebral Venous Thrombosis | Brain |
| Portal Vein Thrombosis | Liver |
| Renal Vein Thrombosis | Kidneys |
Risk Factors: What Causes Blood Clots During Pregnancy?

A variety of risk factors can increase the chances of a blood clot during pregnancy. Not all clotting is detrimental; blood naturally clots when exposed to air, which helps to close open wounds like cuts and scrapes, protecting the body from infections.
When clotting occurs in a blood vessel, however, it can typically be linked back to one of the following risk factors:
- Pregnancy: Pregnant women face a higher risk of developing blood clots during the gestational period. This is primarily because the body produces higher levels of estrogen during pregnancy, a hormone that triggers an increased production of blood clotting proteins like thrombin and fibrinogen.
Additionally, blood vessels will clot more easily as a natural bodily response intended to lessen blood loss during labor and delivery.
Expecting mothers are more likely to develop blood clots in the legs. This is because of the increased pressure on the pelvis blood vessels from the growing child, which can restrict blood flow to the legs.
Because of these additional risks that come with pregnancy, healthcare professionals must closely monitor expecting mothers and treat any blood clot they find promptly before further birth complications occur for the mother or for her unborn child. - Injury to a Blood Vessel: Injury to a blood vessel (known as vascular trauma) can occur from many different types of injuries such as blunt trauma from impacts or falls, excessive muscle strain, medical procedural errors during IV insertion, bone fractures that poke and damage nearby vessels, or any other injury that can tear, stretch, compress or puncture veins and arteries. These will typically result in a DVT blood clot.
During pregnancy, the blood is already naturally thickened due to excess hormones being released into the bloodstream. This will result in faster clotting when a blood vessel is injured. - Underlying Health Conditions: A pregnant mother may be more susceptible to blood clots as a complication from any underlying conditions they may have. This can range from acquired chronic diseases like certain cancers to rare conditions like antiphospholipid syndrome (an autoimmune disorder) or arteriosclerosis (a disease causing the thickening/hardening of the arteries).
Sometimes, certain conditions can be genetically inherited from the mother’s family, increasing their risk of blood clots. Such conditions can include, but certainly aren’t limited to thrombophilia, sticky platelet syndrome (SPS), dysfibrinogenemia and congenital nephrotic syndrome.
It’s important for healthcare providers to be aware of any underlying conditions the mother may have so they can properly assess the risk of blood clots and other pregnancy complications. - Obesity: Pregnant women with maternal obesity are put at a higher risk for developing blood clots. Obesity tends to result in the bloodstream having lower levels of nitric oxide, a molecule that is critical to protecting the blood vessels’ lining. This can result in increased inflammation and risk of blood clots forming.
- Prolonged Immobility: An inadequate amount of movement over a prolonged period can result in issues with blood circulation, especially circulation to the legs.
Sitting still for too long prevents the calf muscles from contracting and can cause blood to pool in the lower leg veins, increasing risk of DVT. This phenomenon is observed commonly in patients who have undergone surgery and required additional bed rest afterward.
Lower energy levels during pregnancy can lead to mothers not getting enough mobility during their daily routine, which can put them at a higher risk for blood clots. This also applies to the postpartum recovery period after delivery.
It is for this reason that healthcare professionals ensure that pregnant women get in enough movement after giving birth while at the same time not overexerting themselves and hurting their recovery. - Certain Medications: Medications high in estrogen, such as contraceptives or hormone replacement therapy (HRT) drugs, will increase the risk of blood clots due to estrogen’s effect on the increased production of coagulant proteins.
Nonsteroidal anti-inflammatory drug medications (or NSAIDs) like Advil and Ibuprofen have also been linked to an increased risk of blood clotting because of their interference with the anticoagulants in the blood.
Pregnant women must exercise extreme caution when taking medications and should consult with their primary healthcare provider to make sure that the medicine won’t have any adverse effects to their health.
What Does a Blood Clot During Pregnancy Feel Like?

Symptoms of a blood clot will depend on the type of clot and its location in the body. In general, the affected area will feel tender and may even swell up. Redness around the affected area is another common symptom. Listed below are the common areas affected by blood clots and the common associated symptoms:
- Legs (Deep Vein Thrombosis): Throbbing pain when standing or walking, cramping, skin discoloration, swollen veins, excess warmth.
- Arms (Deep Vein Thrombosis): Arm pain, cramping, skin discoloration, swollen veins, excess warmth, heaviness or fatigue in the arm, paralysis of the arm (in rare cases).
- Lungs (Pulmonary Embolism): Sharp chest pain when breathing, shortness of breath, dizziness or lightheadedness, irregular heartbeat, coughing up blood, fainting, excessive sweating.
- Heart (Coronary Embolism): Sharp chest pain when breathing, shortness of breath, dizziness or lightheadedness, nausea, heart palpitations, irregular heartbeat, coughing up blood, fainting, excessive sweating, physical sensations mirroring those of a heart attack.
- Brain (Cerebral Embolism): Weakness/paralysis in the face, dizziness or lightheadedness, nausea, loss of vision, sudden confusion, difficulty moving or speaking, severe headache with no known cause.
- Thigh (Deep Vein Thrombosis): Throbbing pain when standing or walking, skin discoloration, swollen veins, excess warmth.
- Pelvis (Pelvic Vein Thrombosis): Throbbing pain in the pelvis/lower abdomen or back muscles, sudden swelling in the leg, skin discoloration, swollen veins, excess warmth around the pelvic/groin area.
- Liver (Portal Vein Thrombosis): Stomach pain and bloating, gastric bleeding, rectal bleeding, vomit containing blood, nausea, fever, chills, jaundice (yellowing of the skin), enlarged spleen (visible through computed tomography scan).
- Kidneys (Renal Vein Thrombosis*): Throbbing flank pain (pain in upper abdomen, lower back and sides), soreness in area over the kidney, decreased urine output, blood in urine, protein in urine (testable with a urine albumin-to-creatine ratio test), nausea, fever, vomiting.
*It’s important to note that many cases of renal vein thrombosis are asymptomatic and don’t present any visible symptoms until causing complications like acute renal failure (kidney failure) or a pulmonary embolism if a part the clot travels to the lungs.
How Do You Diagnose and Treat Blood Clots During Pregnancy?
Healthcare providers can usually detect blood clots early on with imaging scans and screenings that are routine for prenatal checkups. These scans can include ultrasounds and magnetic resonance imaging (MRI) tests, as well as CTA scans where a special dye is injected into the mother’s arm to produce pictures of blood vessels and other imaging tests.
Blood and urine test results can also be indicators for a blood clot or clot-related complication. Treatment for these conditions can vary.
- Medications: The administration of anticoagulant medications to fight blood clots is known as anticoagulant therapy. Blood-thinning medications are commonly prescribed to pregnant women with blood clots and can sometimes be taken as a preventative measure against them.
One of the most common medications is Heparin, which is administered via injection into the bloodstream to prevent blood clots and help the body break down existing ones. Pregnant women are also commonly prescribed Clexane, another injectable anticoagulant that is safe to give to expecting mothers.
Not all blood-thinning medications are safe to give to pregnant women, however; the popular blood thinner Warfarin has been linked to bleeding problems and birth defects in children and should be avoided during pregnancy.
Any prescribed drug’s viability will depend on each person’s medical history and unique circumstances. Healthcare professionals must conduct sufficient research and testing to ensure that the medication prescribed will have the desired effect.
This is especially true for pregnant women, as pregnancy can change the body’s reactions to different drugs. In some cases, prescribing the wrong medication can be considered as negligence and constitute medical malpractice. - Surgical Treatments: In some cases, surgery may be required to remove blood clots resistant to anticoagulant therapy. A surgical thrombectomy is a procedure where the surgeon makes an incision into a blood vessel and manually removes the clot.
Thrombectomies can also be performed percutaneously (meaning in a minimally invasive way) by insertion of a catheter that can be used to deliver medication directly to the clot or to suction it out from the blood vessel. This method is known as catheter-directed thrombolysis.
Frequently Asked Questions For Blood Clots During Pregnancy
What Does It Feel Like to Have a Blood Clot in Your Leg?
The leg is the most common part of the body to develop blood clots. Having a blood clot in the leg can feel painful, like a concentrated tenderness and throbbing sensation similar to a strained muscle or an intense cramp.
As for visual signs, the affected area will typically appear swollen and discolored with a reddish hue (or dark blue/purple in some cases). The affected leg may also feel warm to the touch and tender when pressed on.
What Do Pregnancy Blood Clots Look Like?
Because of increased blood vessel development in the cervix during pregnancy, it isn’t uncommon for pregnant women to pass small blood clots vaginally or to experience some light bleeding. These small clots can look like stringy, jelly-like blobs around the size of a dime.
If the clot is larger than the size of a quarter, it may be a sign of an issue. Other signs of an issue include passing these clots frequently or having any pain when bleeding. If these symptoms arise, notify your primary healthcare provider so they can assist you in giving the necessary treatment.
How Long Does It Take to Dissolve a Blood Clot in the Leg?
The amount of time it takes for a blood clot to dissolve depends on multiple factors, including the type of clot, its size, the underlying health conditions of the mother and the methods of treatment already used to address the clot.
A surface clot in the leg can take several weeks to dissolve, whereas deep vein thrombosis (DVT) can take from several months up to a year. Blood-thinning treatments can speed up the process.
Can a Blood Clot Cause High Blood Pressure?
While blood clots can indirectly cause high blood pressure in some cases, research actually suggests that high blood pressure tends to cause blood clots, not the other way around.
Higher blood pressure causes the blood to travel at a higher speed and pressure, which can cause damage to the artery walls. Blood clotting can happen more easily when the internal lining of the arteries isn’t smooth because fats and proteins can get stuck on the rough edges and accumulate.
In the case of a blood clot embolus (fragment) travelling into the kidneys or the lungs, the excess fluid buildup can play a contributing role in causing higher blood pressure. However, a general case of DVT in the leg or arm is unlikely to significantly impact a pregnant woman’s blood pressure.
How Long Can a Blood Clot Go Undetected?
Depending on the location and severity, a blood clot could go undetected for days, weeks or even months before causing complications. Small clots in the arms or legs are likely to become noticeable rather quickly, within about a week or so before symptoms worsen.
Some types of clots, however, such as renal vein thrombosis in the kidneys, often present as asymptomatic and can take longer to detect.
Catching a blood clot as early as possible is key to treating it effectively. Delays in treatment open the door to further complications, such as fragments of the blood clot breaking off and traveling to important organs like the lungs or the heart.
What Are Foods to Avoid If You Have Blood Clots?
There is insufficient evidence to suggest any foods play a significant factor in causing blood clots. However, if you are taking blood-thinning medication, it is recommended to limit intake of certain foods.
Foods rich in potassium and vitamin K, while still safe to eat on blood-thinners like heparin, are generally recommended to not be eaten in excess as they can affect the drug’s ability to prevent blood clots.
Examples of Medical Negligence When Treating Pregnant Women With Blood Clots
It’s important to remember that every medical malpractice case is different. It requires a careful and thorough review of the facts of your case before determining if medical negligence truly played a factor in the injury of you or your child.
However, these medical errors can be an indicator for a case of medical negligence in blood-clot-related injuries and complications:
- Failure to properly screen for blood clotting disorders before pregnancy or during early prenatal care.
- Failure to identify and diagnose a blood clot, delaying necessary treatment.
- Neglecting to educate pregnant women with blood clotting disorders of the signs and symptoms of complications.
- Prescribing medications that will increase the risk of blood clots without proper warning or monitoring.
- Surgical errors when operating on a pregnant woman with blood clots.
- Inadequate communication and coordination of care during or after pregnancy, resulting in an injury or complication.
Was My Blood Clot During Pregnancy Led to My Child’s Birth Injury Preventable?
Birth injuries related to blood clots may sometimes be preventable with proper medical care. Medical negligence, such as failure to catch clotting in the early stages, prescribing the wrong types of medication or poor management of symptoms can all increase the risk of preventable complications for you and your child.
If a family believes medical negligence contributed to a birth complication or birth injury, legal support may be an option. A knowledgeable birth injury attorney can review the medical records and circumstances to assess whether a claim exists.
Parents whose children suffer from related complications, as well as parents who suffered themselves from a blood-clot related injury like a pulmonary embolism, deserve to know whether it could have been prevented with better treatment. Our dedicated birth injury lawyers want to help you find those answers and obtain the funds necessary to improve the quality of life for both you and your child.
If your child has been diagnosed with a birth injury related to a blood clot during pregnancy, and if you suspect this may have been caused in part by medical mistakes, Miller Weisbrod Olesky will thoroughly investigate the facts and hold the responsible medical providers accountable by pursuing medical malpractice claims against them.
Sometimes, families are hesitant to reach out to a medical malpractice attorney or law firm. Parents might feel overwhelmed by their circumstances and worry that a law firm won’t be able to help. But the only way to find out if you have a case is to talk to an attorney who understands how birth injuries can lead to developmental delays and other complications that require long-lasting medical support.
What is the Statute of Limitations in a Birth Injury Lawsuit?
A statute of limitations (SOL) is a law that sets a time limit on how long an injured person has to file a lawsuit after an accident. It is essential to understand that statutes of limitations vary based on the type of case and the state where it is filed.
For instance, the deadline for birth injury claims is typically different from other claims, such as injury to personal property, fraud, contract disputes, and collection of debts.
Generally, the clock starts ticking on the date the injury occurred. However, there are exceptions to this rule, and in some cases, the statute of limitations starts when a person discovers or reasonably should have discovered an injury. When dealing with government agencies, SOLs can become even more complex.
For example, if the party that injured you was:
- A federal employee
- Employed by a military hospital, Veterans Administration facility, or a federally funded medical entity
You may need to file a birth injury claim under the Federal Tort Claims Act (FTCA). In FTCA cases, claimants must go through certain administrative procedures before filing a lawsuit. In some states, if the negligent party was a local or state government hospital or the doctors and medical providers are employees of a governmental entity, the time period in which you must give "notice" may be shorter.
If your case is filed outside of the statute of limitations, it will typically be dismissed, and you will not be eligible to recover compensation for your injuries. Determining when a statute of limitations begins on your case can be tricky. If you're considering pursuing compensation for a birth injury, contacting an attorney as soon as possible is in your best interest.
How Can Birth Injury Attorneys at Miller Weisbrod Olesky Help?

Blood-clot-related complications are preventable in many cases, but it takes a detailed expert review of the facts and circumstances of your pregnancy and your child's birth to determine whether the injury was the result of medical malpractice.
Our Process
At Miller Weisbrod Olesky, a team of committed birth injury attorneys, nurses and paraprofessionals uses our detailed medical negligence case review process to assess your potential birth injury case. We start by learning more about you and your child and the status of meeting/missing developmental milestones.
Then we gather medical records to determine what happened before, during, and after your delivery. We call in skilled medical experts who review your records and let us know if they think medical errors could have caused you or your child's injuries.
If we feel medical negligence caused or contributed to complications with your pregnancy or your child's injuries, we meet with you to discuss how you can receive compensation from the medical professionals who made the errors.
At no point in our legal intake process will we ask you to pay anything. The medical review of your case and the consultation are free. We only receive payment when you do. The sooner you reach out to us, the sooner we can begin investigating your case and gathering the evidence needed to support your claim.
We work on a contingency fee basis, meaning you won't pay any legal fees unless we win your case. Contact us today to schedule your free consultation by calling our toll-free line at (888) 987-0005 or by filling out our online request form.
Contact Miller Weisbrod Olesky
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.