Obesity Related Birth Injuries
Maternal Obesity Complications
Obesity can occur for several reasons, from genetics and family history to certain medications and lifestyle choices. The Center for Disease Control and Prevention (CDC) estimates that two in five U.S. adults are obese. As for maternal obesity, a 2021 report from NeoReviews found that roughly half of all pregnant women in the United States are classified as either overweight or obese.

Obesity during pregnancy can increase the risk of complications that lead to birth injuries. While the severity of these risks can vary, it is vital for healthcare providers to appropriately identify and monitor the exposure to complications that threaten the health of both the mother and her unborn child.
Many of the risks posed by maternal obesity are preventable with adequate medical care. For a mother classified as obese, additional tests and screenings will be necessary before and after delivery to ensure her and her baby’s safety. If the proper care isn’t taken or overlooked and it leads to a birth injury, it can constitute medical malpractice.
Free Legal Consultation
Birth Injury Lawyers
(888) 987-0005Our Birth Injury Lawyers are available to meet you in your home or the hospital.
Miller Weisbrod Olesky has a long history of successful results in birth injury cases, including birth injuries caused by risks factors due to obesity. If you believe your child suffered a birth injury (including cerebral palsy) due to a failure to recognize or respond to an obesity-related birth complication, we will be happy to investigate your case free of charge. We never charge a fee unless we make a successful financial recovery.
What Is Maternal Obesity?
The National Library of medicine defines obesity as anyone with a body mass index (BMI) of 30 or higher. Maternal obesity simply refers to any pregnant woman with a BMI over 30. Anyone can use their own height and weight measurements to determine their approximate BMI and its corresponding weight class.
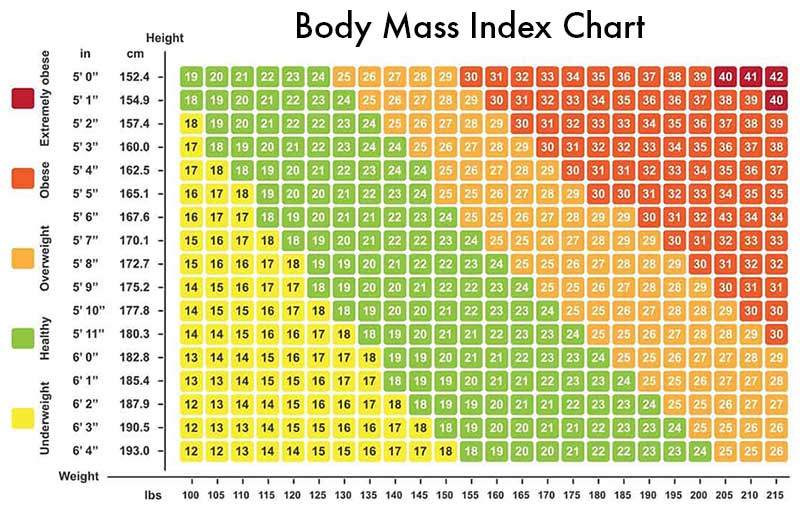
Obesity can be further classified into three subgroups:
- Class I Obesity – BMI range of 30.0 to 34.9
- Class II Obesity – BMI range of 35.0 to 39.9
- Class III Obesity (Known Commonly as Morbid Obesity) – BMI over 40.0
A pregnant woman’s risk of birth complications increases with a higher BMI. These risks can range from gestational diabetes and preeclampsia to preterm birth and other labor difficulties. All of these risks can lead to a birth injury or play a role in long-lasting developmental disorders like cerebral palsy.
What Is Maternal Obesity Linked To?
Maternal obesity has been linked to several complications that can result in a birth injury. These birth complications can be categorized based on when they present themselves, whether it’s during the gestational period, during labor and delivery, or even after the baby has been delivered.
Obesity and Pregnancy Complications: Maternal obesity can play a role in the development of adverse underlying conditions for the mother while she carries her child to term. For example, obesity can build up the body’s resistance to insulin, and increased levels of it in the blood can cause gestational diabetes.
Gestational diabetes can adversely impact the baby’s in-utero development, increasing the likelihood of birth complications like macrosomia and respiratory distress.
Another common pregnancy complication that arises from maternal obesity is preeclampsia. This is a condition that normally occurs in the later stages of pregnancy and is characterized by sudden high blood pressure for the mother. This can lead to complications like gestational hypertension and placental abruption.
Other pregnancy complication risks that are heightened by obesity include neonatal hypoglycemia and intrauterine growth restriction (IUGR). All of these conditions can put both the mother and her unborn child at risk during pregnancy and during delivery.

Obesity and Labor Complications: Maternal obesity can complicate the labor and delivery process, compromising the safety of both the mother and her child. More instances of prolonged and arrested labor have been recorded in cases where the mother was obese. This can be due in part to certain fetal abnormalities such as a large birth weight. Obesity is also a risk factor for triggering premature births, which exposes the child to a number of health risks linked to underdevelopment.
Maternal obesity puts expectant mothers at a higher likelihood for requiring external tools such as forceps and vacuum extractors, which run the risk of accidents. In some cases, vaginal delivery for obese mothers may be deemed unsafe due to the baby’s size or other anatomical conditions.
These women will instead require a cesarean birth (c-section) delivery, which comes with its own risks like infection or operating room errors. Additionally, for obese mothers who have delivered a child via c-section, it is less likely for them to have a successful vaginal birth after c-section (VBAC) in the future.

Obesity and Birth Defects: Research points to maternal obesity playing a factor in birth defects and developmental delays in children. Some defects may be purely physical but not cause inherent harm, such as a high or low birth weight or enlarged parts of the body. Other physical birth defects like shoulder dystocia can severely impact the baby’s physical development and cause long-term nerve damage.
Some birth defects can impact a child’s development for the rest of their life, particularly cases of cerebral palsy and hypoxic ischemic encephalopathy (HIE). Maternal obesity increases the risk of developing complications that can be precursors to these conditions. This sequence of events commonly stems from maternal infections such as group B strep, which increases the chances of brain damage. Obesity coupled with pregnancy can increase the body’s susceptibility to infection, putting both the mother and child at risk.

Symptoms: How Can Maternal Obesity Affect the Fetus?
A mother who has been diagnosed with maternal obesity should be informed of all possible risks her condition may pose to her child. It is important to understand the different risks and necessary procedures that healthcare providers must take to prevent birth injuries from happening. Different complications for the fetus can include:
- Shoulder Dystocia: Babies born to mothers with obesity are at higher risk for shoulder dystocia, where the baby’s shoulders get stuck behind the mother’s pelvic bone during delivery. This condition can lead to brachial plexus injuries, fractures, and nerve damage.
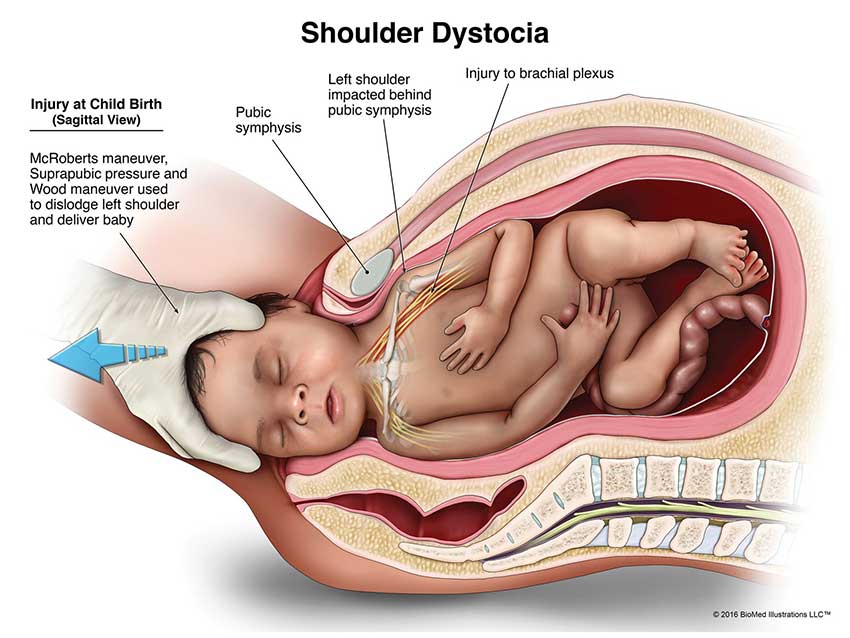
Image courtesy of Biomed Illustrations LLC
- Macrosomia (High Birth Weight): Maternal obesity increases the likelihood of a baby being born with macrosomia, which is classified as any weight over 4000 grams, or about 8 pounds and 13 oz. Babies with macrosomia are at greater risk for birth injuries, including shoulder dystocia, clavicle fractures, and even asphyxia due to prolonged labor.

- Cephalopelvic Disproportion (CPD): Similar to macrosomia, cephalopelvic disproportion (or CPD) occurs when the baby’s head is too large to fit through the mother’s pelvic opening during delivery. The chances of CPD occurring increased in cases where the mother was classified as obese. If the labor is prolonged or obstructed for too long, it can result in birth injuries like cerebral palsy and hypoxic ischemic encephalopathy (HIE).

- Intrauterine Growth Restriction (IUGR): IUGR is a condition where the growth of the fetus is restricted, resulting in the body being smaller and less developed. This can be exacerbated in cases of maternal obesity, where internal hormone imbalances can contribute to low birth weight and fragility of the fetus. IUGR is a serious condition that must be caught early on to ensure the viability of the pregnancy.

- Neonatal Sepsis: Neonatal sepsis occurs in neonates as a response to infection. Mothers with maternal obesity are at a higher risk for contracting infections during pregnancy that can threaten the child’s health, with one of the most common being Group B Streptococcus and other streptococcal infections.
- Stillbirth and Preterm Birth Complications: Obesity is associated with higher risks of stillbirth and preterm birth, where birth complications such as respiratory distress syndrome and immature lung development are common. If not identified and treated immediately (and even in some cases when it is treated immediately), these birth complications can result in long-term developmental delays.

- Neonatal Hypoglycemia: If the mother has been diagnosed with gestational diabetes (which is more common in women with obesity), newborns may experience hypoglycemia (low blood sugar) after birth, which has been shown affect neurological development and increase the risk of seizures or brain injury if not promptly addressed.

Symptoms: How Can Maternal Obesity Affect The Mother?
Maternal obesity does not only jeopardize the health of the unborn child; there are multiple risk factors present for the mother, which can in turn bring further complications to her unborn baby. These risks include conditions that can occur during pregnancy, but some complications can persist post-partum. These risks include, but are not limited to:
- Gestational Diabetes: Obese mothers are at a higher risk of developing gestational diabetes, a type of diabetes common in pregnant women which can lead to increased fetal growth rates and result in macrosomia (a condition where the newborn is much larger than average). This can complicate vaginal delivery and heighten the risk of physical injury to the baby.
- Preeclampsia and High Blood Pressure: Obesity increases the risk of preeclampsia, a condition that can restrict blood flow to the placenta, which can cause fetal distress and an increased likelihood of emergency delivery. If not properly identified early on, it can lead to life-threatening consequences for a mother and her baby, including strokes and eclampsia, both of which have a high fatality rate. It can also lead to placental abruption, where the mother’s placenta is prematurely detached from the uterine lining which can cause heavy bleeding.
- Prolonged Labor and Obstructed Labor: Babies born to mothers with obesity are more likely to experience prolonged labor, increasing their risk of hypoxia (lack of oxygen) and other trauma-related injuries during birth. This can pose multiple risks to the mother, such as uterine rupture or postpartum hemorrhaging.
- Operative Delivery: Pregnant women with maternal obesity are more likely to require operative delivery interventions such as cesarean births (C-sections) or the use of external tools such as forceps and vacuum extractors. Operative delivery is sometimes referred to as “instrumental delivery” for the use of surgical instruments in the procedure. These methods increase the risk of lasting harm to the mother, and they also are associated with specific birth injuries for the newborn like skull fractures, bruising, and nerve damage.
Potential Long-Lasting Consequences of Obesity-Related Birth Injuries
For some women with maternal obesity, there can be adverse health risks that remain present for their child even after delivery. Obesity-related birth injuries can result in immediate and sometimes long-term health consequences for the newborn and the mother, including:
- Cerebral Palsy: Maternal obesity increases the risk of pregnancy complications like neonatal hypoglycemia and neonatal sepsis, which are conditions that restrict the child’s brain from receiving oxygen and other vital nutrients. Infections and a lack of proper oxygen levels are two of the highest risk factors for brain damage in newborns, which can trigger one or more neurological disorders that fall under the umbrella of cerebral palsy.
Other conditions linked to maternal obesity, such as macrosomia or cephalopelvic disproportion, can increase the odds of head trauma during delivery. Severe head trauma has been linked as a risk factor for brain damage and the onset of cerebral palsy in neonates. - Hypoxic Brain Injury: The likelihood of developing conditions such as preeclampsia, prolonged labor, and macrosomia increases when the mother is diagnosed with obesity. These conditions can deprive the child’s brain of oxygen, leading to brain injuries like hypoxic-ischemic encephalopathy (HIE).
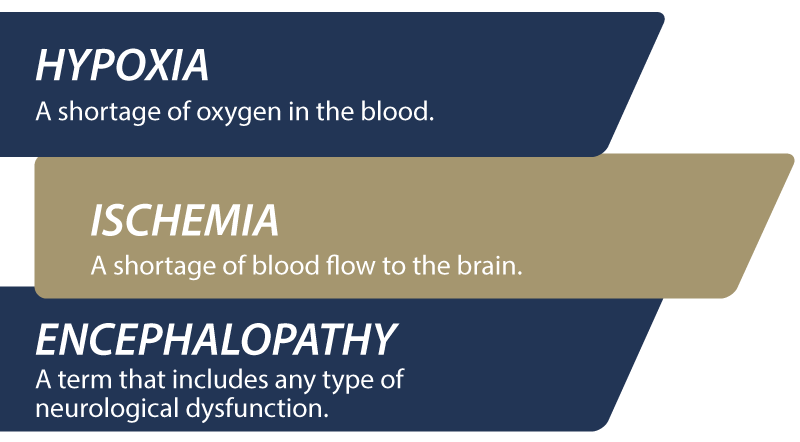
HIE is a severe birth injury that occurs when the brain does not receive adequate oxygen levels nor blood flow. This can result in a multitude of different health complications for the child, including respiratory difficulties, organ dysfunction, seizures, abnormal reflexes and low muscle tone.
Other common hypoxic brain injuries that can be caused from obesity-related risk factors include birth asphyxia, preeclampsia, periventricular leukomalacia (PVL), and injuries sustained via neonatal seizures. - Developmental Delays: During childhood, children will often display certain developmental milestones as they age. These milestones can be physical, such as the age at which a child says their first words or takes their first steps. These also include milestones for cognitive skills, such as development of hand-eye coordination and recognition of faces/objects.
However, certain birth complications can result in the delay of these milestones. Premature infants or those with hypoglycemia or brain injury may experience developmental delays and long-term cognitive impairments, which can require ongoing medical care throughout the child’s life.
The risks of these complications, including hypoglycemia and premature birth, are heightened by maternal obesity. - Nerve Damage and Paralysis: Shoulder dystocia can cause injury to the brachial plexus, where nerve damage can result in temporary or even permanent paralysis of the child’s arm. Additionally, the use of forceps or vacuum extractors, while medically necessary in some cases, also risk damage to the brachial plexus.
It’s important to note that many of these conditions can overlap with one another; for example, a child with a hypoxic brain injury or cerebral palsy is also likely to experience varying developmental delays. Each birth injury case is different and causation for a specific injury will depend on the unique circumstances surrounding the mother’s pregnancy.
Diagnosing Obesity-Related Birth Injury Risks
Healthcare providers must take extra precaution at every step when screening expecting mothers with obesity. Failure to identify specific risks pertaining to obese pregnant women can result in long term complications for both the mother and her child. It is for that reason that these procedures are critical when overseeing and caring a pregnant woman with maternal obesity:
- Prenatal Screening and Monitoring: Doctors typically assess BMI during prenatal testing at the beginning of pregnancy, and should take extra precaution monitoring women who are classified as obese. Additional tests, such as glucose tolerance testing for gestational diabetes and blood pressure monitoring, can help to identify high-risk pregnancies.
- Ultrasound and Fetal Size Estimations: Ultrasound exams are crucial in estimating fetal size and identifying conditions such as macrosomia. This information helps guide decisions on delivery method and timing to minimize injury risks.
- Non-Stress Testing and Biophysical Profiles: Pregnant women with obesity may undergo additional fetal monitoring, such as non-stress tests or biophysical profiles, to assess fetal well-being and detect any signs of fetal distress that might require early intervention. However, research suggests a higher risk of failure of certain non-invasive prenatal screenings for mothers with obesity.

How To Minimize Risks for an Obese Pregnant Woman?
Minimizing the risk of birth injury from maternal obesity can be a joint effort between healthcare providers and the mother.
- Antepartum Management: Regular prenatal visits and managing maternal conditions like gestational diabetes and hypertension are essential for women with obesity. Providers may recommend dietary modifications, physical activity, and medications (as necessary) to control blood sugar and blood pressure levels.
- Intrapartum Management: During labor, a comprehensive plan is vital to reduce birth injury risk. Techniques may include controlled delivery methods, gentle traction during vaginal delivery to avoid shoulder dystocia, and, in some cases, planned C-sections for macrosomic babies to prevent physical injury.
- Postpartum Care: After birth, monitoring the baby’s blood sugar and oxygen levels is critical, especially if the mother has gestational diabetes. Babies with signs of birth injury may require early interventions, such as physical therapy for nerve damage or specialized neonatal care for respiratory issues.
What Causes Maternal Obesity?
A variety of genetic and environmental factors can interact to result in cases of maternal obesity, some of which being outside of the mother’s control. These factors can include:
- Genetic Predispositions: Sometimes, the mutation of certain genes within the body can play a role in determining someone’s weight. Certain genes that play a factor in energy regulation or appetite, such as the Leptin Receptor Gene (LEPR), can cause deficiencies that lead to early onset obesity starting in the first months of life.
Mutations to other genes such as the melanocortin 4 receptor (MC4R), a gene affecting appetite and energy intake, can play a role as well in gaining weight and becoming obese. According to research from the National Institute of Health, the MC4R gene was found to be “the most common associated gene for childhood obesity” Other genes exist within the body that affect exercise regulation and fat storage, which can play a role in a mother’s weight. - Family History & Hereditary Traits: In some cases, a person can inherit specific genetic mutations linked to weight gain from their parents. But obesity running in a family can be attributed to more than just genetics; families who live and eat together tend to adopt the same eating habits and engage in similar lifestyles, which can explain the phenomenon of obesity presenting itself within family units.
- Hormone Imbalances: Different hormone imbalances can affect someone’s weight, with one of the most common imbalances in women being Polycystic Ovary Syndrome, or PCOS. PCOS is a hormone imbalance found in women of reproductive age where the body fails to produce the appropriate proteins needed to ovulate. In response, the ovaries develop many small fluid-filled sacs (or cysts) that can offset a woman’s normal hormonal process and disrupt her menstrual cycle.
A common symptom of PCOS is weight gain, especially around the belly, which can elevate a woman’s BMI and push her into the obese weight class. Though one of the most common, PCOS isn’t the only type of hormonal imbalance to affect a woman’s weight; resistance to hormones like insulin or leptin proteins can also trigger unintentional weight gain in expecting mothers and lead to obesity. - Lifestyle Tendencies: Dietary and exercise habits are fundamental in dictating anyone’s weight and corresponding BMI. Pregnant women increase their risk of obesity when they lead sedentary lifestyles with little to no daily movement, coupled with a diet high in simple/refined carbohydrates and processed sugars.
While it is possible for someone to do both of those things and still not be classified as obese, the overwhelming medical consensus points to these habits having adverse effects to health beyond just weight gain.
Not all cases of maternal obesity are identical; different remedies and treatments may be necessary depending on the mother’s specific health conditions.
Frequently Asked Questions For Obesity-Related Birth Injuries
Does obesity rate lead to high maternal mortality?
While it is true that maternal obesity can increase the risk of maternal and infant mortality, it is absolutely possible to be classified as obese and have a healthy pregnancy and delivery without complications. With proper specialized care, many complications and birth injuries can be avoided.
Does maternal obesity affect infant telomere length?
A telomere is a compound structure at the end of a chromosome that protects it from getting tangled. They have been associated with predicting lifespans As we age and our cells divide, the telomeres become shorter. They are longest at birth, with an average of 6000-15000 bp (base pairs). There is research to support that maternal obesity can play a role in shortening infant telomere length, but there is a variety of other factors that can influence length as well, including maternal stress, maternal folate concentrations, any history of smoking, preexisting conditions prior to pregnancy and more.
Can maternal obesity lead to decrease in fetal oxygen supply?
Yes. Different factors such as increased adipose tissue and higher odds of birth complications can threaten the oxygen supply to the fetus in cases of maternal obesity. Conditions like HIE are also more likely to occur in babies born from mothers with obesity. With the proper care, these risks can be assessed throughout the gestational period and treated appropriately should any complications arise.
Does obesity cause premature birth?
It can, yes. Maternal obesity increases the likelihood of developing gestational diabetes, hypertensive disorders and different fetal malformations. All of these can contribute to a pregnant woman going into labor prematurely. But it’s important to note that the symptoms of maternal obesity can also delay birth in some cases: higher BMI can sometimes be associated with a longer gestational period, which leads to longer term births.
What is the minimum recommended weight gain for the obese pregnant woman?
The general medical consensus is a recommended weight gain of 11-20 lbs. for mothers with a BMI of 30 or higher prior to pregnancy, which works out to about a half pound each week during the 2nd and 3rd trimesters. This can vary depending on BMI, however, so every pregnant woman should consult with their primary healthcare physician to determine how much weight gain is healthy for their specific case.
Examples of Medical Negligence in Obesity-Related Birth Injuries
It’s important to remember that every birth injury case is different. It requires a careful and thorough review of the facts of your case to determine if medical negligence truly played a factor in your child’s birth injury. However, these medical errors can be an indicator for a case of medical negligence in obesity-related birth injuries:
- Failure to diagnose maternal obesity through improper tracking of the mother’s initial weight.
- Failure to monitor the mother’s weight gain during pregnancy.
- Failure to conduct adequate ultrasound screenings during the gestational period.
- Failure to provide the mother with appropriate prenatal care and counseling on nutrition and weight gain during pregnancy.
- Failure to prescribe necessary medications to treat any of the mother’s underlying conditions that put her unborn child at risk.
- Failure to diagnose and treat gestational diabetes early on.
- Failure to identify and diagnose preeclampsia, high blood pressure or hypertension before it causes complications.
- Failure to properly monitor the baby’s growth in utero and catch any abnormalities.
- Failure to perform an emergency c-section in time should the mother require one from a failed attempt at vaginal birth after c-section (VBAC).
- Prolonged wait time during labor in the event of an emergency such as hemorrhaging, uterine ruptures, placental abruption, or complications from macrosomia, cephalopelvic disproportion (CPD), or intrauterine growth restriction (IUGR).
- Misuse of external tools like forceps and vacuum extractors during instrumental delivery, resulting in preventable trauma to the newborn.
- Failure to follow up with appropriate post-partum care for neonates such as care for nerve damage or respiratory issues.
Was My Child’s Obesity-Related Birth Injury the Result of Medical Malpractice?

Birth injuries related to maternal obesity may sometimes be preventable with proper medical care. Medical negligence, such as failure to monitor maternal or fetal health adequately, missed diagnoses of gestational diabetes, or poor management of prolonged labor, can increase the risk of preventable birth injuries.
If a family believes medical negligence contributed to their child’s birth injury, legal support may be an option. A knowledgeable birth injury attorney can review the medical records and circumstances to assess whether a claim exists.
Parents whose children suffer from related complications as well as parents who have suffered the loss of their baby due to obesity-related birth injuries deserve to know whether the complications resulting from it were preventable. Our dedicated birth injury lawyers want to help you find those answers and obtain the funds necessary to purchase devices that can help improve the quality of your child's life.
If your child has been diagnosed with a birth injury related to maternal obesity and you suspect this may have been caused in part by medical mistakes, Miller Weisbrod Olesky will thoroughly investigate the facts and hold responsible medical providers accountable by pursuing medical malpractice claims against them.
Sometimes families are hesitant to reach out to a medical malpractice attorney or law firm. Parents may feel overwhelmed by their circumstances or are worried that a law firm will not be able to help them. But the only way to find out if you have a case is to talk to an attorney who understands how birth injuries can lead to developmental delays and other complications that require long-lasting medical support.
Statute of Limitations in a Birth Injury Lawsuit
A statute of limitations (SOL) is a law that sets a time limit on how long an injured person has to file a lawsuit after an accident. It is essential to understand that statutes of limitations vary based on the type of case and the state where it is filed. For instance, the deadline for birth injury claims is typically different from other claims, such as injury to personal property, fraud, contract disputes, and collection of debts.
Generally, the clock starts ticking on the date the injury occurred. However, there are exceptions to this rule, and in some cases, the statute of limitations starts when a person discovers or reasonably should have discovered an injury. When dealing with government agencies, SOLs can become even more complex.
For example, if the party that injured you was:
- A federal employee
- Employed by a military hospital, Veterans Administration facility, or a federally funded medical entity
You may need to file a birth injury claim under the Federal Tort Claims Act (FTCA). In FTCA cases, claimants must go through certain administrative procedures before filing a lawsuit. In some states, if the negligent party was a local or state government hospital or the doctors and medical providers are employees of a governmental entity, the time period in which you must give "notice" may be shorter.
If your case is filed outside of the statute of limitations, it will typically be dismissed, and you will not be eligible to recover compensation for your injuries. Determining when a statute of limitations begins on your case can be tricky. If you're considering pursuing compensation for a birth injury, contacting an attorney as soon as possible is in your best interest.
How The Birth Injury Attorneys at Miller Weisbrod Olesky Can Help?

Obesity-related birth injuries are preventable in many cases, but it takes a detailed expert review of the facts and circumstances of your child's birth to determine whether the birth injury was the result of medical malpractice.
At Miller Weisbrod Olesky, a team of committed attorneys, nurses and paraprofessionals uses our detailed medical negligence case review process to assess your potential birth injury case. We start by learning more about you and your child and the status of meeting/missing developmental milestones. Then we gather medical records to determine what happened before, during, and after your delivery. We call in skilled medical experts who review your records and let us know if they think medical errors could have caused your child's injuries.
If we feel medical negligence caused or contributed to your child's injuries, we meet with you to discuss how you can receive compensation from the medical professionals who made the
errors.
At no point in our legal intake process will we ask you to pay anything. The medical review of your case and the consultation are free. We only receive payment when you do. The sooner you reach out to us, the sooner we can begin investigating your case and gathering the evidence needed to support your claim.
We work on a contingency fee basis, meaning you won't pay any legal fees unless we win your case. Contact us today to schedule your free consultation by calling our toll-free line at (888) 987-0005 or by filling out our online request form.
Contact Miller Weisbrod Olesky
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.