Fetal Bradycardia
Fetal Bradycardia During Labor
Certain heart rate changes in an unborn baby are critical indicators of their health condition. The general medical consensus is that a “normal” fetal heart rate (FHR) rests within 110-160 beats per minute (bpm).
Anything exceeding this range is a fast heart rate (“tachycardia”), and anything below it is a slow heart rate (“bradycardia”). Abnormal fetal heart rates can be the first signs of serious health risks in the womb.
Bradycardia Fetal Heart Rate Strip
A baby with fetal bradycardia may be suffering from oxygen deprivation. Babies on the verge of hypoxia will naturally lower their heart rate to conserve oxygen. A prolonged baseline heart rate below 110 bpm indicates that the baby is in fetal distress.
Doctors, nurses, and all other present healthcare providers must carefully monitor fetal heart rates during pregnancy and during labor. If they fail to respond to concerning heart rate patterns like bradycardia, the baby can suffer from hypoxic brain injuries.
The lower the baby’s heart rate during pregnancy, the higher the risk of brain injuries like hypoxic ischemic encephalopathy (HIE). HIE is permanent brain damage at birth that stems from reduced oxygenated blood flow to the baby before birth. It can cause neonatal seizures, vision impairments, speech impairments, and other delayed developmental milestones. HIE is the leading cause of cerebral palsy in early childhood.
A medical professional’s delayed reaction to fetal distress during delivery counts as medical malpractice when it causes preventable birth injuries.
Birth Injury Malpractice Attorneys
Our top rated birth injury attorneys specialize in identifying how oxygen deprivation during delivery can lead to severe brain injuries. If your baby suffered from fetal bradycardia at birth, don’t hesitate to contact our firm. We can answer difficult legal and medical questions and investigate the facts on your behalf.
Free Legal Consultation
Birth Injury Lawyers
(888) 987-0005Our Birth Injury Lawyers are available to meet you in your home or the hospital.
Our vast network of medical experts and in-house nursing staff and nurse-attorneys gives us the edge over our competition. When we take your case, we assign you with not just an attorney but an entire medical team. This team includes attorneys, experienced nursing advocates, and seasoned medical experts.
Your team is available to assist with any day-to-day treatment you or your child may need. This includes assistance with obtaining medical records, scheduling doctors’ appointments, providing transportation, and any other problems that may arise.
We offer all of this on a contingency fee basis. This means you will not pay any fees until after we win your case and secure a settlement. Miller Weisbrod Olesky’s unmatched track record of birth injury results sets us apart from other birth injury law firms.
Recent Birth Injury Settlement:
Birth Injury settlement against a hospital in which nurses and physicians failed to properly monitor the mother's blood pressure during delivery causing an HIE event resulting in neonatal seizures and cerebral palsy at birth. Our team of top-rated birth injury lawyers recovered $13,750,000 for the family to help with future medical expenses and developmental therapy.
What is Fetal Bradycardia?

Bradycardia is the medical term to describe an abnormally low heart rate. Fetal bradycardia is a type of arrhythmia (slow and irregular heart rhythm) which could affect the fetus’s health during pregnancy. It is one of the most common indicators that the baby is suffering from fetal distress.
In modern day medicine, doctors can use an electronic fetal monitor to observe the baby’s heart rate prior to delivery. The machine will produce strips that show the number of beats per minute (bpm) of the baby’s heart. Obstetricians and nurses can determine if a baby is suffering from bradycardia from those strips.
What Are the Types of Fetal Bradycardia?
There are several types of fetal bradycardia. The medical team can diagnose the specific fetal bradycardia based on the echocardiogram (ECHO) measurements and atrioventricular (AV) conduction patterns.
“Atria” re the heart’s upper chambers and “ventricles” are the lower chambers. A “heart block” occurs when electrical signals that produce heartbeat do not travel normally from the atria to the ventricles.
Sinus Bradycardia
Sinus bradycardia occurs when the heart’s atria and ventricles beat in sync, but the heart rate is consistently slow.
- Transient Sinus Bradycardia: Brief bradycardia episodes lasting 1-2 minutes and often occur because of increased vagus nerve stimulation (VNS). The vagus nerve in the nervous system controls the heartbeat. Transient sinus bradycardia usually happens in second trimester when the fetal nervous system is relatively immature.
- New-onset Sinus Bradycardia: A consistently slow heartbeat that suddenly develops after having a previously normal heart rate. This condition indicates that some sort or complication occurred that led to severe hypoxia and fetal distress. Some possible complications that can cause new-onset sinus bradycardia include uterine rupture, placental abruption, umbilical cord prolapse, and fetal hemorrhage.
- Sinus Node Dysfunction: A slow heartbeat stemming from improper functioning of the sinus node. Located in the right upper heart chamber, the sinoatrial node is the heart’s natural pacemaker that controls the heart rhythm. Babies with structural heart disease are at a higher risk for sinus node dysfunction leading to bradycardia.
Blocked Premature Atrial Contractions
A fetal premature atrial contractions (PACs) are “extra” heartbeat that occurs outside of the sinoatrial node. The extra beat starts in the atria chambers, but the atrioventricular (AV) node blocks it. This means the heartbeat never reaches the ventricles. When repeated, the “missed” heartbeats occurring from this condition can manifest as fetal bradycardia.
The diagnosis may become complex when the ectopic heartbeats occur at a regular rate, resulting in a “regularly irregular” heart rhythm. It’s important that medical providers differentiate between blocked premature atrial heartbeats and AV heart block condition. The two conditions have different prognoses and treatment options.
Atrioventricular (AV) Heart Block
Congenital heart block (CHB) or AV heart block is one of the commonly occurring forms of fetal bradycardia. This condition can lead to developmental delays or even fetal demise when intervention doesn’t happen soon enough. Up to 70% of the babies with this condition will require a pacemaker after birth.
Medical experts believe that placental transfer of maternal antibodies (Ro and La antibodies) is what causes this form of bradycardia. The antibodies cross the placenta and injure the fetal heart’s electrical conduction system, which causes heart tissue damage.
Doctors generally diagnose fetal CHB during pregnancy at around 18 to 24 gestational weeks using fetal echocardiogram (ECHO) techniques. It’s noteworthy that congenital heart block condition can be dynamic, meaning its severity can fluctuate throughout the mother’s pregnancy. Some babies may exhibit a normal or first-degree atrioventricular interval (gap between heartbeats) during initial prenatal testing. However, the same baby may develop second-degree or complete heart block later into the pregnancy.
Babies with severe CHB will show a substantially lower heart rate of around 50 to 70 bpm. In these cases, the risk of intrauterine death, fetal heart failure, premature delivery, and edema is high.
What Causes Fetal Bradycardia During Labor?

A variety of conditions may cause fetal bradycardia during labor. Slower fetal heart rates typically stem from a lack of sufficient oxygen (known as hypoxia) during delivery. The baby could have restricted access to oxygen for a number of reasons, including:
Uterine rupture
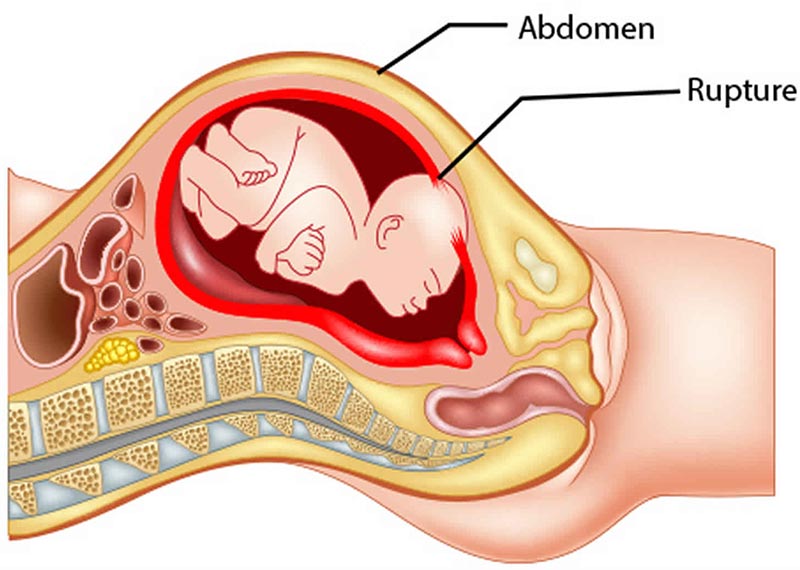
A uterine rupture occurs when there is a tear in the wall of the uterus. This condition usually occurs at the site of a previous C-section or previous uterine surgery.
A uterine rupture can dramatically affect the baby’s oxygen supply and put them into fetal distress.
Placental Complications

The placenta plays a critical role in fetal gas exchange. It absorbs oxygen from the mother’s blood and transfers oxygenated blood and nutrients to the baby through the umbilical cord.
A damaged placenta can disturb this process. Complications like a placental abruption or uteroplacental insufficiency can leave the baby with diminished levels of oxygen. Prolonged periods with low oxygen can force the baby’s heart to conserve energy by beating slower.
Umbilical Cord Complications

The baby receives all its oxygen and nutrients through the umbilical cord. The cord is also the baby’s route for discarding carbon dioxide and other waste products.
Umbilical cord complications like compression or a nuchal cord can prevent sufficient levels of oxygen from reaching the fetus. If a baby goes too long without a functioning umbilical cord, the resulting oxygen deprivation can lower their heart rate.
Prolonged Labor

Doctors will typically call a mother’s labor “prolonged” when it lasts past 18-20 hours. An arrested labor is one that ceases to progress at all.
A baby has weaker access to oxygen after the mother’s water breaks and labor begins. The longer labor lasts, the greater the baby’s risk is for birth asphyxia and hypoxia. Prolonged oxygen deprivation can affect fetal heart rates and lead to bradycardia.
Excessive Uterine Contractions

Just like with a prolonged labor, excessive uterine contractions (tachysystole) can restrict the baby’s access to oxygen and blood flow. Going too long without oxygenated blood can result in severe hypoxic and ischemic (lack of blood flow) injuries.
The baby’s heart rate may dip and stay dangerously low in response to the lack of oxygenated blood flow.
Oligohydramnios

Amniotic fluid surrounds the baby inside the womb. It serves multiple purposes like temperature regulation, organ development, and allowing for fetal movement and repositioning.
Too little amniotic fluid (oligohydramnios) can increase the risk of complications like umbilical cord compression. This can affect the flow of oxygenated blood and put the baby in fetal distress.
Abnormal Fetal Position

When the baby is in an abnormal fetal position, it increases the risk of complications that threaten their oxygen supply. These complications include prolonged labor, umbilical cord compression, and emergency C-section.
Depending on the severity, these complications can cause hypoxia and put the baby into a state of fetal distress. Prolonged fetal distress can lower the baby’s heart rate to a dangerous level.
About Abnormal Fetal Positions
Size Of The Baby

When the baby weighs more than 9 lbs., it may become more difficult to traverse through the mother’s birth canal. This can prolong or arrest labor and increase the risk for oxygen deprivation and subsequently slower heart rates.
Other size complications like cephalopelvic disproportion (when the baby’s head doesn’t fit through the birth canal) can have similar outcomes.
It is critical that doctors monitor all babies during the labor and delivery process. They must utilize electronic fetal monitoring equipmentto detect whether or not bradycardia or another concerning pattern is occurring. Medical professionals should move to immediate delivery by emergency c-section in cases where:
- They don’t know the cause of the baby’s bradycardia
- The baby’s bradycardia is persistent
- Other intervention measures are not helping
- The baby has new-onset sinus bradycardia
Degrees of Severity in Fetal Bradycardia
Heart rate 100 to 120 bpm
Bradycardia in this range with normal variability is more common in post-term pregnancy (lasting more than 42 weeks). It is also common in fetuses with transverse or occiput posterior presentations.
Heart rate 90 to 100 bpm
A fetus with this degree of bradycardia has a much higher risk of suffering from hypoxia and ischemia. This non-reassuring pattern of bradycardia can be a sign of myocardial conduction defects or other congenital heart abnormalities.
Heart rate 90 bpm or lower
The chances of miscarriage are very high in this heart rate range. Bradycardia of less than 80 bpm which lasts for at least three minutes is an indication of severe hypoxia. If these babies survive, they are likely to sustain severe hypoxic-ischemic injuries like HIE.

How to Diagnose Fetal Bradycardia
Early diagnosis as well as differential diagnosis (differentiating between two conditions with similar symptoms) is vital to the baby’s survival.
Internal Fetal Monitoring (IFM)

Doctors may use internal fetal heart monitoring during labor when the cervix is open after the amniotic sac breaks. The medical team will put a thin electrode on the baby’s scalp through the cervix. One end of the electrode connects to a monitor.
Readings with this method are incredibly reliable and may prove useful when external monitoring fails to provide a concrete measurement. Medical providers should monitor heart rates and uterine contractions simultaneously and compare the results for a more accurate diagnosis.
External fetal monitoring should occur as soon as healthcare professionals admit an expectant mother with labor. This type of electronic fetal monitoring will provide important information about the fetal heart rate during early labor.
Fetal Echocardiogram

Fetal echocardiography is quite similar to an ultrasound test. It helps the medical providers see the heart’s structure and function in the unborn baby. This exam normally occurs during prenatal testing between 18 and 24 gestational weeks (in the second trimester). The test utilizes sound waves, which produce an “echo” off the fetal heart structures.
A fetal echocardiogram (fetal echo) can establish a fetal bradycardia diagnosis. Doctors perform a fetal echocardiogram to evaluate the fetal heart structure and diagnose potential structural defects.
To identify the specific form of fetal bradycardia, the medical team should assess the cardiac conduction pattern. The heart conduction system includes conducting fibers and cardiac cells that initiate impulses that travel rapidly through the baby’s heart.
Analysis of the echocardiogram images can provide useful information about the fetal heart formation and how it is functioning. A detailed look at the fetal echo images will also help the medical team identify abnormalities in blood flow. This can sometimes be the cause of the baby’s abnormal heartbeat.
Fetal Ultrasound

A Doppler ultrasonography is a non-invasive test used to diagnose fetal bradycardia. Unlike the standard ultrasound test, a Doppler ultrasound can estimate the blood flow through the baby’s blood vessels. It bounces ultrasound waves off circulating red blood cells to indicate congenital heart disease, heart valve defects, and fetal bradycardia.
Abnormal ultrasound findings (fetal heart rates below 100-120 bpm) could be an early indicator of potential miscarriage.
Laboratory Studies

Lab tests are essential to diagnose congenital AV heart block type of fetal bradycardia. Two antibody tests in this regard are anti-Ro (SSA) and anti-La (SSB) tests. These tests identify the presence of anti-Ro and anti-La antibodies, which can cause third-degree AV block (congenital heart block).
When the mother has a connective tissue disorder, the fetus is a higher risk of developing CHB. Nine out of 10 mothers with fetuses with CHB will test positive for anti-Ro and anti-La antibodies.
Diagnosing fetal bradycardia is of paramount importance in order to prevent fetal mortality. When the fetal heart rate measurements are abnormal, the medical team should consider urgent interventions. This may include changing the mother’s position, providing supplemental maternal oxygenation, and administering IV fluid.
How to Treat Fetal Bradycardia?

The labor and delivery medical team’s response to abnormal fetal heart rates can mean the difference between life and death. Healthcare professionals must quickly intervene when they suspect a baby has bradycardia to avoid adverse neonatal outcomes.
Antepartum Management
Proper antepartum (before birth) management will depend on the specific form of fetal bradycardia the baby has:
- Fetal Sinus Bradycardia: If the condition results from hypoxia or fetal distress, doctors should consider urgent delivery. If the sinus bradycardia continues after birth (pediatric sick sinus syndrome), doctors may use defibrillators, beta blockers, and/or pacemakers.
- Congenital Heart Block (CHB): Fetal structural heart conditions aren’t possible to treat in-utero. However, doctors may use intravenous immunoglobulin (IVIG 400 mg/kg) or beta blockers to improve heart rates in cases of CHB. They may also consider using fluorinated steroids (dexamethasone 4 mg per day).
Intrapartum Management
When fetal bradycardia occurs, nurses and doctors must immediately take actions to correct it.
Intrapartum fetal monitoring is critical to identify bradycardia that could lead to hypoxic ischemic encephalopathy (HIE) or even fetal mortality. Continuous electronic fetal monitoring (EFM) can help the medical team decide when to intervene. In the most severe cases, doctors may need to conduct an emergent c-section delivery or an instrumental vaginal delivery. Timely action may reduce the risk of neonatal seizures, cerebral palsy, and neonatal death.
In the event of abnormal electronic fetal monitoring tracings, the following interventions may help medical staff avoid a C-section:
- Changing the maternal position
- Administering IV fluids
- Evaluating maternal vital signs (pulse, blood pressure and temperature)
- Discontinuing labor inducing infusions, if any
- Initiating oxygenation at 6 to 10 LPM (liters per minute)
- Carrying out a vaginal examination (to determine umbilical cord prolapse, postpartum hemorrhaging, or rapid descent of the fetal head)
- Performing a fetal scalp stimulation test
- Administering amnioinfusion (instilling of fluid into amniotic cavity) in case of variable and recurrent decelerations
Postpartum Management
In the postpartum phase, doctors must discontinue any medical therapy they started during labor to treat the fetus. If the mother has a connective tissue disorder, she should follow up with a rheumatologist or her primary care physician. That disorder can sometimes be the initial cause of a congenital heart block that results in bradycardia.
Babies with fetal bradycardia who aren’t breathing at birth will require urgent neonatal resuscitation. If the baby appears to have brain damage, medical staff should admit them into the neonatal intensive care unit. From there, neonatal nurses and other medical professionals can determine the next steps such as therapeutic hypothermia treatment.
What Are the Consequences of Fetal Bradycardia?
Undiagnosed or untreated fetal bradycardia may lead to serious long-term effects. The fetal or neonatal outcomes may include nerve damage, brain damage, paralysis, cerebral palsy, and in some instances even death.

Consequences will depend on the baby’s gestational age, any existing congenital heart defects, and the timing of diagnosis and treatment.
Fetal bradycardia can be one physiological sign of brain injuries like HIE. Babies with these types of injuries have a high likelihood of receiving a cerebral palsy diagnosis later in childhood.
Children who experience brain damage at birth from prolonged asphyxia may also experience developmental delays. They may rely on assistive equipment and devices such as wheelchairs, walkers, and communication devices.
These children will also require varying levels of birth injury treatment throughout their lives. Children with cerebral palsy typically benefit from physical therapy, speech therapy, and occupational therapy to enhance their gross motor function.
Children who survive prolonged bradycardia may still be at the risk for needing a pacemaker after birth or in childhood. Having a pacemaker requires regular scheduled appointments where doctors can evaluate its functioning and look for any issues like displacement.
Pacemakers can also limit a child’s participation in some activities. It may make them ineligible for contact sports or using certain electronics.
Did Doctors Miss or Mismanage My Child’s Bradycardia?

Fetal bradycardia can cause brain injuries like HIE and other neurological outcomes that will forever alter a child’s life. Birth injury negligence, like delaying a C-section amid fetal distress or delaying therapeutic hypothermia after birth, increases the baby’s risk.
If a family believes medical negligence worsened a child’s brain damage at birth, legal support may be an option. A specialized birth injury attorney can review the medical records and circumstances to assess whether a claim exists.
Families who have experienced the effects of brain injuries from negligent medical care deserve to know whether they were avoidable. Our top rated birth injury lawyers will help you find those answers and obtain the necessary funds to secure treatment.
Our National Birth Injury team will thoroughly investigate the facts, holding responsible parties accountable by pursuing medical malpractice claims.
What is the Statute of Limitations in a Birth Injury Lawsuit?
A statute of limitations (SOL) is a law that sets a time limit on how long an injured person has to file a lawsuit after an accident. It is essential to understand that statutes of limitations vary based on the case and the state where you file. For instance, the deadline for birth injury claims is typically different from other claims, such as injury to private property.
Generally, the clock starts ticking on the date the injury occurred. However, there are exceptions to this rule. In some cases, the statute of limitations starts when a person discovers or reasonably should have discovered an injury. When dealing with government agencies, SOLs can become even more complex.
For example, if the party that injured you was:
- A federal employee
- Employed by a military hospital, Veterans Administration facility, or a federally funded medical entity
You may need to file a birth injury claim under the Federal Tort Claims Act (FTCA). In FTCA cases, claimants must go through certain administrative procedures before filing a lawsuit. In some states, you may have less time to give notice if:
- The negligent party was a local or state government hospital
- The doctors and medical providers are employees of a governmental entity
If you file your case outside of the statute of limitations, the court will typically dismiss it. This means you will not be eligible to recover compensation for you or your child’s injuries.
Determining when a statute of limitations begins on your case can be tricky. If you are considering pursuing compensation, contact a birth injury attorney as soon as possible.
How Can Our National Birth Injury Attorneys Help?

Doctors can sometimes prevent adverse neonatal outcomes by taking quick action in response to non-reassuring fetal heart rates. Fetal bradycardia is survivable in many cases and does not always lead to permanent injuries. However, it takes an expert review of the facts of your birth to determine whether medical professionals made preventable errors.
Our Process
Our team of committed attorneys, nurses and paraprofessionals works to answer these questions and seek compensation. We use our detailed medical negligence case review process to assess your potential birth injury case.
We start by learning more about your pregnancy by gathering records to determine what happened during and after your delivery. This includes evaluating the fetal heart rate strips during labor and the actions medical professionals took or failed to take.
We will call in skilled medical experts who review your records and provide insight into where medical professionals went wrong. If we feel medical negligence caused or worsened your baby’s bradycardia, we meet with you to discuss further.
At no point in our legal intake process will we ask you to pay anything. The medical review of your case and the consultation are free. We only receive payment once you do. The sooner you reach out, the sooner we can investigate your case and gather the evidence to support your claim.
We work on a contingency fee basis, meaning you will not pay any legal fees until we win your case. We do not purse any medical malpractice cases unless we fully believe we can win.
Contact us today to schedule your free consultation by calling our toll-free line at (888) 987-0005. You can also reach us by filling out our online request form.
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.

