Polyhydramnios
What Is Polyhydramnios?
Polyhydramnios is a pregnancy complication in which an excessive volume of amniotic fluid accumulates around the baby, increasing the risks of birth complications and birth injuries. Polyhydramnios can cause birth complications, such as premature birth, umbilical cord prolapse, premature rupture of membranes (PROM), and breech presentation.
In severe cases, especially if polyhydramnios is left undiagnosed or untreated, it can cause hypoxic-ischemic encephalopathy (HIE), which may lead to cerebral palsy.

Mild vs. Severe Polyhydramnios
Polyhydramnios is classified as “mild” when the build-up of excess amniotic fluid is relatively small and the amniotic fluid index (AFI) ranges between 8-11 cm. (AFI is the sum of the vertical diameter of the deepest pocket in the four quadrants of the uterus.) When the AFI value is found between 12 and 15 cm, it is clinically termed as “moderate” polyhydramnios.
Milder cases of polyhydramnios usually first occur during the third trimester, but the condition may sometimes develop in the second trimester – as early as 16 or 17 weeks of gestation. Severity of polyhydramnios is generally higher when it occurs early in the pregnancy.
When the AFI value ranges exceed 16 cm, it’s defined as severe polyhydramnios. The higher the volume of excess amniotic fluid, the greater is the severity of polyhydramnios. Higher volume indicates greater severity because it causes the uterus to swell excessively, creating too much pressure both within the uterus and on the external wall. This can create physical symptoms in the expectant mother, such as:
- Abdominal pain or discomfort
- Persistent heartburn
- Maternal shortness of breath (respiratory distress)
- Chronic swelling in the legs, feet, and ankles
- Swelling in the vulvar region
- Difficult in urination
Birth Complications for the Baby with Severe Polyhydramnios
- Premature rupture of membranes (PROM)
- Premature birth
- Placental abruption (placenta separates from the uterine wall before delivery)
- Umbilical cord prolapse (the cord drops into the vagina through the open cervix before the baby enters the birth canal)
- Fetal malposition (unusual position of the baby in the womb (such as breech or transverse)
- Fetal macrosomia (baby’s size is abnormally large for their gestational age)
All of these potential birth complications of severe polyhydramnios increase the baby’s risk of birth injuries, such as hypoxic-ischemic encephalopathy (HIE), which can lead to cerebral palsy.

Diagnosing Polyhydramnios
In addition to the physical symptoms, the medical provider should be alert to clinical symptoms that may be present and can be detected on examination. An ultrasound exam can provide an accurate measurement of the volume of amniotic fluid. The volume may be measured as amniotic fluid index (AFI) or as maximum vertical pocket (MPV). MPV measures the single deepest vertical pocket of amniotic fluid in the uterus.
Other tests that can help diagnose polyhydramnios include:
- Glucose Challenge Test: If the expectant mother has gestational diabetes, the risk of polyhydramnios is higher. Therefore, the results of this test should be correlated with other findings to diagnose polyhydramnios.
- Fetal heart rate monitoring: When polyhydramnios is suspected, FHR monitoring must be performed to assess the rate and rhythm of the baby’s heartbeat to evaluate if the baby is experiencing fetal distress.
- Doppler Ultrasound: This test will help the medical provider evaluate and study the blood flow patterns in the umbilical cord, placenta, uterus, and parts of the baby’s body. Abnormal circulation may indicate polyhydramnios, if correlated with other findings.
- Biophysical Profile (BPP): This test usually combines an ultrasound with nonstress test to provide more information about the baby’s movement, breathing and tone. It can also help assess the uterine volume of amniotic fluid.
- Nonstress Test (NST): Closer monitoring of the baby is necessary when polyhydramnios is suspected. This non-invasive test will help the medical provider evaluate how the baby’s heart rate changes or responds when the baby moves or experiences stimulation.
- Blood Tests: Maternal infections, such as Group Strep B and certain viral infections may be the cause of polyhydramnios in some cases. Therefore, when this condition is suspected, blood tests to diagnose maternal infections should be performed.
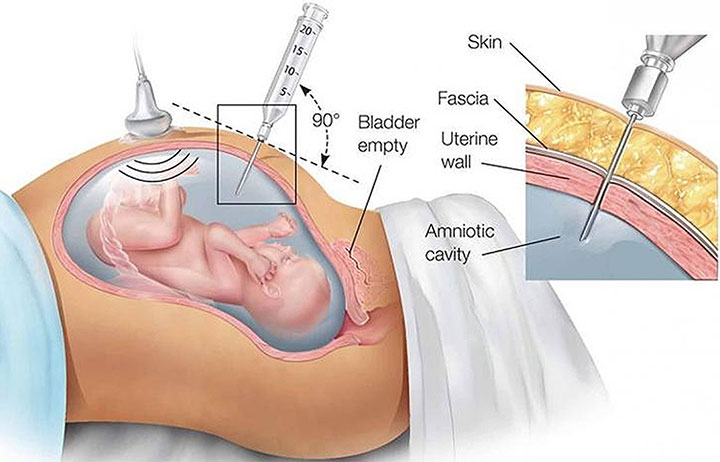
- Aminocentesis: If polyhydramnios is strongly suspected, the medical provider may decide to assess the baby for fetal anemia (insufficient red blood cells), which can cause polyhydramnios. This may require aminocentesis or direct fetal blood sampling. Rh-factor is also a special type of fetal anemia, which can lead to polyhydramnios.
Managing Polyhydramnios
When severe polyhydramnios is diagnosed, the medical provider should consider a procedure called amnioreduction depending upon when in the pregnancy this occurs. This procedure may be performed using vacuum assisted devices, such as vacuum bottles or tubing, or even manually.
Depending on the clinical status, performing a amnioreduction varying volumes of excessive amniotic fluid may be removed at specific rates using needles of 18 or 20 gauge. Even after the procedure, the medical team should continue to monitor the condition because polyhydramnios may recur after amnioreduction.
The medical provider may decide to administer Indomethacin, an oral medication, which can help reduce the amniotic fluid volume as well as fetal urine output. This treatment should not be prescribed beyond 31 weeks of gestation.
Close fetal heart rate monitoring is essential when the expectant mother is on Indomethacin treatment. The potential risks of fetal complications with this medication should be carefully balanced against the potential benefits before the treatment is prescribed.

Researchers have highlighted the increased risks of vaginal delivery and labor complications in cases of mild, moderate, or severe polyhydramnios. Therefore, medical providers should be prepared for the significant likelihood of a planned or emergency cesarean section in these cases.
Planning for the newborn’s care with a neonatologist is equally important, including possible admission to the neonatal intensive care unit (NICU) in all cases of polyhydramnios.
Is Your Child’s Birth Injury the Result of Medical Malpractice?
Parents whose children suffer from polyhydramnios related birth injuries or birth complications want and deserve answers as to cause of their child’s injury and whether mistakes by the doctors and nurses contributed to the injury.
- Were there signs of polyhydramnios during the pregnancy, labor, and delivery process, or presence of risk factors, which were either not recognized or properly treated?
- Did the medical team fail to order a series of tests to diagnose polyhydramnios in a timely manner?
- Was the decision to perform a cesarean delivery delayed?
- During the labor and delivery, were there clear indications that their baby was suffering from fetal distress, but appropriate actions were not taken by the obstetrician or nurses?
- Did the neonatal resuscitation team delay in providing important breathing support after birth?
- Were serious neonatal conditions like hypoglycemia or jaundice missed or treated incorrectly?
- Should brain cooling (also called “hypothermia therapy”) have been offered to your baby, but the doctors and nurses failed to perform the appropriate tests or ignored the results of the tests?
The proven and dependable birth injury lawyers at Miller Weisbrod Olesky, who have been through the legal minefields before, will help you determine if mistakes of the medical providers caused a birth injury to your child, including Hypoxic-Ischemic Encephalopathy (HIE) or cerebral palsy.
Our birth injury attorneys have represented families all over the United States in their time of need after a birth injury. We use our experience and expertise to obtain you and your child a medical malpractice settlement that will help provide specialized medical therapy to maximize the quality of life and independence of your child throughout their life.
Sometimes families are reluctant to contact a medical malpractice lawyer. It’s also not uncommon for parents to feel overwhelmed by the responsibilities they encounter in caring for their injured child and worried that they will not be able to help out in a lawsuit involving their child’s birth injury. Our birth injury attorneys and nursing staff will address these hesitations and concerns, so you can focus on your child and maximizing their care.
Registered Nurses and Nurse-Attorneys Are a Vital Part of Our Birth Injury Team…and Yours

Most birth injury law firms will employ one or two nurses to assist the review of cases and medical research. But Miller Weisbrod Olesky offers an unmatched number of nurses and nurse-attorney employees support to both the birth injury attorneys and our clients.
Our team of registered nursing staff and nurse-attorneys bring a deep level of medical and personal insight to every client’s case. Our nursing team includes both an experienced labor and delivery nurse as well as an ICU nurse. Working closely with the rest of the team, they investigate the reasons behind a birth injury and how medical professionals breached their standard of care.
Why Should You Talk with the Knowledgeable Attorneys at Miller Weisbrod Olesky?

The only way to find out if you have a birth injury case is to talk to a lawyer experienced in birth injury lawsuits. It’s not uncommon that a birth related complication results in a preventable birth injury, including cerebral palsy, but it takes a detailed expert review by a birth injury attorney of the medical records from your child’s birth to determine if the birth injury was the result of medical malpractice.
At Miller Weisbrod Olesky, a team of committed lawyers, nurses and paralegals uses our detailed medical negligence case review process to assess your child’s potential birth injury case. We start by learning more about you and your child and the status of meeting/missing developmental milestones. Then we gather medical records to determine what happened before, during, and after your delivery. We call in skilled medical experts who review your records and let us know if they think medical errors could have caused your child’s injuries.
If we feel medical negligence caused or contributed to your child’s injuries, we meet with you to discuss how you can receive compensation from the medical professionals who made the errors. Our birth injury attorneys have recovered millions of dollars in settlements for families of children that have suffered a birth injury.
At no point in our legal intake process will we ask you to pay anything. The medical review of your case and the consultation are free. We only receive payment when you do.
Contact Our Birth Injury Lawyers
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.