Pregnancy Complications
Complications of Pregnancy
During pregnancy, an expecting mother’s body undergoes incredible changes to support her child’s development in the womb. In the roughly 40 weeks it takes for her baby to grow to term, she will experience alterations to her physical appearance, her hormone levels, her mental and emotional state, and more.

During this time, the expecting mother becomes vulnerable to several health risks that can threaten her and her child’s wellbeing. These risks range in severity, but it is critical for doctors, nurses, and everyone else on her healthcare team to account for them. This can be done through sufficient prenatal testing, identifying and treating any issues that arise, and regular monitoring of the mother’s and the child’s status and symptoms throughout the gestational period.
When trained healthcare professionals make preventable medical errors in diagnosing, treating, or following up on a mother’s pregnancy complications, it can threaten the viability of her pregnancy and lead to birth complications or even a birth injury. When these injuries (or even fatalities) are the result of negligence, it is considered medical malpractice.
Free Legal Consultation
Birth Complication Lawyers
(888) 987-0005Our Birth Injury Lawyers are available to meet you in your home or the hospital.
Miller Weisbrod Olesky has a decades-long proven track record of results for children and families across the United States who have suffered from all types of improperly-treated pregnancy complications. Our team of specialized birth injury attorneys and registered nurses can review the unique circumstances of you or your family’s case to deliver the treatment, care, and financial resources you deserve. You won’t be charged with any fees until we win your case.
What Are Common Pregnancy Complications?
Preeclampsia
Preeclampsia is a severe pregnancy complication that arises during pregnancy usually in the later stages. It is primarily characterized by sudden high blood pressure that usually appears after 20 weeks and often near the end of a woman’s pregnancy. Other symptoms include proteinuria (protein in the urine) and visual changes (seeing spots).
When mismanaged or left untreated, preeclampsia can progress into eclampsia, which has serious related birth complications such as breathing difficulties and seizures. Preeclampsia can also progress into a condition called HELLP syndrome (an acronym for Hemolysis, Elevated Liver Enzymes, Low Platelet counts). This condition was once thought of as a more severe form of preeclampsia and is linked to higher rates of maternal mortality.
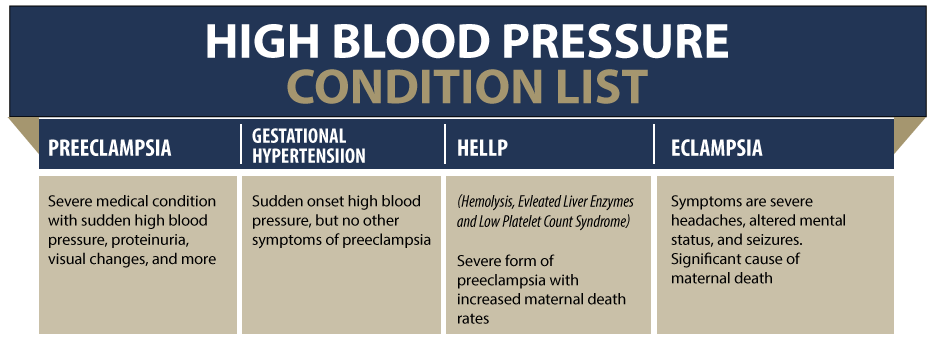
Preeclampsia can be caught through adequate prenatal testing and blood pressure checks. For a woman with previously normal blood pressure, “high” might mean a systolic reading of 140 or more or a diastolic of 90 or more (≥ 140/90 mmHg). For women with pre-pregnancy chronic high blood pressure, a systolic reading of 160 or more over 110 or more diastolic (≥ 160/110 mmHg) is considered a sudden onset high blood pressure.
Generally, healthcare providers should take blood pressure readings on two separate occasions at least four hours apart to ensure the accuracy of the high reading. They may also test the mother’s urine for proteins to diagnose preeclampsia.
Healthcare professionals must closely monitor an expecting mother with preeclampsia to ensure it does not progress into a more severe hypertensive condition that will put her pregnancy at risk.
Gestational Diabetes
Gestational diabetes, clinically known as gestational diabetes mellitus (GDM), occurs in pregnant women when their pancreatic function is unable to overcome the pregnancy-related insulin resistance and glucose levels in the blood reach certain levels.

A woman’s pregnancy is almost always accompanied by some degree of "insulin resistance" because of the placental secretion of certain hormones like estrogen, cortisol, and human placental lactogen (hPL). These hormones affect her cells’ ability to remove glucose from the blood stream and produce energy with it. When too much glucose is in the bloodstream during pregnancy, the mother may be diagnosed with GDM.
GDM increases the mother’s risk of preeclampsia and can cause abnormalities in fetal growth. This may include fetal macrosomia (a baby that’s large for gestational age), cephalopelvic disproportion, and other birth defects. The mother may experience a prolonged delivery due to the large baby.
Other potential complications of gestational diabetes for the baby include fetal hypoglycemia (low blood sugar), respiratory distress, and fetal distress.
According to the American Diabetes Association, nearly one in 10 pregnancies is affected by gestational diabetes. Timely diagnosis and management of this condition can help prevent potentially severe outcomes for the baby’s health.
Infections During Pregnancy
A woman’s immune system is naturally suppressed during pregnancy, increasing her risk of contracting an infection. Maternal infections can range in severity, but they all require a quick diagnosis and treatment plan to minimize the risk of infections passing to the baby or causing further complications.
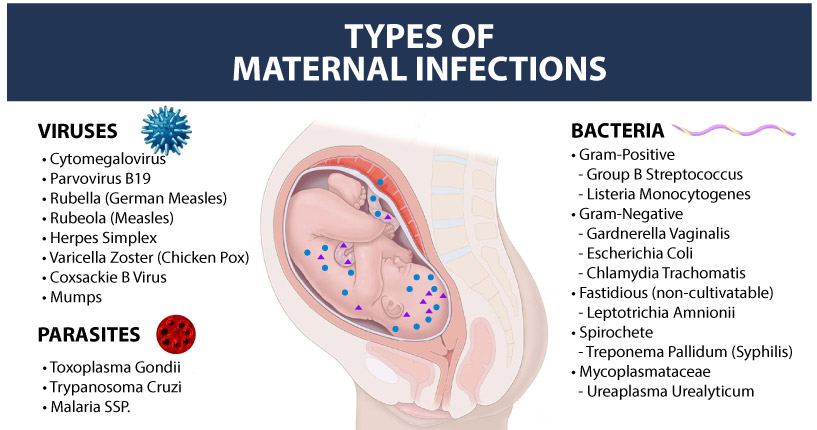
Listed below are some of the most common maternal infections that can complicate a mother’s pregnancy:
- Group B Strep: Group B strep (Group B Streptococcus or GBS) is a very common bacterial infection occurring in the genitourinary (genital and urinary) or gastrointestinal (digestive) tract. About one in four pregnant women will have GBS. Most of these women will have no symptoms at all.
The CDC recommends screening for all pregnant women for group B strep during the 35th to 37th week of pregnancy. This is the “standard of care” for obstetricians, MFM physicians and midwives caring for expectant mothers. GBS testing involves obtaining a swab of the vaginal and rectal areas, which is then sent to a laboratory for analysis.
As part of routine prenatal care, medical providers should identify patients that are more likely to benefit from administration of intrapartum (during the birthing process) antibiotics to treat GBS. - Bacterial Vaginosis: About 25% of all pregnant women contract bacterial vaginosis, making it one of the predominant maternal infections leading to adverse pregnancy outcomes. This infection is caused by a bacterium called Gardnerella vaginalis. Marked by vaginal irritation, a “fishy” odor, and abnormal vaginal discharge, BV may contribute to miscarriage, premature membrane rupture, or cerebral palsy due to other complications.
- Herpes Simplex Virus: Among all the sexually transmitted infections, herpes simplex virus is one of the most common to affect pregnant women. Mother to baby transmission of this infection can cause serious complications in the baby, including birth injuries and cerebral palsy. Medical providers can significantly reduce the risk of infection transmission to the baby with a timely diagnosis, proper management with medications and even a cesarean section delivery if necessary when the baby is showing signs of fetal distress.
- Chorioamnionitis: Chorioamnionitis is an acute bacterial infection of pregnancy that enters the mother’s uterus and invades the membrane and amniotic fluid surrounding the baby. The most common bacteria causing chorioamnionitis are Group B Strep and E.coli.
Chorioamnionitis typically occurs when the amniotic sac is broken for an extended period prior to birth. This is known as “premature rupture of membranes” or PROM. Another typical scenario where chorioamnionitis may develop is when the mother has a prolonged or arrested labor.
A delayed diagnosis or improper management of chorioamnionitis can lead to serious birth complications such as preterm birth, meningitis, neonatal sepsis, pneumonia, and cerebral palsy. - Urinary Tract Infections: Pregnant women often encounter urinary tract infections. One of the serious medical conditions that may occur because of inadequate treatment of UTI during pregnancy is pyelonephritis. This kidney infection is a major cause of preterm labor and may increase the risk of birth complications including cerebral palsy or hypoxic-ischemic encephalopathy. The medical team should be able to distinguish between normal and abnormal findings for UTI and kidney infections and treat the infection appropriately.
Bleeding During Pregnancy
A light amount of vaginal bleeding early in a woman's pregnancy is normal and often not a cause for concern. In fact, many women who experience spotting or bleeding during this time go on to have normal pregnancies and deliver healthy babies.

Bleeding later in pregnancy or heavier bleeding that requires a sanitary pad isn't normal and may indicate a potential complication. If you are bleeding at any stage in your pregnancy, you should call your doctor or midwife. They can help you determine why you are bleeding and offer guidance and support. When physicians and other healthcare providers fail to promptly recognize and address maternal bleeding, it can lead to severe birth complications such as placental abruption, placenta previa, preterm birth, and uterine rupture.
To successfully manage bleeding disorders in pregnant women, it is not only necessary for healthcare providers to understand the type of bleeding disorders that commonly occur in pregnancy, but they must also be knowledgeable about when and how bleeding occurs so they can properly treat the mother.
Post Term Pregnancy
Post term pregnancy, alternatively called prolonged pregnancy or post maturity, occurs when the pregnancy extends beyond the normal gestation of 37 to 42 weeks from the first day of the last menstrual period (LMP). An estimated 10 percent of all expectant mothers give birth post term.
Birth injury risks increase in a post term pregnancy because the baby may develop macrosomia (larger size than average), the placenta may begin to fail, or the mother may experience a premature rupture of membranes (PROM). PROM increases a baby’s risk for experiencing meconium aspiration syndrome (when the baby breathes a mixture of fecal material and amniotic fluid). These birth complications also put the baby at a risk of hypoxic-ischemic encephalopathy (HIE), which is a leading cause of cerebral palsy.
Medical negligence may be involved if your labor was not induced on time, the labor was prolonged or arrested, or if the medical provider miscalculated the due date or failed to corroborate it with an ultrasound test. Inaccurate pregnancy dating based on the last menstrual period (LMP) without corroborating it with an ultrasound exam is the most common cause of post term pregnancy.
Medical providers should carefully track the pregnancy and be prepared to induce labor around 40 weeks or even earlier (depending on the condition) rather than allowing the pregnancy to continue further. In some instances, this may require performing an emergency C-section delivery.
Blood Clots During Pregnancy
During pregnancy, a woman’s body produces higher levels of estrogen, which triggers an increased production of proteins like thrombin and fibrinogen. These proteins thicken the blood and increase the likelihood of blood clotting.

Additionally, a pregnant woman’s blood vessels will clot more easily as a natural bodily response intended to lessen blood loss during labor and delivery.
Expecting mothers are more likely to develop blood clots in the legs because of the increased pressure from the growing child on the pelvic blood vessels. This can restrict blood flow to the legs and increase the chance of clotting.
Healthcare professionals must be aware of these risks and carefully monitor expecting mothers so they can administer appropriate information and treatment to safeguard them from the dangers blood clots present.
Intrauterine Growth Restriction (IUGR)
Intrauterine growth restriction (IUGR) or "Fetal Growth Restriction" means the baby’s size is abnormally small, which can cause serious birth complications around the time of birth as well as long-term stunted growth.

IUGR is most commonly caused by placental insufficiency, a complication with the placenta that restricts it from delivering the proper amount of oxygen and vital nutrients to the fetus. Placental insufficiency can be caused by certain infections, past placental damage, or the mother’s underlying medical conditions like preeclampsia or gestational diabetes.
To detect IUGR and placental insufficiency, the medical provider should perform a thorough physical exam of the mother and review her detailed medical history during prenatal testing visits. Periodic Doppler ultrasound screenings can help in early diagnosis of the condition. MRI imaging will also provide valuable information to make a more conclusive diagnosis of placental insufficiency.
According to several research studies, babies with IUGR are five to seven times more likely to develop cerebral palsy. Reduced oxygen supply to the developing brain during pregnancy can put the baby at an increased risk of hypoxic-ischemic encephalopathy, leading to cerebral palsy and other neurodevelopmental disabilities. White matter injury patterns in the brain are also seen in some babies with IUGR, which can be an early indication of cerebral palsy.
Neonatologists, pediatricians, and NICU nurses must exercise caution in how they treat babies with IUGR to minimize their risk for birth injuries.
Placental Problems
An expecting mother’s placenta plays an enormous role in her baby’s well-being. The placenta is an organ that grows in the mother’s uterus during pregnancy and attaches itself to the uterine wall. The placenta is what provides the baby with all the oxygen and nutrients needed to thrive during pregnancy.

The baby’s umbilical cord is connected to the placenta and is the vessel through which these nutrients and oxygen travel to the baby. The placenta also carries the fetus’s waste products away.
Any complications with the placenta, including its size, strength, or location, can endanger both the mother and her baby and require close medical attention.
Placenta Previa
Placenta previa is a medical condition that may occur during pregnancy when the placenta fully or partially covers the cervix (the uterus opening). In normal conditions, the placenta is attached to the top of the inner uterine walls, but it attaches lower with placenta previa.
The condition can usually be diagnosed early during pregnancy with an ultrasound exam. Some patients with undiagnosed placenta previa may experience painless vaginal bleeding and visit the ER during the second or third trimester.

When an expecting mother has placenta previa, it may cause the blood vessels connecting the placental tissue to the uterus to tear at the time of labor or during delivery. This can cause severe bleeding which will result in fetal distress if not immediately addressed with an emergency c-section.
Routine ultrasound exams in the first and second trimester usually help medical providers detect placenta previa. It’s noteworthy that the earlier during the pregnancy placenta previa has been present, the greater are the chances that it will resolve on its own. About 9 out of 10 “low lying” placenta conditions will naturally resolve by the third trimester.
Nevertheless, obstetricians and maternal fetal medicine specialists should always order follow-up ultrasound exams at 28 to 32 weeks gestation to identify unresolved or persistent placenta previa.
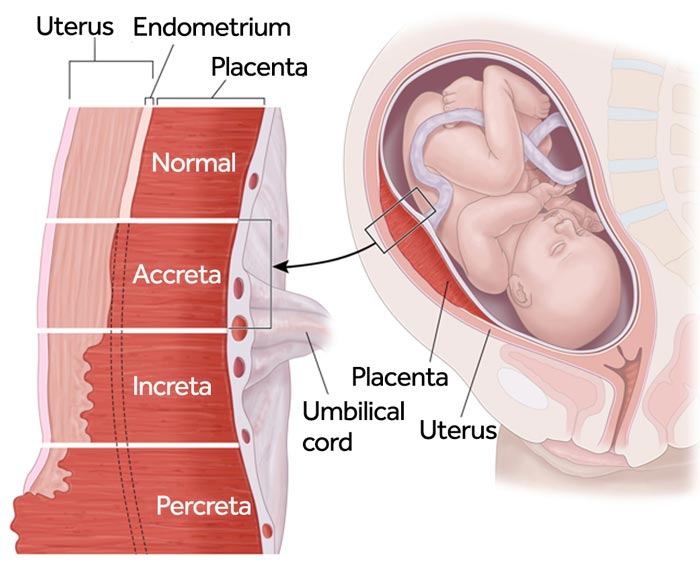
Placenta Accreta
Placenta accreta is a pregnancy complication where the mother’s placenta implants too deep into the uterine wall. While the placenta is supposed to attach to the wall of the uterus, it may not detach properly after birth if it is embedded too deep into it.
There are three types of placenta accreta that increase in severity:
More severe forms of placenta accreta (increta and percreta) are often accompanied by placenta previa, where the placenta covers the opening of the mother’s cervix. This can cause a placental abruption during labor and delivery and cause excessive bleeding for the mother. Doctors often opt to deliver the baby early to minimize these risks. In cases where placenta previa is suspected, they may require a planned C-section procedure.
Placenta accreta can normally be caught during prenatal testing with ultrasounds or magnetic resonance imaging (MRI) scans. An early diagnosis gives healthcare providers more time to plan for treatment options, but sometimes the condition can go unnoticed until the mother has given birth and hasn’t delivered her placenta within 30 minutes after.
Doctors, nurses, and other specialized medical professionals must be able to identify an expecting mother’s risk for placenta accreta and know how to treat it along with any related birth complications.
Polyhydramnios
Polyhydramnios is a pregnancy complication in which an excessive volume of amniotic fluid accumulates around the baby, increasing the risks of birth complications and birth injuries. Polyhydramnios can cause birth complications like premature birth, umbilical cord prolapse, premature rupture of membranes (PROM), and breech presentation.
Milder cases of polyhydramnios usually first occur during the third trimester, but the condition may sometimes develop in the second trimester – as early as 16 or 17 weeks of gestation. Severity of polyhydramnios is generally higher when it occurs early in the pregnancy.
An ultrasound exam can provide an accurate measurement of the volume of amniotic fluid. The volume may be measured as amniotic fluid index (AFI) or as maximum vertical pocket (MPV). MPV measures the single deepest vertical pocket of amniotic fluid in the uterus.
When severe polyhydramnios is diagnosed, the medical provider should consider a procedure called amnioreduction depending upon when in the pregnancy this occurs. This procedure may be performed using vacuum assisted devices, such as vacuum bottles or tubing, or even manually.
Oligohydramnios
The opposite of polyhydramnios, oligohydramnios occurs when the amniotic fluid volume (AFV) during pregnancy is lower than expected for the baby’s gestational age.

An abnormally low level of amniotic fluid may affect the baby’s health or could be an indicator of an underlying medical condition, which may create complications at the time of labor or delivery. Oligohydramnios affects about 4% of expectant mothers and is more commonly seen during the last trimester. In post term pregnancies, the incidence of oligohydramnios is as high as 12% because amniotic fluid volume significantly reduces after 40 weeks of pregnancy.
Oligohydramnios can increase the risk for restricted fetal growth, umbilical cord compression, underdeveloped lungs (which can lead to respiratory distress syndrome), fetal heart rate decelerations, or a neonatal infection if the mother’s water breaks early.
Obstetricians and labor-delivery nurses caring for a mother with known or suspected oligohydramnios must closely monitor the well-being of the baby including using an electronic fetal monitoring device. If warnings signs of fetal distress arise, the medical providers must be prepared to deliver the baby early by performing an emergency c-section.
Obesity Related Complications
Maternal obesity can increase an expecting mother’s risk of complications and birth defects for her child. Two of the most common complications associated with maternal obesity are preeclampsia and gestational diabetes. However, it can also affect fetal development in the following ways:
Cephalopelvic Disproportion (CPD)
Fetal Macrosomia

Fetal macrosomia is an obstetric condition that describes a newborn with a higher-than-normal birth weight. Macrosomia is associated with potentially life-threatening complications for the baby and increases the baby’s risk of birth injury and birth complications.
The American College of Obstetrics and Gynecology (ACOG) defines macrosomia as growth of the baby beyond a specified absolute birth weight of 4,000 grams (8 lb, 13 oz) to 4,500 grams (9 lb, 15 oz), irrespective of the baby’s gestational age. Importantly though, there is no universally accepted absolute birth weight figure that defines macrosomia.
There are serious birth complications that can occur if a baby with macrosomia is delivered vaginally. The baby may be too large to fit down the birth canal, causing prolonged or arrested labor that can cause fetal distress or complications right at birth including shoulder dystocia that increases the risk of needing to use of vacuum extractors and forceps.
Effective coordination and communication among the inter-professional team members, including obstetric providers, neonatologists, anesthesiologists, endocrinologists, pediatricians, mental health counselors, and registered dietitians is vital to the successful management of a macrosomic pregnancy.
Ectopic Pregnancy Misdiagnosis
An ectopic pregnancy occurs when a fertilized egg doesn’t attach to the uterus properly and instead implants outside of it. In a normal pregnancy, a mother’s egg is dropped from her ovary and travels through the fallopian tube to be fertilized by the father’s sperm.

But in an ectopic pregnancy, instead of the fertilized egg attaching into the uterus, the egg tries to attach to an external organ. 90% of ectopic pregnancies implant into the fallopian tube, but they can also occur in the cervix, the ovary, or even in the abdominal cavity.
A fetus is unable to develop properly outside of the uterus, meaning that an ectopic pregnancy has no chance of being viable. Medication is normally prescribed to treat it, although more severe ectopic pregnancies require surgery to treat.
An ectopic pregnancy is a life-threatening medical emergency that requires immediate treatment. When mismanaged or left untreated, it can rupture a woman’s internal organs and threaten her ability to ever become pregnant again. Doctors, nurses, and all other healthcare professionals must recognize the risks, signs, and symptoms of a mother’s ectopic pregnancy and act quickly to reduce her chances of becoming permanently injured.
A blighted ovum (also sometimes called an anembryonic pregnancy) is a pregnancy complication that occurs when a fertilized egg implants into the uterus but doesn’t grow into an embryo. Ovum means female reproductive egg cell, and the word blighted refers to the egg cell being in a state of deterioration or decay.
Blighted ova are one of the most common causes of miscarriage during the first trimester. When mismanaged or left untreated, the retained scar issue of a blighted ovum can cause bleeding or infection for the mother.

An expecting mother may not notice at first that she has a blighted ovum because the placenta still develops and releases hormones that will make her body mimic the signs and symptoms of a normal pregnancy. In addition, her pregnancy test will still read as positive.
Healthcare providers can normally spot a blighted ovum miscarriage through a transvaginal ultrasound, where they will observe an empty gestational sac that resembles a dark spot or bubble in the mother’s womb. They may also test her human chorionic gonadotropin (hCG) hormone levels as low traces by the 8th week can indicate a miscarriage.
Healthcare providers must be able to identify the signs of a blighted ovum as early as possible to prepare and assist the mother for the grief that comes with a miscarriage. In the event she cannot pass the excess tissue naturally, they must be prepared to remove it manually to reduce her risk of infection.
Premature Rupture of Membranes (PROM)
Premature rupture of membranes (PROM) is a medical condition that occurs after 37 weeks of gestation and before labor begins, when the amniotic sac holding the amniotic fluid and the baby ruptures. Commonly known as “water breaking,” rupture of membranes (ROM) usually prompts the onset of labor.
Premature rupturing of membranes can sometimes be caused from a maternal infection that weakens the membranes early. It can trigger a mother’s premature birth, can cause umbilical cord prolapse or compression, or can lead to contracting an infection from the amniotic fluid entering the bloodstream. An emergency cesarean section is usually advised in cases of PROM to avoid these risks.
When the mother suspects PROM and reports watery vaginal discharge or leaking, the medical provider should confirm it with a sterile speculum exam. A speculum is a device to look inside the vagina to observe the cervix. This minimally invasive diagnosis can help the healthcare provider identify the complication and move forward with treatment.
Doctors and nurses must be very aggressive in providing care and treatment to minimize the birth complications that can cause injury to a child following a preterm PROM.
Rh & ABO Incompatibility
Everyone has a blood type – either A, B, AB, or O. But each type is also split into different categories based on several factors, including whether Rh protein is present. “Rh” refers to the rhesus factor, an antigen found on the surface of some people’s red blood cells. A person’s blood type includes either “positive” or “negative” to indicate their Rh status.
About 85% of humans have Rh-positive blood. Generally, being Rh-negative is not a problem except for pregnant women and their babies.

Expecting mothers and their babies usually do not share blood, but small amounts of blood sometimes transfer from baby to mother. When this happens, the mother’s body views blood from a Rh-positive baby as a foreign substance. Her immune system kicks in and creates antibodies to combat that substance.
When this occurs, the mother’s antibodies can cross the placental barrier and enter the baby’s bloodstream. Because of the Rh incompatibility, the antibodies then begin to attack the baby’s red blood cells, damaging and sometimes destroying them. Diminished red blood cells can lead to oxygen deprivation in the baby, cause heart failure and may contribute to neonatal jaundice due to high bilirubin levels in the blood.
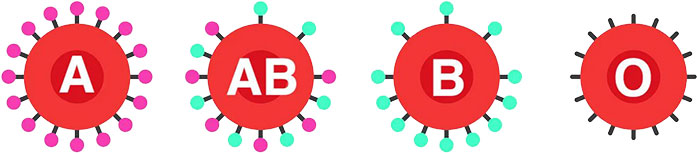
As with Rh incompatibility, problems can arise when the mother’s blood type contrasts with her baby’s. However, this condition only occurs when the mother is blood type O. For example, incompatibility occurs if the mother is type O and the baby is type A, B, or AB. If the baby is also type O, then the mother’s body should not produce antibodies if their blood intermingles.
The most common complication with ABO incompatibility is neonatal jaundice. Doctors can prepare for these risks by taking adequate blood samples during routine prenatal testing.
Incompetent Cervix
As a pregnant woman prepares to give birth, the cervix softens, shortens, and dilates, allowing the baby to travel through the birth canal towards delivery.
When pregnant women experience a condition called incompetent cervix, the cervix begins to shorten or dilate sooner than the 40-week gestational period. An incompetent cervix occurs in about 2% of pregnancies and puts the mother at risk of giving birth prematurely or miscarrying her child.
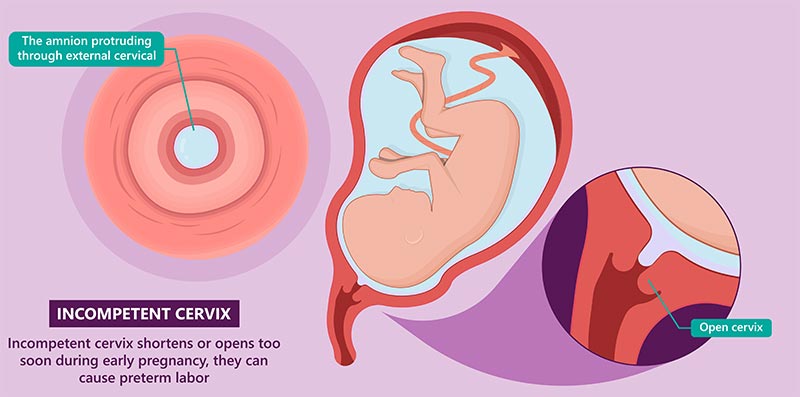
The most common cause of an incompetent cervix is when the cervix is too weak to withstand the baby's weight. The first reason why this occurs is because of structural abnormalities that make the cervix inherently weak. The second is that the cervix has suffered an injury or another sort of trauma in the past.
It is the responsibility of physicians and other healthcare providers to thoroughly review the history of a pregnant woman to identify any potential risk factors for an incompetent cervix. If a physician fails to intervene with appropriate medical treatment in time, it could potentially lead to tragic consequences.
To protect the fetus, a doctor may often recommend a medication induced labor or a cesarean section (C-section) to prevent further complications or a potential birth injury.
Hyperemesis Gravidarum
Hyperemesis Gravidarum is an extreme form of morning sickness that affects roughly 1 to 3 in every 100 expectant mothers. Morning sickness becomes hyperemesis gravidarum when nausea and vomiting intensify and continue past the first trimester.

Hyperemesis gravidarum symptoms often last longer than morning sickness and cause pregnant mothers to vomit several times per day. If a mother becomes dehydrated from vomiting several times a day, she may need treatment in a hospital with IV fluids.
Mothers who experience extreme weight loss because they are unable to keep food down may need nutritional treatment by nasogastric feeding to restore lost nutrients.
Healthcare providers don't know precisely what causes hyperemesis gravidarum; however, changing hormone levels in a pregnant woman’s body, namely human chorionic gonadotropin (hCG) and estrogen, likely play a role in the condition.
An early diagnosis of hyperemesis gravidarum can decrease the severity of symptoms and prevent adverse maternal and fetal outcomes.

If the mother’s healthcare provider suspects hyperemesis gravidarum based on symptoms, they must review her medical history and perform a physical exam to identify the symptoms and begin planning treatment options.
This may include hydration through IV fluids and tube feeding to relieve nausea and vomiting.
Cholestasis
Intrahepatic cholestasis of pregnancy or cholestasis is a liver disease that occurs when pregnancy hormones affect the flow of bile acids in the gallbladder. Bile is a substance in the liver that helps digestion; however, when it piles up in the liver, it can be released into the bloodstream and cause serious problems for a developing baby.

Although the typical development period of cholestasis is during the third trimester, it may sometimes start in early pregnancy. While cholestasis typically goes away within a few days after delivery, it can potentially lead to long-term complications for the child when improperly managed.
For instance, two of the primary birth injuries that ICP increases a baby's chances of developing are Hypoxic-Ischemic Encephalopathy (HIE) and Meconium Aspiration Syndrome (MAS).
In addition, women with cholestasis of pregnancy are at an increased risk for premature birth. While ICP is rare, it is the most common liver disease in pregnancy, affecting approximately one to two in 1,000 expectant mothers.
Severe itching, also known as Pruritus, is one of the main symptoms of ICP that primarily affects the hands and feet. Healthcare professionals must warn expectant mothers that itching or jaundice may be a sign of cholestasis.
Which Pregnancy Complications Carry the Highest Risk of Maternal Death?
A mother’s death during pregnancy or shortly thereafter can be painfully devastating for the people she leaves behind. And while the majority of pregnancy complications don’t pose a threat to the mother’s life, some conditions carry more risk than others.

The most common pregnancy complications with the highest risk of maternal mortality include:
- Excessive Bleeding: Excessive blood loss can be life-threatening when not treated with the required urgency. Many different complications can result in internal hemorrhaging, such as a tear in the placenta or the uterus. It is also a common complication of preterm birth or a C-section delivery.
- Infections: One of the primary concerns with a maternal infection is that the mother’s immune system will overreact to the infection and cause her to go into sepsis. Sepsis is a life-threatening condition where the infection-fighting chemicals in the body trigger an inflammatory response, damaging vital organs and sometimes resulting in death. A 2024 article from the National Institute of Health’s Medline Plus magazine cited infections and sepsis as the second-leading cause of maternal death in the United States.
- Preeclampsia: Preeclampsia and other hypertensive disorders can be deadly as they directly affect the mother’s vital organs like her brain, liver, and kidneys.
- Embolisms: When a piece of a blood clot (or thrombus) breaks off and travels through the bloodstream, that fragment is known as an embolus, and the blockage it causes is called an embolism. Embolisms in the lungs (pulmonary embolism) or the heart (coronary embolisms), while rare, are medical emergencies that often have small chances of survival.
Any pregnancy complication can become fatal when missed or improperly treated. If medical professionals make an error that violates the standard of care, and it results in a preventable death of the mother, it is considered medical malpractice.
Did Medical Malpractice Cause or Worsen My Pregnancy Complication?

Many common complications that arise during pregnancy are easily caught and treated with proper medical care during prenatal testing. Birth injury medical negligence, such as a misdiagnosis or failure to catch early symptoms of a problem, can lead to avoidable birth complications and cause injury to you or a birth injury for your child.
If a family believes medical negligence contributed to a pregnancy complication causing an injury, or even caused the untimely death or the mother or her child’s death, legal support may be an option. A specialized birth injury attorney can review the medical records and circumstances to assess whether a claim exists.
Parents whose children suffer from the long-term effects of their mother’s pregnancy complication, as well as mothers who were harmed during pregnancy, deserve to know whether it could have been prevented. Our dedicated birth injury lawyers want to help you find those answers and obtain the funds necessary to improve the quality of life for your child.
If your child has been diagnosed with a birth injury and you suspect this may have been caused in part by medical mistakes, Miller Weisbrod Olesky will thoroughly investigate the facts and hold the responsible medical providers accountable by pursuing medical malpractice claims against them.
Sometimes families are hesitant to reach out to a medical malpractice attorney or law firm. They may feel overwhelmed by their circumstances or are worried that a law firm will not be able to help them. But the only way to find out if you have a case is to talk to an attorney who understands how birth injuries can lead to developmental delays and other birth complications that require long-lasting medical support.
What is the Statute of Limitations in a Birth Injury Lawsuit?
A statute of limitations (SOL) is a law that sets a time limit on how long an injured person has to file a lawsuit after an accident. It is essential to understand that statutes of limitations vary based on the type of case and the state where it is filed. For instance, the deadline for birth injury claims is typically different from other claims, such as injury to personal property, fraud, contract disputes, and collection of debts.
Generally, the clock starts ticking on the date the injury occurred. However, there are exceptions to this rule, and in some cases, the statute of limitations starts when a person discovers or reasonably should have discovered an injury. When dealing with government agencies, SOLs can become even more complex.
For example, if the party that injured you was:
- A federal employee
- Employed by a military hospital, Veterans Administration facility, or a federally funded medical entity
You may need to file a birth injury claim under the Federal Tort Claims Act (FTCA). In FTCA cases, claimants must go through certain administrative procedures before filing a lawsuit. In some states, if the negligent party was a local or state government hospital or the doctors and medical providers are employees of a governmental entity, the time period in which you must give "notice" may be shorter.
If your case is filed outside of the statute of limitations, it will typically be dismissed, and you will not be eligible to recover compensation for your injuries. Determining when a statute of limitations begins on your case can be tricky. If you're considering pursuing compensation for a birth injury, contacting an attorney as soon as possible is in your best interest.
How The Birth Injury Attorneys at Miller Weisbrod Olesky Can Help

It takes a detailed expert review of the facts and circumstances of your pregnancy and the events happening before and after to determine whether any injuries sustained came as the result of medical malpractice.
Our Process
At Miller Weisbrod Olesky, a team of committed birth injury attorneys, nurses and paraprofessionals uses our detailed medical negligence case review process to assess your potential birth injury case. We start by learning more about you and your child and the status of meeting/missing developmental milestones. Then we gather medical records to determine what happened before, during, and after your delivery. We call in skilled medical experts who review your records and let us know if they think medical errors could have caused your child's injuries.
If we feel medical negligence caused or contributed to your child's death, we meet with you to discuss how you can receive compensation from the medical professionals who made the errors.
At no point in our legal intake process will we ask you to pay anything. The medical review of your case and the consultation are free. We only receive payment when you do. The sooner you reach out to us, the sooner we can begin investigating your case and gathering the evidence needed to support your claim.
We work on a contingency fee basis, meaning you won't pay any legal fees unless we win your case. Contact us today to schedule your free consultation by calling our toll-free line at 888-987-0005 or by filling out our online request form.
Contact Miller Weisbrod Olesky
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.