Neuroimaging
Neuroimaging During Pregnancy
Neuroimaging is a key tool in determining how and when a brain injury occurs in birth injury cases. There are many birth and neonatal injuries that can be diagnosed thanks to neuroimaging, such as hypoxic-ischemic encephalopathy (HIE), cerebral palsy (CP), and intracranial hemorrhages. Imaging is generally defined as the process of capturing detailed images of the structure and function of the central nervous system, including the brain, spine, and adjacent structures (such as cerebral spinal fluid).

Medical professionals can create images of the newborn's brain using various techniques, such as an MRI, CT, or ultrasound scan. When your baby is diagnosed with cerebral palsy or another neurological condition, neuroimaging is of the utmost importance for several reasons. Information from brain imaging can be used to determine the cause of any injury and provide necessary information that allows healthcare providers to develop appropriate treatment plans and interventions to optimize the child's long-term outcomes.
It can also help determine whether any injury occurred before or around the time of labor and delivery. If you have suspicions that your baby has suffered a birth injury caused by a medical professional's negligence, one of the questions you may have is whether the injury could have been prevented. At Miller Weisbrod Olesky, our birth injury attorneys have the knowledge and experience to help you determine if your child's birth injury was caused by a preventable medical mistake.
Birth Injury Malpractice Lawyers
(888) 987-0005The birth injury attorneys at Miller Weisbrod Olesky are dedicated to providing compassionate legal support to families and their children living with a brain injury or birth injury, such as cerebral palsy.
With the help of our in-house team of registered nurses and nurse-attorneys, we will assess whether the healthcare provider deviated from the expected standard of care by reviewing medical records, analyzing neuroimaging results, and consulting with medical experts. As soon as we've established that medical negligence was to blame for your child's injuries, we will fight tirelessly for the compensation you need to provide for your child’s long-term well-being and quality of life. Let us put our experience and results to work for your child.
Neuroanatomy- A Quick Overview
Our brains are the body's command center, controlling every thought, emotion, and the vast majority of our behaviors. Each part of the brain's intricate three-dimensional architecture works together to help us interpret the world around us by processing incoming sensory information and generating appropriate responses. The brain contains 100 billion neurons, which communicate with each other through an intricate network that carries messages to and from the brain to the rest of the body.
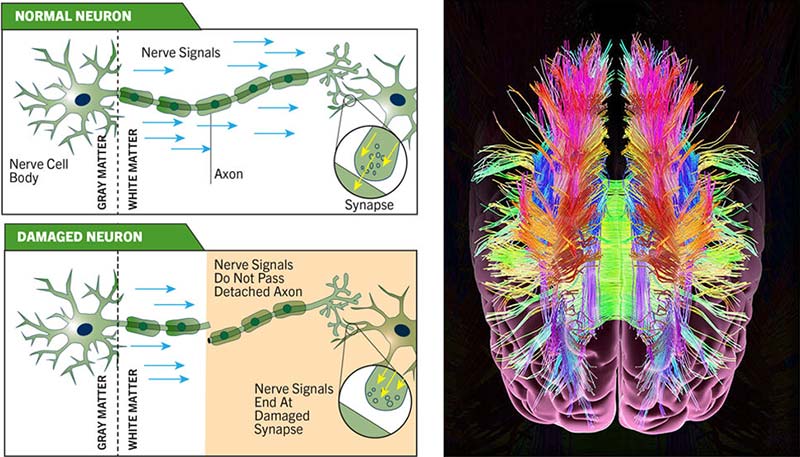
The outermost layer of the brain (the cerebral cortex) is composed of a complex network of tightly packed neurons that communicate over short distances via branching processes known as Dendrites and a separate process that is typically longer, known as the Axon. Electrical and chemical signals are transmitted between neurons by axons that travel in clusters called tracts to remote regions of the brain.
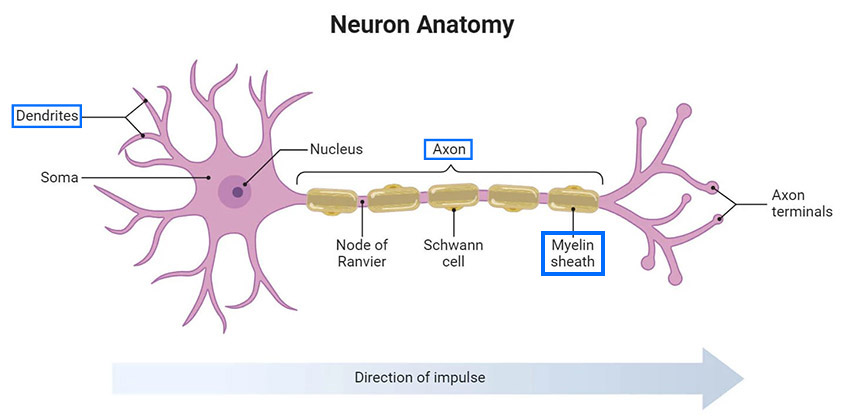
Myelin, a fatty substance that surrounds many axons, insulates traveling electrical signals and connects functionally specialized yet segregated areas of the brain. A direct injury from trauma can cause severe damage to this highly complex architecture of the human brain. An infant's skull is fragile and less rigid than an adult, making their developing brain more susceptible to brain damage.
A child can suffer lifelong physical and/or mental disabilities as a result of brain damage sustained before, during, or after delivery. A birth injury lawyer can help you determine whether you are eligible to file a claim for medical malpractice if your infant suffered brain damage due to a preventable birth injury.
What is Neuroimaging?
Neuroimaging is a remarkable class of technology that allows physicians to better understand the anatomy, chemistry, physiology, and electrical activity of the brain. Physicians can use neuroimaging to diagnose, monitor, and treat various neurological disorders, such as epilepsy, cerebral palsy, and hydrocephalus.
In summary, neuroimaging can help physicians:
- Study how the brain works
- Diagnose a disease
- Assess your brain health
- Better understand how various conditions or disorders impact the brain
There are two broad categories that neuroimaging falls into:
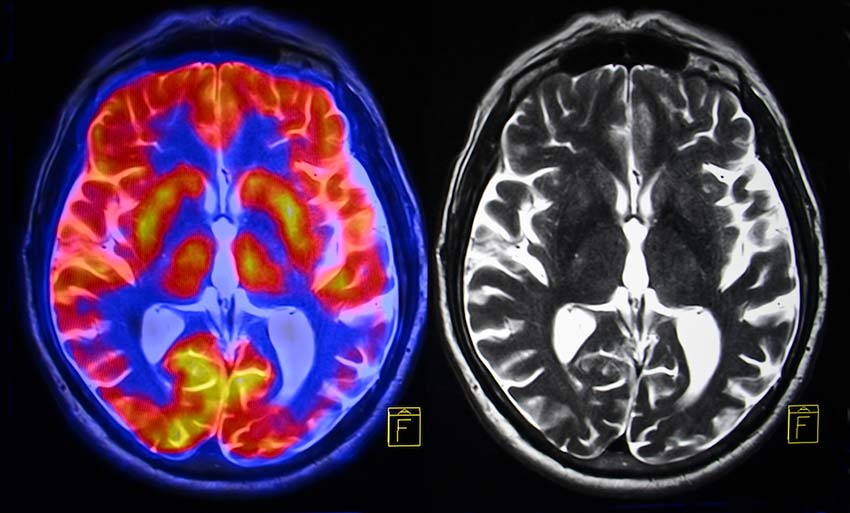
Structural imaging is often used to visualize the brain and diagnose large-scale injuries and intracranial diseases, including brain tumors.
Functional imaging involves measuring and mapping the brain's information-processing activity and function. This type of neuroimaging can be used for a more precise diagnosis of brain tissue injury and lesions (areas of injury or damage) to assist with cognitive psychology treatments. While current imaging techniques reveal both form and function, the newest tools can show how different regions of the brain connect and communicate.
What are the Different Types of Brain Imaging Techniques?
Throughout the years, experts have gradually improved brain imaging methods to map out different parts of the brain and see if it's structurally and functionally typical. After receiving the information from these scans, a doctor can form a diagnosis and create the most accurate treatment plan for their patient's specific needs.
While it may seem stressful to go in for brain imaging, one of the benefits is that it is a safe and painless procedure that doesn't require invasive steps. There are several different types of brain scans that are used to visualize the brain in a unique way. A physician will be able to assess which one to use for the issue they're trying to evaluate and treat.
The following are commonly used brain imaging techniques:
CT Scan
Computed Tomography, also known as a CT scan, uses a computerized X-ray machine to create detailed images of bones, soft tissue, blood vessels, and internal organs. A CT scan is likely be ordered to quickly evaluate whether a patient is bleeding into the brain after a brain injury or detect some other large abnormality.

CT uses a series of X-rays from multiple angles to create 2-D images of the brain and body and then combine them to develop cross-sectional slices or a 3-D map of the area of interest. This type of brain imaging technique can be used to find certain types of brain injuries, identify the extent and location of any brain swelling or bleeding, and reveal major structural brain changes.
Benefits of a CT Scan
- It is widely available in many hospitals
- It is a relatively quick procedure that is cheap compared to other options
- Three-dimensional pictures can be generated by stacking images
Limitations of a CT Scan
- It uses ionizing radiation
- It is often performed in a separate room that is far from the NICU
- It is not a suitable option for multiple scans in a row
- In terms of diagnosing HIE, it is less accurate than MRI
- It fails to examine tissue damage to the brain
Although Cranial CT has been used to assess for brain injury, MRIs are most commonly recommended for neonatal imaging because they provide a more precise image of the texture of the tissues in question. Unlike a CT scan, an MRI relies on the magnetic properties of water to provide images of the brain and does not use radiation. It is the best technique for providing useful information about the timing and nature of the injury.
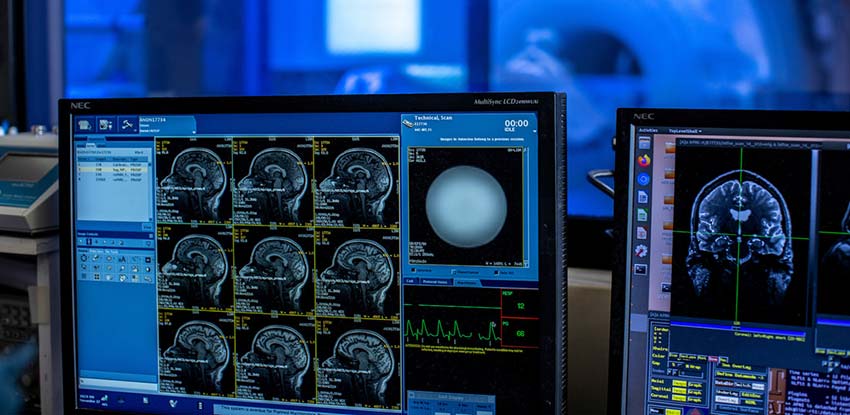
Magnetic Resonance Imaging (MRI)
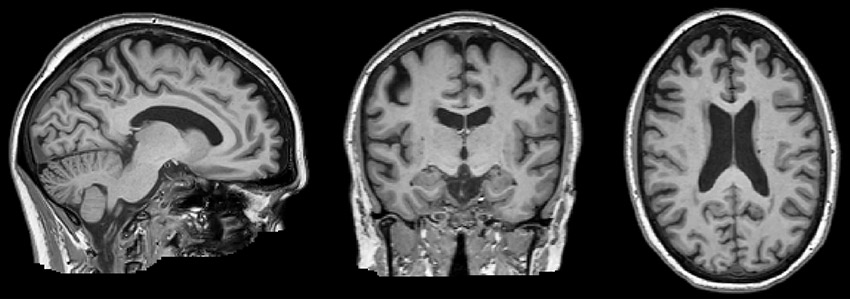
Magnetic Resonance Imaging (MRI) is the best technique for detecting and quantifying brain abnormalities. It is also helpful in diagnosing neonatal injuries such as cerebral palsy, hypoxic-ischemic encephalopathy, and hydrocephalus. This imaging method is a painless, non-invasive scanning technology that produces detailed 3-D anatomical images of the brain and body.

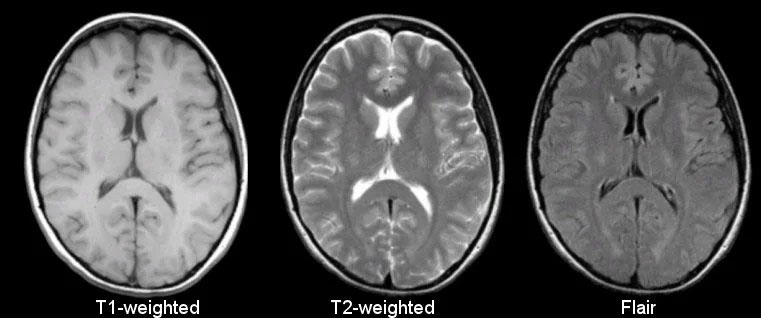
There are generally two types of MRIs:
- T1-weighted: Provides detailed images of the brain's anatomy and structure. In T-1 images, water appears darker and fat lighter.
- T2-weighted: More sensitive to changes in water content and better at detecting abnormalities like inflammation and tissue damage. In T-2 images, water appears lighter, and bone/tissue appears gray or black.
The basic MRI that you usually see in a hospital works by using a strong magnetic field that aligns the hydrogen protons of the body, which are then subjected to radio waves. When the radio waves are turned off, the scanner detects the energy released by the protons. It then sends this information to a computer that creates cross-sectional black-and-white images through complex mathematical calculations.
Although MRIs create a 3-D representation of the brain and body, MRIs are typically read and analyzed in 2-D slices, just like CTs. These images are used to diagnose and find the cause of specific brain injuries. MRIs can also provide rapid feedback about the effectiveness of treatments.
Benefits of an MRI
- No ionizing radiation is produced during the exam
- It is suitable for many scans in a row
- It creates very clear and detailed images
Limitations of an MRI
- The cost can be high
- While new MRIs can be used in the NICU, the exam often must be completed in a separate room
Although MRIs can be costly, improved diagnostic accuracy and patient safety often far outweigh the expense. MRI studies are essential for identifying the cause and severity of brain abnormalities in the neonatal period and have made a significant contribution to the decreased frequency of brain injuries in newborns.
One of the practical difficulties in obtaining an MRI for a newborn is that a typical MRI scan is very sensitive to motion, which is a major obstacle for pediatric MRIs. Additionally, because neonates' brains are made up of more water and have lower levels of proteins and lipids, MRI sequences used for adults must be adapted for newborns.
Electroencephalography (EEG)
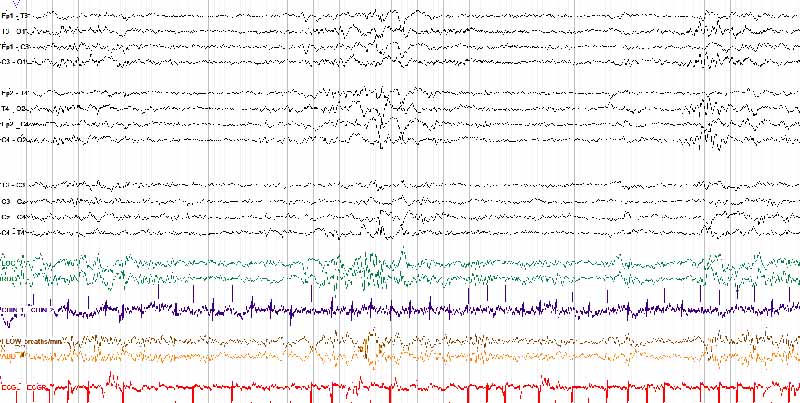
An EEG, or electroencephalography test, was the first non-invasive neuroimaging technique developed to measure brain activity levels and diagnose a number of conditions, including epilepsy (seizures) and traumatic brain injuries (TBIs). An EEG works by placing electrodes on the scalp with special glue and/or within a special cap that detects and records the electrical signals produced by the brain.

The electrodes placed on the scalp pick up the electrical signals generated by the activity of neurons in the brain and transmit the information to a computer that records the activity. These electrical brain waves look like random squiggly lines to the untrained eye but can be translated into five basic wave patterns, each associated with different cognitive functions.
The five basic wave patterns observed in electrical brain waves are:
- Gamma Waves are associated with higher cognitive functioning, such as problem-solving, memory retention, and processing sensory information. They are typically observed when a person actively engages in learning and has heightened perception.

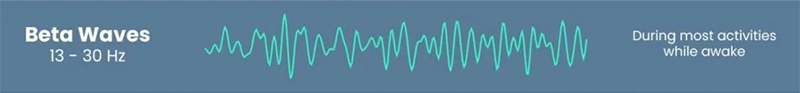
- Beta Waves are associated with an awake and alert state. They are typically observed when the brain is stimulated, and the person is engaged in conscious thought.
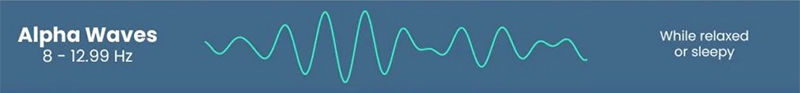
- Alpha Waves are associated with a relaxed but awake mental state. They are typically observed when a person is drowsy or daydreaming.
- Theta Waves are associated with deep meditation, intuition, and creativity. They are typically observed when a person is experiencing deep relaxation.

- Delta Waves are associated with very deep sleep. They are usually observed during states of unconsciousness.

Depending on the medical issues, healthcare providers may order different types of EEG tests to gather more specific information about a patient's brain activity and diagnose any potential neurological conditions.
EEG test types include:
- Routine EEG: A routine EEG scan can take as little as 30 minutes. During the test, a technician may ask you to breathe in and out deeply for a few minutes. They may also ask you to look at flashing lights to see how it affects your brain activity.
- Sleep EEG: A sleep EEG may be ordered if you have a sleep disorder resulting from an epileptic condition. This test is performed while you sleep, usually over several hours. In some cases, a sleep-deprived EEG test may also be recommended.
A sleep-deprived EEG is similar to a Sleep EEG test, but the patient is asked to stay awake the night before the test or get up earlier than usual to help ensure you can sleep while the test is being carried out. When a patient is deprived of sleep or is tired, the possibility of detecting abnormal brain wave activities is much higher.
- Ambulatory EEG: An ambulatory EEG test is prescribed when previous tests fail to capture unexplained seizure episodes that occur at random intervals. With this type of test, brain activity is recorded throughout the day and at night over a period of one or more days. This test involves wearing a small, portable EEG recorder connected to electrodes on the scalp.
The device measures the electrical activity of the brain as the patient goes about their daily activities while they're awake or asleep. During the test period, the patient is asked to keep a record of all their activities and may also require an assistant to monitor them in case a seizure occurs. With this test, a doctor can better understand what was occurring during a seizure episode. - Video Telemetry: A video telemetry test, also known as video EEG, combines the use of EEG electrodes and video recording equipment to continuously monitor and record a patient's brain activity. This integrated approach enables healthcare providers to detect seizures and other abnormal brain activities accurately.
By capturing both the electrical signals and visual symptoms, healthcare providers can better understand the relationship between the electrical activity in the brain and the physical manifestations of seizures. This enables them to make more accurate diagnoses and provide the most appropriate treatment options to manage the patient's condition effectively. - Invasive EEG: While Invasive EEG-telemetry tests are less common, they may be used in cases of more complex epilepsy to determine whether surgery is possible. This surgery involves placing electrodes in or on the surface of the brain to determine exactly where the seizures are coming from. Electrodes can be grouped in strips or grids or placed on thin wire probes. With an invasive EEG, the patient will stay hospitalized for a period of time to allow for continuous monitoring and recording of their brain activity.
A specialist can use an EEG to detect abnormalities in brain activity that can be indicative of a brain or mental disorder. Compared to older children and adults, the interpretation of the electrical brain waves in a newborn is more complex due to the immaturity of their developing brain. An EEG can help pediatric neurology clinicians identify seizures or understand the impact of brain injuries on the infant's brain.
The test is painless and generally very safe, with a low risk of possible complications. During the procedure, no amount of electrical current will enter the body and the patient will normally not experience any side effects apart from possibly feeling a bit tired.
Evoked Potential Tests
Evoked Potential Tests measure electrical activity in areas of the brain and spinal cord in response to stimulation of sight, sound, or touch. These non-invasive tests use electrodes and a stimulus to evaluate possible damage from a birth injury and can help diagnose neurological conditions in infants.
Electrodes placed on specific parts of the scalp and/or other parts of the body detect these signals and allow a healthcare provider to record and interpret the brain's electrical response to stimulus. Healthcare providers use evoked potential in combination with other tests to measure how quickly and completely nerve signals reach the brain and respond to stimulation. Through these tests, they can find abnormalities in the function of nerve and brain pathways that may result from neurological conditions. An EEG is especially useful in assessing hearing, diagnosing optic nerve disorders, and detecting problems affecting the infant's brain and spinal cord.
The three main types of evoked potential tests include those that measure response to visual, auditory, and electrical stimuli:
Brainstem Auditory Evoked Response (BAER)

This test measures the electrical signals the auditory pathway in the brain generates in response to sound and can be used to diagnose suspected neurologic abnormalities of the auditory nerve, auditory pathway, and brainstem. A BAER test uses small electrodes placed on the patient's scalp and earlobes. These electrodes provide information to a computer that records the brain's response to auditory stimuli, such as clicking noises and tones delivered to each ear. The test is one reliable way to identify issues with the nervous system and evaluate hearing losses in infants who suffered brain injuries during childbirth.
Visual evoked potential (VEP)
This test can help diagnose issues with the optic nerves and other visual pathways in the brain that affect sight by measuring the electrical signals the visual cortex generates in response to visual stimulation. A healthcare provider will attach electrodes to a patient's scalp and earlobes during a VEP test to record how their eyes respond when they look at a flashing checkerboard pattern on a screen. The test captures the patient's vision activity, and the doctor will review the results to determine how well they can see. The VEP test is safe and useful for patients of all ages, including infants.
Somatosensory evoked potential (SEP)
This test can detect damage within the spinal cord and brain by measuring the brain's response to mild electrical stimulation in various places on the body. During a SEP, a healthcare provider attaches electrodes to the scalp and other areas of the body that could be affected by numbness or paralysis. The electrodes are connected to a system that measures the electrical signals generated by the brain in response to mild electrical stimuli. By analyzing these signals, healthcare providers can identify any abnormalities or damage in the spinal cord and brain, helping to determine whether the child's senses have been impacted by a brain injury suffered at birth.
If you have concerns about the possibility of a developmental or structural issue that may require further investigation, you can consult your physician about the appropriate or suggested imaging procedure for your infant. Typically, follow-up imaging isn't done after a child leaves the NICU.
However, you have the right to insist on getting follow-up imaging done, as these tests can provide valuable information regarding your child's health and development. Before making a decision, it is important to discuss the benefits and risks of the various neuroimaging options available with your physician.
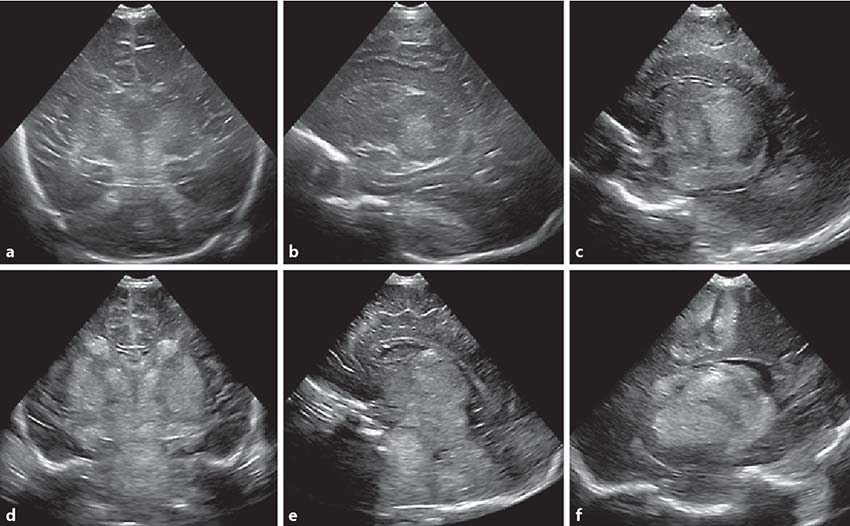
Ultrasound
A cranial ultrasound is a non-invasive medical test that uses reflected sound waves to make pictures of its inner fluid chambers (ventricles) and the cerebrospinal fluid that flows through these chambers. Sound waves and a small probe called a transducer produce a picture of the inside of the body. During an ultrasound, the technologist applies a small amount of gel to the area under examination and presses the transducer against the area under examination.

When pressed against the skin, the transducer transmits small pulses of high-frequency sound waves into the body. These high-frequency sound waves travel back and forth between the probe and the area being examined. The transducer records the echo waves (the sounds that bounce back). A computer then measures these waves and creates an image that is immediately visible on a video monitor.
The computer creates the image based on the amplitude, frequency, and time it takes for the ultrasound signal to return to the probe. Through these black-and-white images, your healthcare provider can view the internal structure of the brain, including the ventricles (fluid-filled cavities in the brain) and the blood flowing through the blood vessels. Radiologists are trained to analyze these images and will send a signed report to a doctor, who will then share the results with their patients.
The two main types of cranial ultrasound are:
- Head ultrasound: This test is most commonly done on newborns whose skull bones have not completely grown together. Head ultrasounds are typically done only on young babies because bones block the passage of ultrasound waves, and the fontanelles (soft spots on the infant’s head) provides an opening for the sound waves to reach the brain. The technologist places the ultrasound probe and some gel on the "soft spots" of the baby's head. A head ultrasound examines the structures of the brain, including the cerebrospinal fluid that surrounds and fills its ventricles.
- Transcranial Doppler: A Doppler ultrasound is a special ultrasound technique that measures both the direction and speed of the blood flow as it moves through the major cerebral arteries of the brain. The Doppler effect refers to a change in the pitch of the reflected sound waves caused by the movement of blood cells. The sounds are collected and processed by a computer that creates graphs or color pictures depicting blood flow through the blood vessels. A transcranial Doppler can be used alone or in conjunction with Magnetic Resonance Imaging (MRI), Magnetic Resonance Angiography (MRA), or Computed Tomography (CT).
Cranial ultrasounds are usually done:
- As part of routine tests for all premature neonates
- To look for bleeding within the brain tissue or the ventricles (intraventricular hemorrhage)
- To identify damage to the white matter brain tissue surrounding the edges of the ventricles (periventricular leukomalacia (PVL)
- To check a baby's increasing head size or a bulging fontanel
- To test for abnormal growths like a tumor or locate the site of an infection in or around the brain, such as from encephalitis or meningitis
- To detect a hypoxic-ischemic event in neonates
- To screen for brain problems that may be present from birth, such as congenital hydrocephalus
Ultrasound imaging is extremely safe because it does not use ionizing radiation, and there is no need for needles, injections, or sedation. There may be some discomfort during this exam, but it shouldn't be painful.
Some additional benefits of an ultrasound exam include:
- It is widely available
- It is portable and easily used in the NICU
- It is less expensive than most other imaging techniques
- It does not require special preparation
- It can be quickly performed
- Imaging can be repeated as many times as necessary
- It provides a clearer view of soft tissue that do not show up as well on X-rays
However, ultrasound imaging does have its limitations. For instance, because ultrasounds are sensitive to motion, moving or crying children can slow down the examinations. Additionally, because greater amounts of tissue weaken the sound waves as they pass deeper into the body, this test may not be recommended for larger patients who may be more difficult to image with ultrasound.
Some additional limitations of an ultrasound exam include:
- An open wound, recent surgical incision near the area being imaged, or changes in blood flow pattern as a result of irregular heart rhythms may alter the exam results
- Compared to other available technologies, ultrasounds tend to produce a less clear and complete picture
- Identifying the exact location of certain injuries can be difficult
- It is imperative that the ultrasound administrator and interpreter possess absolute expertise in this field
- Some biological effects can be produced in the body under certain conditions and settings
- The use of ultrasound should be restricted to medically necessary situations, particularly on neonates
- When detecting brain injuries, ultrasounds are not as sensitive or accurate as CT scans or MRIs
Further diagnostic tests, such as magnetic resonance imaging (MRI), are recommended for infants with abnormal cranial ultrasonography findings. Additional testing is useful in providing more detailed information about brain structures and identifying any potential underlying conditions. Consult your child's doctor if you have concerns about the cranial ultrasonography results or if you want to explore additional diagnostic options.
Common Neonatal Conditions Diagnosed with Neuroimaging
Neuroimaging in neonatal care is critical for diagnosing and understanding various conditions and disorders that may affect the developing brain. Doctors can use this diagnostic tool to identify and recommend appropriate treatment interventions for these vulnerable newborns. Early diagnosis of these conditions through neuroimaging can significantly improve the effectiveness of treatments and long-term outcomes for infants, reducing the risk of developmental delays and disabilities in the future.
Some of the most common disorders and conditions that neuroimaging can detect and treat include:
- Hypoxic-Ischemic Encephalopathy (HIE)
- Cerebral Palsy (CP)
- Periventricular leukomalacia (PVL)
- Caput Succedaneum
- Cephalopelvic Disproportion (CPD)
- Hydrocephalus
- Neonatal Stroke
- Cephalohematoma
Brain imaging of a newborn baby is the first and most important step in proving how your baby was injured. These techniques can demonstrate quite clearly that the injury suffered by the newborn occurred at or around the time of birth. A birth injury lawyer can establish a causal link between a medical professional's negligence and your child's birth injury by comparing the neuroimaging results with medical records and expert testimony from medical specialists.
This evidence can then be used to support a legal claim for medical malpractice and help families seek compensation for their child’s medical expenses, ongoing care and therapy, pain and suffering, and lost future earnings. If you suspect that your newborn has suffered a birth injury due to a preventable medical mistake, it is crucial to contact a birth injury attorney as soon as possible.
Birth Injuries and the Importance of Requesting Brain Imaging
Birth injuries can occur if a doctor fails to provide appropriate medical care or promptly address complications that arise during childbirth. Some examples of medical negligence that can cause a baby to experience a birth injury include improper use of forceps or vacuum extractors, delays in performing an emergency cesarean section (C-section), and administration of incorrect labor-inducing medications during labor and delivery.
In many cases, medical errors result in damage to an infant's brain that is not easy to identify without testing. Neuroimaging can provide evidence of structural abnormalities, such as intracranial hemorrhages or hypoxic-ischemic injuries. Doctors can use this imaging to diagnose the affected area of the brain and make informed decisions regarding treatment.
Furthermore, brain imaging scans like MRIs and EEGs can contribute to persuasive advocacy in a lawsuit by proving that negligence occurred during pregnancy or delivery and was to blame for your child's birth injury. Each of the mentioned neonatal imaging techniques allows observations to be made about the brain and helps physicians diagnose how the fetal or newborn brain was injured.
In addition to identifying well-recognized patterns of injury, imaging can also help establish whether the injury occurred before, during, or around the time of labor. Having your baby tested through various methods will strengthen your medical malpractice case by demonstrating that your child did, in fact, sustain a birth injury. If you are able to prove that a brain injury has occurred and that it was caused by the alleged negligence, financial compensation may be obtainable through a lawsuit.
Establishing that medical negligence caused a brain injury is a complex medical and legal issue. Having an experienced birth injury attorney on your side who can use this imaging may give you an advantage in filing a medical malpractice claim. Our birth injury attorneys at Miller Weisbrod Olesky understand the importance of gathering the necessary evidence to prove the damage your child and family have suffered. We have extensive experience assessing and litigating complex medical malpractice cases and encourage you to contact us as soon as possible to discuss the specifics of your potential claim.
Filing a Birth Injury Lawsuit
Parents may file a birth injury lawsuit on behalf of their child against negligent medical professionals responsible for causing their child to sustain a preventable birth injury. Families may seek compensation to cover the cost of their child's medical care and treatment costs through a Birth Injury lawsuit. It is important to note that while every case is different, most lawsuits typically follow a similar process. If your child was injured by a doctor, nurse, or other healthcare provider, an experienced birth injury lawyer can file your case, gather evidence, and pursue full and fair compensation on your behalf.
Free Case Review
Our experienced birth injury lawyers will determine if you are eligible to file a birth injury lawsuit during your complimentary case review, which you can schedule by contacting us via our toll-free line at (888) 987-0005 or by filling out our convenient online form on this page. If we can determine that medical malpractice may have played a role in your child's birth injury, your case will likely be accepted by our team.
Gather Evidence
A birth injury malpractice attorney will gather information and evidence related to your case as soon as they determine you qualify to pursue a lawsuit. Evidence like medical records, witness statements, and the employment history of the medical professional in your case are crucial to proving that your child's birth injury was caused by medical negligence.
File the Lawsuit
After gathering the necessary information, your attorney will file your lawsuit in the appropriate court. As soon as the case is filed, you and your family will become the plaintiffs (the party taking legal action). The healthcare professionals who may be responsible for causing your child's injury will become the defendants (the party being sued). The statute of limitations in each state governs the deadline for filing a birth injury lawsuit.
Your lawyer will ensure your case is filed on time according to your state's statute of limitations. The lawsuit outlines the charges against the defendants and gives them around 30 days to respond. If the defendants fail to respond, judgment will automatically be entered in the plaintiff's favor. In the event the defendants respond but fail to assume responsibility, they will explain why they believe they are not to blame for your child's injury.
Discovery
Your attorney will gather more evidence, such as medical records, medical expense reports, and other documents related to your case, once the defendants file their response. During this time, you, your loved ones, and medical experts may be required to give statements under oath. The parties will also exchange information and evidence relevant to their respective cases in an effort to build strong arguments. To prove that medical professionals failed to uphold a high standard of care, an experienced attorney will collect all legally required evidence.
Settlement Negotiations
Settlement negotiations can begin once both parties have prepared their cases. During this phase, both parties will try to reach an agreement (settlement) that allows them to resolve their dispute without going through a full trial. Should a settlement be reached, the defendants will pay you a lump sum, and all legal action will stop. If the case cannot be resolved during this stage, our lawyers have the experience and knowledge to represent your best interests in court.
Go Through a Trial
Cases that do not settle through settlement negotiations will go to trial. A jury and judge will examine all the evidence presented by both legal teams during the trial. A verdict is reached after each party has presented their case and a judgment has been entered. The losing party may decide to appeal the decision in some cases. The disadvantage of trials is that, while you might receive more compensation than you would receive from a settlement if you lose, you risk receiving no compensation at all. Our birth injury lawyers can help you obtain the compensation you need to cover the cost of your child's care and other injury-related expenses.
Medical Malpractice in Birth Injury Cases

When doctors, nurses, or other healthcare professionals commit medical negligence before, during, or after delivery, it can result in injuries to a mother, her child, or both. Even though not every birth injury is caused by medical malpractice, an experienced birth injury attorney can help make sure your child is compensated fairly if their provider was negligent in their care.
There are several examples of acts of medical negligence that can cause birth injuries during childbirth:
- Failure to recognize and treat signs of maternal or fetal distress, such as lack of oxygen
- Improper use of forceps or a vacuum extractor
- Using too much force during delivery
- Failure to schedule an emergency cesarean section (C-section)
- Delaying in performing an emergency C-section
- Failure to properly monitor the mother during her pregnancy
- Failure to administer the proper antibiotics or dosage to a mother with an STD or other maternal infections before delivery
- Ignoring or misreading a fetal monitoring strip
- Failure to detect and treat an umbilical cord complication
- Failure to diagnose and treat preterm labor in a timely manner
- Failure to treat maternal elevated blood pressure (preeclampsia)
- Failure to properly resuscitate a newborn after delivery
- Failure to treat jaundice and kernicterus
- Failure to respond to signs of a placental abruption
- Failure to detect a severe birth defect on a prenatal ultrasound
- Failure to carefully manage an abnormal fetal position
- Administering too high a dose of labor-inducing drugs like Pitocin
Failing to address birth complications such as a preterm delivery or umbilical cord issues can result in a serious birth injury. As leaders in our communities, we rely on medical professionals to provide high-quality health care.Generally, when people think of medical malpractice liability, they picture doctors and nurses. However, other parties involved in the care of a pregnant woman and her baby may also be held responsible in a birth injury lawsuit.
Medical negligence may be committed by one or more of the following types of medical providers or facilities:

- Obstetricians (OB-GYN)
- Other obstetric professionals
- Pediatricians, including pediatric neurologists
- Anesthesiologists
- Labor and delivery nurses
- Midwives
- Nurses
- Hospitals and medical facilities
- Hospital administrators
- Other hospital staff
- Neonatal nurses and aids
- Neonatologists or pediatricians providing neonatal care
- Respiratory therapists
- Maternal-fetal medicine physicians and specialists (MFM)
- Laboratory staff
Although medical malpractice suits are often filed against healthcare providers like doctors and nurses, hospitals can also be held liable in certain circumstances. A hospital can be vicariously liable for an employee's negligent actions that caused harm during work hours or while the employee was performing a job-related task. For example, if an OBGYN makes a negligent mistake during pregnancy or delivery, the hospital can be held vicariously liable.
A hospital may also be held directly liable for its own actions. For instance, if a hospital fails to adhere to medical protocols and standards, they may be directly liable for a patient's injuries. We can help you determine whether your child's birth injury was caused by a doctor, the hospital itself, or another medical professional.
When you file a birth injury claim, your lawyer must be prepared to present evidence that proves that a doctor's or hospital's negligence caused your child's birth injury. An injured plaintiff must be able to prove each of the following four legal elements in their birth injury lawsuit.
- Duty of care: Before the provider will have a duty of care, the plaintiff must be able to establish a provider-patient relationship. Upon establishing this relationship, the medical provider is expected to meet a relevant standard of care that a medical professional with the same specialization would have exercised under the same conditions.
- Breach: The next element the plaintiff must prove is that the healthcare provider or facility breached that duty by failing to meet the applicable standard of care.
- Causation: The plaintiff must then demonstrate that the healthcare provider's negligent care directly caused their or their child's injuries.
- Damages: Finally, the plaintiff must show that the harm they or their child suffered resulted in specific expenses and other losses. These losses may include anything from the cost of lifelong medical care to emotional suffering.
The plaintiff's attorney must present compelling evidence to establish liability and recover damages in birth injury cases. At Miller Weisbrod Olesky, our birth injury lawyers can collect evidence on your behalf, consult with medical experts to determine the cause of the injury, and identify all medical professionals who contributed to you or your child's birth injury.
What Legal Damages are Available in Birth Injury Cases?
When a doctor or hospital's negligence, wrongful action, or lack of action before, during, or after childbirth results in injuries to you or your child, you may be entitled to seek financial compensation. Damages in birth injury lawsuits generally fall into two categories: economic and non-economic. Economic damages are the financial losses you have sustained as a result of the injuries you or your child suffered. Non-economic damages refer to subjective, monetary losses and are meant to compensate the victim for pain and suffering experienced because of the birth injury.

Economic Damages
- Medical expenses (including the cost of any future medical care)
- The cost of any medications or surgeries
- Rehabilitation and therapy costs (occupational, physical, and speech)
- Lost income or wages of parents (including future loss of income)
- The cost of assistive equipment and devices like wheelchairs or communication aids
- Lost future earning capacity (if the child's birth injury impacts the child's ability to work in the future)
- The cost of special education services and tutors
- Home modification costs (such as ramps or accessible bathrooms)
- Costs associated with a caregiver or home nurse
Non-economic Damages
- Physical pain and suffering
- Reduced quality of life
- Disfigurement and permanent scarring
- Emotional or mental anguish
- Paralysis, scarring, and disfigurement
- Post-traumatic stress disorder (PTSD)
- Loss of consortium
Punitive or exemplary damages may be awarded in addition to economic and non-economic damages. Damages for this type of behavior are often hard to prove and are usually awarded when the medical professional's behavior is especially negligent or careless. These damages are intended to punish the at-fault party and deter others from committing similar wrongful acts.
The settlement award you may receive will depend on various factors, including the nature and severity of your child's condition, the impact of the injury on the child's quality of life, and the financial damages you have suffered. A birth injury lawyer can assist you in proving all your damages and calculating the value of your medical malpractice settlement.
Statute of Limitations Birth Injury Cases
A statute of limitations is a law that imposes a deadline for filing birth injury lawsuits. If you fail to file a claim before the statute of limitations "runs out," you may lose your right to pursue legal action and seek compensation. In some cases where an injury may not be immediately apparent, the statute of limitations may be extended.
The discovery rule prevents the statute of limitations from running until the injury is discovered or reasonably should have been discovered. It is also important to remember that the statute of limitations varies by state and the type of claim you're filing. A birth injury attorney can help you avoid missing all crucial deadlines related to your case.
Get the Legal Support and Guidance Needed Our Cerebral Palsy Lawyers

While no amount of money can ever fully compensate for your child's suffering, an experienced cerebral palsy lawyer can help ease the financial burden of caring for your child and make it easier for you to afford the best medical care, treatment, and educational opportunities. At Miller Weisbrod Olesky, our birth injury lawyers are dedicated to helping you hold negligent doctors, hospitals, or other healthcare professionals accountable for your child's birth injuries.
Having achieved successful verdicts and settlements for medical malpractice clients in over 20 states, you can be confident that we will fight for the best possible outcome for you and your family. Our firm works on a contingency fee basis, meaning you will only pay fees if we win your case. We invite you to contact us at 888-987-0005 or fill out our convenient online form to schedule your free consultation with one of our attorneys.
Free Birth Injury Lawsuit Consultation
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.