Placental Abruption
Placental Abruption During Labor
An expecting mother’s placenta plays an enormous role in her baby’s well-being. The placenta is an organ that grows inside the mother’s uterus during pregnancy and attaches itself to the uterine wall. It contains all the blood, oxygen, and nutrients the baby needs to grow and thrive before birth.
These vital nutrients flow from the placenta to the baby through the umbilical cord. The placenta also carries away the fetus’s waste products.
Placental complications like a placental abruption threaten this critical exchange of gas, waste, and nutrients. When the placenta breaks off and prematurely detaches from the uterine wall, it endangers both mother and her baby.
Placental abruptions can cause postpartum hemorrhaging, shock, and organ failure for the mother. It can also reduce fetal blood flow and deprive the baby of oxygen. Prolonged periods of perinatal asphyxia can cause fetal hypoxia and lead to dangerous brain injuries like hypoxic ischemic encephalopathy (HIE).
HIE is a form of brain damage at birth resulting from a lack of oxygenated blood flow to the baby during labor. It can cause neonatal seizures, vision impairments, developmental delays, and a range of physical and intellectual disabilities. HIE is also the leading cause of cerebral palsy.
It’s critical that medical providers understand the causes of placental abruption so they can identify mothers who are at risk. They must know the signs and understand how to respond to this medical emergency. Failing to act in a timely manner can increase the risk for birth injuries and sometimes count as medical malpractice.
Birth Injury Malpractice Attorneys
Our top rated birth injury lawyers help families seek justice and compensation for preventable injuries to mothers or their babies during childbirth. If you or your baby suffered preventable harm from mismanaged labor and delivery complications, don’t hesitate to contact our firm. We can answer difficult legal and medical questions and investigate the facts on your behalf.
Free Legal Consultation
Birth Injury Lawyers
(888) 987-0005Our Birth Injury Lawyers are available to meet you in your home or the hospital.
Our vast network of medical experts and in-house nursing staff and nurse-attorneys gives us the edge over our competition. When we take your case, we assign you with not just an attorney but an entire medical team. This team includes attorneys, experienced nursing advocates, and seasoned medical experts.
Your team is available to assist with any day-to-day treatment you or your child may need. This includes assistance with obtaining medical records, scheduling doctors’ appointments, providing transportation, and any other problems that may arise.
We offer all of this on a contingency fee basis. This means you will not pay any fees until after we win your case and secure a settlement. Our firm’s unmatched track record of birth injury results sets us apart from other birth injury law firms.

Recent Birth Injury Settlement:
Birth Injury settlement against a hospital in which nurses and physicians failed to properly monitor the mother's blood pressure during delivery causing an HIE event resulting in neonatal seizures and cerebral palsy at birth. Our team of top-rated birth injury lawyers recovered $13,750,000 for the family to help with future medical expenses and developmental therapy.
What Is Placental Abruption?
As a temporary organ, the placenta normally detaches from the uterus after the baby delivers. The body naturally expels it since the baby no longer needs the oxygen and nutrients the placenta provided in utero. In fact, doctors commonly refer to a mother delivering her placenta as “the third stage of labor”.
Placental abruption occurs when the placenta prematurely separates from the uterus before delivery.

Since the uterus is a muscle, it is more “elastic” than the placenta. The uterus sometimes stretches or moves in response to trauma or during prolonged and excessively forceful contractions from uterine hyperstimulation. The placenta lacks the same stretchy, elastic tissue structure and therefore does not move along with the uterus.
Uterine movement that’s too intense can strain the vascular structures between the uterus and placenta. The blood vessels may rupture and tear away from the uterine lining, jeopardizing the placenta’s essential functions.
A detached placenta is weaker at delivering blood and oxygen. A baby receiving less oxygen may show signs of fetal distress as their heart beats faster to compensate.
Prolonged periods without sufficient oxygen put the baby at risk for fetal hypoxia or anoxia, which can have dangerous consequences. Oxygen deprivation during labor is the leading cause of brain injuries like hypoxic ischemic encephalopathy (HIE). HIE is permanent brain damage at birth that can cause cerebral palsy symptoms in young children.
While placental abruptions don’t always result in neonatal brain damage, doctors must be aware of the high risk they pose. Healthcare professionals must always treat an abruption as a medical emergency and react to it with the necessary urgency.
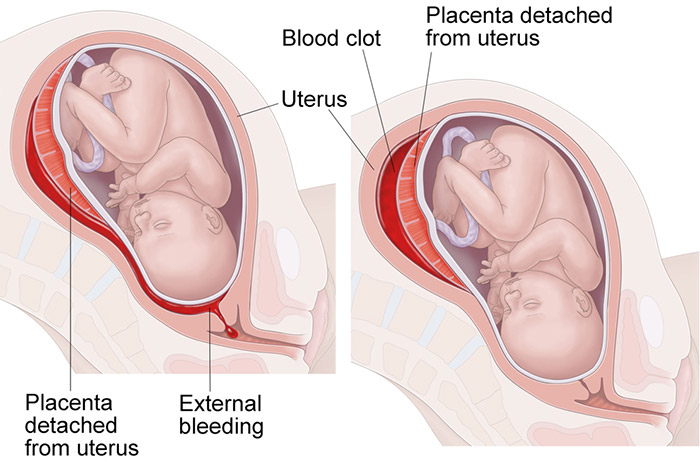
Are There Different Types of Placental Abruption?
A mother’s placental abruption can range in severity, depending on the extent of separation between the placenta and the uterus. Doctors may refer to the mother’s placental abruption as a:
- Partial Placental Abruption: The placenta has not completely detached from the wall of the uterus
- Complete or Total Placental Abruption: The placenta has completely detached from the uterine wall
- Revealed Placental Abruption: The mother has moderate to severe vaginal bleeding
- Concealed Placental Abruption: The mother has little to no visible vaginal bleeding. Typically, this is because the blood remains trapped between the uterus and placenta
Additionally, doctors and other medical providers may classify the severity of a mother’s placental abruption. The four classes of severity include:
- Class 0 - Asymptomatic: The abruption may not be evident until after the mother delivers the placenta
- Class 1 - Mild: The mother may exhibit little to no vaginal bleeding with very slight uterine tenderness. However, her vital signs remain normal and the electronic fetal heart rate monitor shows no signs of fetal distress
- Class 2 - Moderate: The mother may have moderate vaginal bleeding with significant uterine tenderness. Her heart rate and blood pressure may change, and signs of fetal distress from oxygen deprivation may appear
- Class 3 - Severe: Vaginal bleeding is heavy, causing the mother to go into shock. Her uterus may be rigid. There is a high risk of fetal demise unless an emergency delivery occurs in time

The mother’s and baby’s lives depend on the quick response from their doctors, nurses, and other attending medical professionals. Regardless of the classification, medical professionals should always treat a mother’s placental abruption as a medical emergency. Delayed responses only put her and her baby at an elevated risk for birth injuries.
What Is the Most Common Cause of Placental Abruption?
The most common cause of placental abruption is maternal hypertension, or high blood pressure during pregnancy.
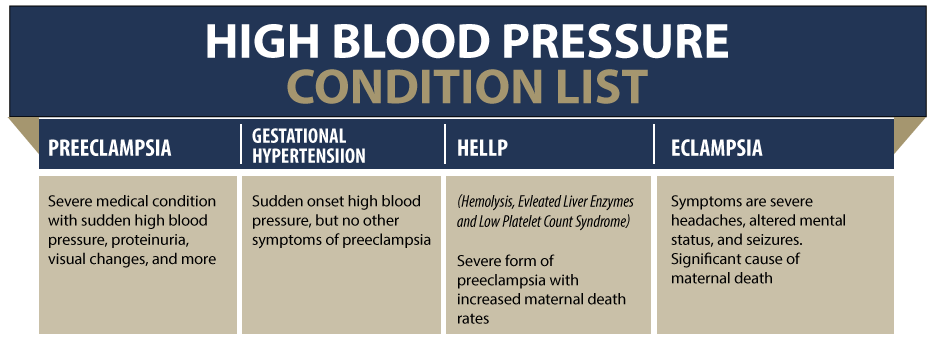
Blood pressure refers to the force of the blood pumping through the artery walls. An expecting mother’s blood pressure is normal at 120/80 millimeters of mercury (mm Hg). Blood pressure at or exceeding 140/90 mm Hg is high and qualifies as gestational hypertension.
Pregnancy complications like preeclampsia or HELLP syndrome can elevate a mother’s blood pressure to unsafe levels. Prolonged hypertension can damage the delicate uterine and placental blood vessels, resulting in a premature abruption.
The medical consensus is that maternal hypertension significantly increases the risk for placental abruption. Some studies identify mothers with chronic hypertension at a three-times-higher risk for abruption compared to pregnancies with normal blood pressure.
What Are Risk Factors for Placental Abruptions?

Beyond hypertension, a number of other factors and pregnancy complications can increase a mother’s risk for placental abruption. Such risks fall into one of four groups:
Medical History

Information from a mother’s medical history can signal she’s at risk for placental abruption. Some studies suggest that placental abruption is ten times more likely when the mother has already experienced a previous abruption.
Previous uterine surgery can also weaken the mother’s uterine wall and alter blood flow, increasing the risk for an abruption. A mother may undergo surgery to remove uterine fibroid tumors or to treat other conditions like endometriosis or maternal infections.
Doctors should also thoroughly check the mother’s medical records for any history of chronic high blood pressure or heart disease. These conditions, along with rarer complications like certain blood clotting disorders, can significantly increase her risk for an abruption.
Medical professionals will be able to account for these risk factors during scheduled prenatal testing checkups.
Current Pregnancy
Complications and events that occur during the mother’s pregnancy can call for increased monitoring. Complications like preeclampsia, eclampsia, HELLP syndrome, and hypertension-related conditions all increase her risk for an abruption.
Other placental complications such as placenta previa or nearby infections of the amniotic fluid (chorioamnionitis) can also increase her risk.
Substance abuse during pregnancy (including alcohol, cocaine, and smoking nicotine) can all contribute to a mother’s hypertension and vasoconstriction. This can induce a premature rupture of membranes and even lead to a premature placental separation.
Doctors must carefully watch over a mother during pregnancy, especially when they identify her as high-risk for complications.
Labor and Delivery Complications

Certain complications during labor and delivery can increase a mother’s risk for a placental abruption. Among the highest risk is overly frequent and forceful uterine contractions, known as uterine hyperstimulation. Excessive uterine activity can rupture the blood vessels connecting the uterus to the placenta, causing it to prematurely detach.
A mother may experience hyperstimulation as the result of labor-inducing medications like Pitocin or Cytotec. Doctors typically administer these medications in the event of a prolonged and arrested labor or sometimes for post term pregnancies. While they can successfully induce contractions, some mothers have adverse reactions that cause their uterus to overreact.
Other complications that can contribute to a mother’s risk for abruption include uterine ruptures, premature birth, and twin labor.
Unexpected Trauma

Finally, unexpected traumatic incidents can cause a placental abruption. Incidents like falls, vehicle crashes and blows to the mother’s abdomen can all cause the placenta to prematurely detach.
When a mother sustains unexpected trauma before delivery, she must immediately seek medical assistance in the emergency room. Doctors will be able to perform ultrasound testing to monitor the baby and check for signs of premature placental detachment.
Placental Abruption Risk Factors

Medical History
- Previous placental abruption
- Uterine fibroid tumors
- Prior uterus surgery
- Being an older mother(over 35-40)
- Blood clotting disorders
- Heart disease
- Chronic HBP

Current Pregnancy
- Preeclampsia, eclampsia, HELLP, and hypertension-related conditions
- Substance abuse: alcohol, cocaine, and smoking
- Infections of the uterus, placenta, or amniotic fluid
- Early rupturing of membranes (PROM)

Unexpected Trauma
- Falls
- Vehicle accidents
- Violence including blows to the abdomen
Doctors and other healthcare providers should watch closely for signs of complications like abruption, regardless of the mother’s risk assessment.
What Are Signs of a Placental Abruption?

A placental abruption most commonly occurs in the late third trimester in the weeks leading up to delivery. But it can also occur during delivery itself.
If the following symptoms appear, the mother may need additional testing, closer observation, or admission to the nearest hospital:
- Vaginal bleeding during pregnancy: This is one of the most common signs of abruption. A mother’s placental abruption can cause bleeding that ranges from light to heavy. However, not all expecting mothers with abruptions will have significant vaginal bleeding. Concealed placental abruptions do not come with any vaginal bleeding, but they can still present serious problems. It’s also important to note that other complications beyond abruption can cause bleeding. Not all cases of bleeding during pregnancy stem from placental abruptions.
- Abdominal Pain: A placental abruption may cause the mother to experience lower abdominal pain. This can range in severity between light cramping and severe, sharp pains that come on suddenly. The mother may also report feeling pain in her lower back.
- Uterine changes: The mother may experience tenderness, pain, rigidity, or contractions after a placental abruption. She may report feeling her uterus “expanding”; this can occur due to blood accumulating behind it.
- Decreased Fetal Movement: Placental abruptions can limit the baby’s oxygen supply, resulting in less fetal movement around the mother’s womb.
It’s particularly critical to monitor women in the last trimester of pregnancy. Most placental abruption cases occur just a few weeks before a woman’s due date.
Expectant mothers should notify their doctors when they feel something is wrong. However, it’s even more crucial for medical providers to react quickly and appropriately with treatments. The appropriate protocol for an abruption ranges from additional bed rest to an emergency C-section.
How Do Doctors Diagnose a Placental Abruption?

Obstetricians and other medical professionals can use several diagnostic tools to confirm a mother’s suspected placental abruption. Getting a detailed report of the mother’s medical history should always be their first step. This can provide clues to any conditions that make placental abruption more likely.
After getting context, medical professionals can use ultrasounds and blood testing to uncover more information.
- Ultrasounds can show the doctor the placement of the placenta– top, side, front, or back of the uterus.
- Blood tests can give doctors a good baseline to start. They can evaluate subsequent blood tests against the baseline to watch for troubling changes.
One test – the Kleihauer-Betke test – can detect fetal blood cells within the mother’s bloodstream. Their presence does not always indicate placental abruption, but it proves that the fetus’s blood has mingled with the mother’s.
Beyond ultrasounds and blood testing, doctors should also:
- Monitor any vaginal bleeding and get a sense for how much blood the mother has lost
- Monitor the mother’s blood pressure
- Monitor fetal heart rates
- Monitor uterine contractions
Failing to identify and treat placental abruption puts both the mother and the baby at risk. Such inaction may also count as medical negligence or medical malpractice when it results in otherwise preventable injuries.
What Are Complications of a Placental Abruption?

A placental abruption is a medical emergency that comes with serious risks for both the mother and her unborn baby. Depending on when the placenta detaches and how severe it is, the following may happen:
Postpartum Hemorrhaging
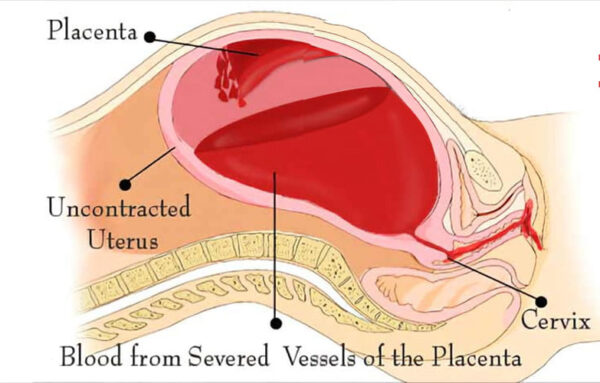
The accumulation of blood between the placenta and uterus can lead to uncontrollable hemorrhaging after the baby delivers. This is because an abruption can disrupt the uterus’s ability to contract, leaving the uterine blood vessels open and exposed.
Blood Clotting Disorders

The rupturing of maternal blood vessels from an abruption can flood the mother’s bloodstream with thromboplastin. This is a substance that initiates blood clotting by converting prothrombin to thrombin in the blood.
The blood pooling between the placenta and uterine wall after an abruption also puts the mother at risk for clotting. Doctors refer to this as a retroplacental hematoma, and it can cause further placental separation from the uterine wall.
Uteroplacental Insufficiency

Premature placental detachment can weaken or entirely disrupt the placenta’s ability to distribute blood, oxygen, and nutrients to the baby. As a result, the baby may have stunted growth (known as intrauterine growth restriction) and have complications at birth. The baby may also suffer from oxygen deprivation, putting them at a higher risk for brain injuries from fetal hypoxia.
Premature Delivery

When the placenta prematurely detaches, it can rupture the amniotic sac surrounding the fetus (known as premature rupture of membranes). This can trigger labor early before the baby fully develops, putting them at risk for birth complications. Common complications of a premature delivery include low birth weight, respiratory distress syndrome (RDS), and underdeveloped brains.
A high percentage of children delivered early go on to receive a cerebral palsy diagnosis in early childhood.
Emergency C-section

When a mother’s abruption results in dangerously low fetal heart rates, doctors have no choice but to deliver the baby. They must sometimes do this via an emergency C-section procedure if the baby is not yet due for delivery.
C-sections are hard on the mother’s body but are sometimes the best chance for avoiding hypoxic brain injuries like HIE. Delaying a C-section procedure can prolong a child’s perinatal asphyxia and increase their risk for permanent birth injuries.
Maternal Mortality

Severe placental abruptions can cause major maternal hemorrhaging, shock, and organ failure (especially in the kidneys due to blood loss). Though modern medicine greatly reduces the mother’s risk, these complications can become fatal when doctors fail to intervene.
Can A Baby Survive A Placental Abruption?

It is possible for a baby to survive following a mother’s placental abruption. However, their chances for survival will depend on timing, severity, and how soon the mother received treatment.
A delay in treatment can result in multiple minutes or even hours with reduced fetal oxygenation. This can cause brain damage at birth like hypoxic ischemic encephalopathy (HIE), which has permanent effects to the child’s wellbeing.
If the abruption occurs early in the mother’s pregnancy, premature birth becomes likely. This can impact the baby’s development and lead to multiple issues at birth. Some infants will not survive these complications.
If a severe abruption occurs before the fetus is viable for delivery, there becomes a high chance of fetal demise. Stillbirth can also occur during labor and delivery if medical professionals cannot respond to fetal distress quickly enough.
The majority of babies survive following a mother’s placental abruption. Their chances of survival increase with timely medical care.
How to Treat Placental Abruption?

Treatment for a placental abruption depends on the severity of the situation and when it occurs in the pregnancy. For mild abruptions with no signs of maternal or fetal distress, the doctor may only monitor the situation more closely.
A moderate or severe abruption, on the other hand, requires immediate action. Vaginal birth may happen quickly and can actually be less risky for the mother. But doctors will typically make the call to perform an emergency C-section when they see signs of fetal distress. Waiting for vaginal birth despite non-reassuring heart rates can increase the baby’s risk for injuries like hypoxic ischemic encephalopathy (HIE).
If the baby is not close to term, there becomes a high risk for premature birth. Doctors may administer corticosteroids like Betamethasone to advance lung development, giving the baby their best chances against birth complications.
Doctors may administer labor-inducing medications to prompt a mother’s delivery. They must closely monitor her contractions alongside the baby’s heart rate to ensure uterine hyperstimulation does not occur.
Frequently Asked Questions About Placental Abruption
What Does a Placental Abruption Feel Like?
A placental abruption may cause sharp, shooting pains in the mother’s lower abdominal region. She may also feel that pain extend to her lower back. She may feel light or moderate vaginal bleeding, which is a sign that her condition is critical.
Severe abruptions with significant blood loss may make the mother feel dizzy and weak. It can also induce labor contractions, meaning birth is imminent.
Is Placental Abruption Hereditary?
Research studies suggest that placental abruptions may have a genetic component, with family members found to have an elevated risk. However, other genetic risk factors (such as hereditary high blood pressure) likely play a larger role in predicting risk.
Can Placental Abruption Kill the Mother?
Yes, placental abruptions can result in maternal mortality from postpartum hemorrhage or organ failure. However, a mother’s risk decreases when she receives timely and adequate treatment from medical professionals. Medical negligence will only increase her maternal mortality risk.
Can You Get Pregnant Again After a Placental Abruption?
Yes, it is possible for a mother to have a successful pregnancy following a placental abruption. However, her chances for a second abruption significantly increase, classifying her pregnancy as high risk. Careful monitoring during prenatal testing is critical to the success of any future pregnancies after an abruption.
Can You See a Placental Abruption on an Ultrasound?
Ultrasound exams can detect placental abruptions usually by revealing the presence of blood accumulated between the placenta and uterine wall. But ultrasounds do not have a 100% success rate in identifying placental abruptions, especially a mild concealed abruption. Medical professionals will typically use a combination of diagnostic tools along with an ultrasound to confirm suspicions of abruption.
Did Doctors Mismanage My Placental Abruption?

Doctors, nurses, midwives, and hospitals have a duty of care to their patients. The following medical errors in response to a mother’s placental abruption can cause further injury or even death:
- Failing to identify that an expecting mother is high-risk for placental abruption.
- Understanding the risk but failing to monitor both mother and baby closely.
- Missing the signs of placental abruption.
- Failing to identify signs of maternal and fetal distress
- Delaying an emergency C-section despite signs of fetal distress
- Failing to protect the baby from brain damage, hypoxic ischemic encephalopathy, and death
If you believe the mismanagement of a placental abruption harmed you or your baby, contact one of our top rated birth injury attorneys. We can help you determine the strength of your case and explain your legal rights and options.
Families who have experienced the effects of birth injuries from negligent medical care deserve to know whether they were avoidable. Our birth injury lawyers help you seek justice and compensation for preventable injuries by proving medical negligence occurred. We handle medical malpractice cases involving birth injuries to babies and for mothers injured from mismanaged labor and delivery complications.
What is the Statute of Limitations in a Birth Injury Case?
A statute of limitations (SOL) is a law that sets a time limit on how long an injured person has to file a lawsuit after an accident. It is essential to understand that statutes of limitations vary based on the case and the state where you file. For instance, the deadline for birth injury claims is typically different from other claims, such as injury to private property.
Generally, the clock starts ticking on the date the injury occurred. However, there are exceptions to this rule. In some cases, the statute of limitations starts when a person discovers or reasonably should have discovered an injury. When dealing with government agencies, SOLs can become even more complex.
For example, if the party that injured you was:
- A federal employee
- Employed by a military hospital, Veterans Administration facility, or a federally funded medical entity
You may need to file a birth injury claim under the Federal Tort Claims Act (FTCA). In FTCA cases, claimants must go through certain administrative procedures before filing a lawsuit. In some states, you may have less time to give notice if:
- The negligent party was a local or state government hospital
- The doctors and medical providers are employees of a governmental entity
If you file your case outside of the statute of limitations, the court will typically dismiss it. This means you will not be eligible to recover compensation for you or your child’s injuries.
Determining when a statute of limitations begins on your case can be tricky. Our birth injury lawyers can help inform you of all the important filing cutoff dates in your state. We will help your family seek justice and compensation for preventable injuries to you or your baby.
How Can Our Birth Injury Attorneys Help?

Most placental abruptions are manageable without causing permanent harm to the mother or her baby. However, it takes an expert review of the facts of your birth to determine whether medical professionals made preventable errors.
Our Process
Our team of committed attorneys, nurses and paraprofessionals works to answer these questions and seek compensation. We use our detailed medical negligence case review process to assess your potential birth injury case.
We start by learning more about your pregnancy by gathering records to determine what happened during and after your delivery. This includes evaluating the fetal heart rate strips during labor and the time it took to perform an emergency C-section.
We will call in skilled medical experts who review your records and provide insight into where medical professionals went wrong. If we feel medical negligence caused your postpartum injuries or your baby’s brain injuries, we contact you to discuss further.
We will help your family seek justice and compensation for preventable injuries by proving medical negligence occurred.
At no point in our legal intake process will we ask you to pay anything. The medical review of your case and the consultation are free. We only receive payment once you do. The sooner you reach out, the sooner we can investigate your case and gather the evidence to support your claim.
We work on a contingency fee basis, meaning you will not pay any legal fees until we win your case. We do not purse any medical malpractice cases unless we fully believe we can win.
Contact us today to schedule your free consultation by calling our toll-free line at (888) 987-0005. You can also reach us by filling out our online request form.
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.