Placental Complications
Placental Complications During Pregnancy
The placenta plays an incredibly important role in a baby’s development inside the womb. It is the source of vital nutrients, hormones, and oxygen that keeps the fetus alive and prepares the mother’s body for pregnancy.

Placental complications, including ruptures, blocking the cervix, or implanting too deeply into the uterine wall, can threaten the mother’s and her baby’s health by causing dangerous labor and delivery complications.
Some of these pregnancy complications can be caught and treated or planned for early with proper prenatal testing. When healthcare professionals miss the signs of a placental pregnancy complication or mistreat a placental issue after birth, it can lead to a preventable birth injury and may count as medical malpractice.
Free Legal Consultation
Birth Complication Lawyers
(888) 987-0005Our Birth Injury Lawyers are available to meet you in your home or the hospital.
Over the past three decades, the nationally recognized team of birth injury lawyers, registered nurses, and nurse-attorneys at Miller Weisbrod Olesky have established a proven track record of delivering justice for children and families across the United States who have suffered from all types of birth injuries, including maternal injuries from placental complications.
We are prepared to meticulously investigate the circumstances of your case, gather crucial medical records, consult with top medical experts, and fight tirelessly to secure the compensation you deserve for your child's injury.
We represent families and their birth-injured children throughout the United States. You can contact us today to schedule your free legal consultation by calling our toll-free line at (888) 987-0005 or by filling out our online request form. We work on a contingency fee basis, meaning you won't pay any legal fees unless we win your case. We only receive payment once you do.
What is the Function of the Placenta?
The placenta is an organ that develops at the beginning of pregnancy as the mother’s fertilized egg implants into her uterus and transitions into an embryo. It starts as only a few cells and grows as the fetus does, eventually measuring several inches in diameter.
Attached to the uterine wall, the placenta takes in the mother’s oxygenated blood and diffuses the oxygen and nutrients from it using tiny threadlike membranes called villi.

The placenta then delivers the nutrients and oxygen to the fetus through the umbilical cord. It also filters out carbon dioxide and waste products expelled by the fetus. The placenta functions as the baby’s vital organs, acting as its lungs, liver, and kidneys.
The changes a mother experiences during pregnancy stem from the hormones that her placenta produces, namely estrogen, progesterone, lactogen, and human chorionic gonadotropin (hCG).
As the mother’s pregnancy progresses, the placenta passes antibodies to the fetus to build up its immunity to germs. This immunity stays with the baby after birth and into the first few months of life. After delivering her child, the mother will “deliver” her placenta as it detaches from her uterus and expels out through her birth canal.
What are Common Risk Factors for a Placental Complication?
Sometimes placental complications occur for unknown reasons. Certain complications like placenta accreta appear to be related to genetics and medical history, but other complications like placental abruptions have causes that can be pinpointed.

In all cases, research has marked certain conditions and experiences as risk factors that increase a mother’s chances of having a placental complication. These risk factors can include:
- Previous history of a placental complication
- Previous reproductive surgery such as dilation and curettage (D&C) or a myomectomy (removal of the uterine fibroids)
- Advanced maternal age (over 35 years)
- Maternal infections
- Previous C-section delivery
- Twin pregnancy
- Hypertension or preeclampsia diagnosis
- Premature birth
- Blood clotting conditions
- Umbilical cord problems
- Substance abuse, including the excessive use of alcohol, cocaine, and cigarettes
- Accidents such as falls, car crashes or any other unexpected trauma
These factors may increase a mother’s risk for a placental issue, but they aren’t always guaranteed to. Other unseen factors can play a role too, such as genetic mutations. Healthcare professionals must be aware of the known risks and prepare for medical intervention should a placental complication arise.
What are Different Types of Placental Complications?
Placental complications can range from abnormal placing and implantation to tearing and rupturing of the membranes and blood vessels. The following examples are the most common complications that can threaten the wellbeing of a mother and her child during pregnancy, during labor and delivery, and shortly after birth:
Placenta Previa
Placenta previa is a pregnancy complication where the placenta fully or partially covers the cervix (the uterus opening). In normal conditions, the placenta is attached to the top of the inner uterine walls, but with placenta previa, it attaches lower.

The condition can usually be diagnosed early during prenatal testing with an ultrasound exam. Some patients with undiagnosed placenta previa may experience painless vaginal bleeding and visit the ER during the second or third trimester.
When an expectant mother has placenta previa, it may cause the blood vessels connecting the placental tissue to the uterus to tear at the time of labor or delivery. This can cause severe bleeding which will result in fetal distress if not immediately addressed with an emergency c-section.
The biggest risk of placenta previa is that it can cause major internal hemorrhaging inside the mother’s uterus if a vaginal birth is attempted.
While growing in the womb, the baby’s head will continue to place increasing pressure on the placenta, which will eventually lead to a placental abruption if not addressed quick enough. Placenta previa can even cause severe bleeding after birth, endangering the life and welfare of the mother if the bleeding is not stopped.
Another potential complication of placenta previa is premature birth. The complication can sometimes necessitate an emergency cesarean delivery before the baby has reached full term.
Nearly 15% of expectant mothers with placenta previa will deliver before the 34th week of pregnancy. This increases the baby’s risk of preterm birth related complications, such as fetal distress due to lack of oxygen or hypoxic-ischemic encephalopathy (HIE), which could lead to cerebral palsy.

Placenta previa can sometimes be accompanied by other placental issues, such as a placental abruption or placenta accreta. According to researchers, placenta previa is also the single most common placenta-related cause of anemia in infants.
Because of these major health risks to the both the mother and her baby, healthcare providers and all specialized medical teams must do their due diligence when observing and planning for placenta previa to minimize as much harm as possible.
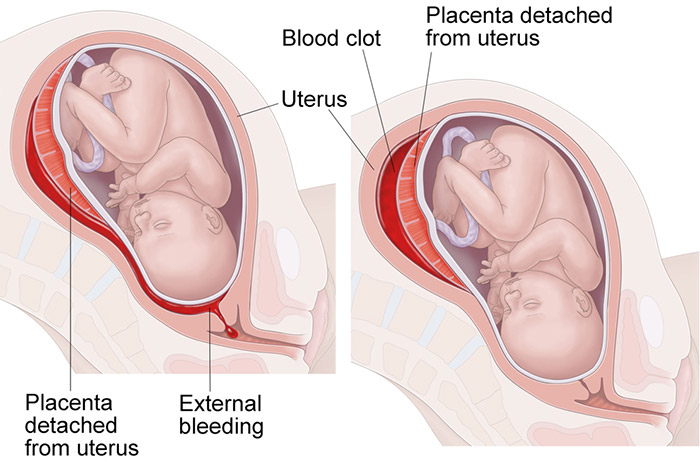
Placental Abruption
A placental abruption is a labor and delivery complication that occurs when the placenta prematurely separates from the uterus for any given reason. In a typical pregnancy, the placenta separates from the uterus after the baby is born. In fact, its removal is often referred to as the “third stage of labor.”
Since the uterus is a muscle, it is more “elastic” than the placenta. Sometimes when the uterus stretches or moves for some reason (like trauma or prolonged excessively hard or long contractions from uterine hyperstimulation), the placenta does not move, causing it to separate from the lining.
The resulting accumulation of blood also causes them to further separate. For some mothers, the blood remains trapped in the uterus instead of being expelled through the vagina.
This separation also puts the baby at risk as the placenta’s ability to provide oxygen weakens. A baby receiving less oxygen may show signs of fetal distress as their heart attempts to compensate. This, then, can lead to hypoxic-ischemic encephalopathy (HIE) as the flow of oxygenated blood to the brain decreases.

Babies in fetal distress typically must be delivered quickly, sometimes by emergency C-section. Sometimes a C-section may be necessary before the baby is fully developed, resulting in a premature birth.
Placental abruptions can be categorized into increasing levels of severity. A partial abruption happens when the placenta doesn’t fully detach from the uterine lining.
A complete abruption or total abruption means that the placenta is fully detached. The classes of a placental abruption categorize the severity of symptoms a mother experiences.

A placental abruption is a medical emergency that healthcare professionals must quickly respond to in order to avoid infant death or serious birth complications and maternal injuries. Failing to respond quick enough can constitute medical malpractice in some cases.
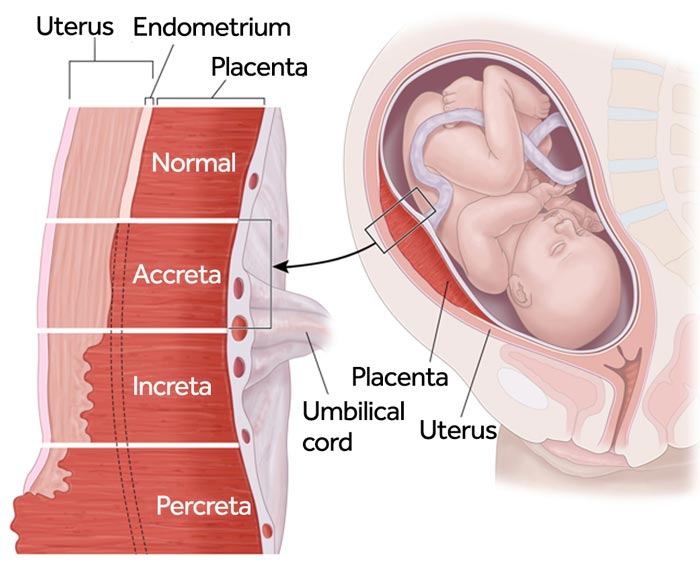
Placenta Accreta
Placenta accreta is a pregnancy complication where the mother’s placenta implants too deep into the uterine wall. While the placenta is supposed to attach to the wall of the uterus, it may not detach properly after birth if it is embedded too deep into it.
There are three types of placenta accreta that increase in severity:
More severe forms of placenta accreta (increta and percreta) are often accompanied by placenta previa. This can cause a placental abruption during labor and delivery and lead to excessive bleeding for the mother. Doctors often opt to deliver the baby early to minimize these risks. In cases where placenta previa is suspected, they may require a planned C-section procedure.

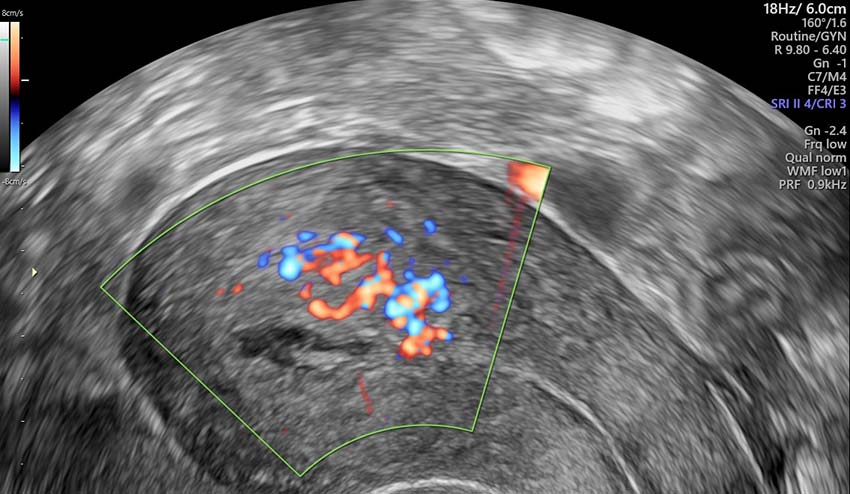
Placenta accreta can normally be caught during prenatal testing with ultrasounds or magnetic resonance imaging (MRI) scans. An early diagnosis gives healthcare providers more time to plan for treatment options, but sometimes the condition can go unnoticed until the mother has given birth and hasn’t delivered her placenta within 30 minutes after.
Doctors, nurses, and other specialized medical professionals must be able to identify an expecting mother’s risk for placenta accreta and know how to treat it along with any birth related complications.
Placental Insufficiency (IUGR)
Placental insufficiency is a pregnancy complication in which oxygen and vital nutrients are not properly delivered to the fetus.
It has also been recorded in post term pregnancies (pregnancies exceeding 40 weeks gestation). When a fetus does not receive sufficient nutrients from the placenta, they become at risk for intrauterine growth restriction (IUGR), a complication where the baby’s size is abnormally small.
Babies with IUGR are at a higher risk for birth injuries like hypoxic-ischemic encephalopathy (HIE), which is the leading cause of cerebral palsy. Placental insufficiency contributes to this risk because the placenta is the baby’s main source of oxygenation and blood flow.
When the placenta’s function is diminished, it increases the risk of hypoxia (restricted oxygen) and ischemia (restricted blood flow), the two factors that HIE encompasses.
Placental insufficiency can normally be detected during prenatal testing through ultrasounds, which detect blood flow between the placenta and the fetus. An OB-GYN may suspect insufficiency if the fetus’s size is abnormally small or if they observe limited movement.
Treating placental insufficiency depends on what stage of pregnancy the mother is in. If it occurs toward the end stages of pregnancy in the third trimester, doctors may suggest using labor inducing medications when safe enough to do so. In cases of premature birth, doctors may also prescribe corticosteroids such as Betamethasone to help with fetal lung development and avoid respiratory distress syndrome and other complications.
Retained Placenta
A retained placenta or retained products of conception (RPOC) is a labor and delivery complication where, after birth, the mother’s placenta or traces of placental tissue remain stuck inside her uterus. This can happen after a traditional birth or in cases of miscarriage, such as an ectopic pregnancy or a blighted ovum miscarriage.
It’s important to note that RPOC isn’t always the same as a retained placenta; retained products of conception can refer to other fetal tissue or waste products outside of the placenta. Both complications are rare.
Risk factors that increase the likelihood of a retained placenta include prolonged and arrested labors and assisted deliveries with forceps and vacuum extractors. It can also be caused by placenta accreta because of its deep embedding within the uterine wall.
A retained placenta typically doesn’t cause complications to the baby, but the mother can sustain injuries from it including bleeding, blood clots, and maternal infections that can develop into sepsis.
To avoid these risks, doctors sometimes opt to perform a surgical operation to remove the mother’s placenta when it won’t pass on its own. In other cases, doctors may prescribe the mother medications that induce labor contractions as a way to force the placenta out.
Healthcare professionals must closely monitor the mother after her child is born to ensure that she passes the placenta fully during the critical “third stage of labor” to avoid any maternal complications from retained products of conception.
How to Diagnose and Treat Placental Complications?
The majority of placental complications can be spotted during prenatal testing using neuroimaging technology. Ultrasounds, MRIs, and other neuroimaging tests can reveal blood flow moving from the placenta to the fetus. Observing a lack of blood flow can be a sign of placental insufficiency.
They will also be able to locate the placenta’s position within the uterus. Noticing a low attachment can indicate placenta previa. A mother’s symptoms can sometimes indicate a placental complication; sharp abdominal pain and vaginal bleeding can indicate a possible placental abruption, for example.

Other complications, like placenta accreta or a retained placenta, may become visible after the mother has delivered her baby and hasn’t passed her placenta.
Doctors may use one or a combination of the following methods to treat placental complications:
- Observation and Monitoring: Prenatal testing is one of the best preventative measures against birth injuries. Some placental complications, namely placenta previa, have shown to naturally self-correct as the mother’s pregnancy progresses. This happens because the uterus can grow and expand, pushing the attached placenta away from the mother’s cervical opening.
Many cases of placenta previa are self-correcting, so healthcare providers must carefully monitor the situation and potentially schedule additional check ups over the course of the mother’s pregnancy. - Blood Transfusions: A blood transfusion is a medical procedure where someone is given donated blood through an intravenous line (IV) to replace blood or blood components that are too low. For a mother who has experienced a placental abruption, this may become necessary when she’s experienced severe blood loss.
- Emergency Cesarean Delivery: For cases of placenta previa that have failed to self-correct, an emergency C-section delivery may be the safer option to avoid massive hemorrhaging and rupturing of the placenta. It can also be the preferred method of delivery when a placental abruption occurs, too.
A C-section may also be performed in cases of placental insufficiency where vaginal birth or labor induction is considered too risky. Healthcare providers must act quickly when this happens to minimize the risk of fetal distress and hypoxic brain injuries like hypoxic-ischemic encephalopathy. - Surgical Removal of the Placenta: For cases of placenta accreta (especially more severe cases like increta and percreta), surgical removal of a mother’s placenta may be required to avoid the risks and complications of a retained placenta.
This is usually done using an epidural or general anesthetic so the mother feels no pain for the procedure. In some severe cases of accreta, doctors may need to remove the mother’s uterus entirely to avoid the invasion of other tissues and further damage.

When healthcare providers make errors in treatment of placental complications, such as delaying care or missing the complication altogether, it can lead to birth injuries and other maternal complications and count as medical malpractice.
Was My Placental Complication Mismanaged?

In many cases, placental complications can be easily caught and safely managed with proper medical care during prenatal testing. Treatment can vary on the type of complication, but there are typically treatment solutions available to avoid the risk of further complications during pregnancy or during labor and delivery.
Birth injury medical negligence, such as a misdiagnosis or failure to catch early symptoms of a problem, can lead to avoidable birth complications and result in injuries to you or a birth injury for your child.
If a family believes medical negligence worsened a mother’s placental complication leading to a child's birth injury, or even caused the untimely death or the mother, legal support may be an option. A specialized birth injury attorney can review the medical records and circumstances to assess whether a claim exists.
Parents whose children suffer from the long-term effects of their mother’s mismanaged treatment for a placental problem, as well as mothers who were harmed during pregnancy from an untreated placental issue, deserve to know whether it could have been prevented. Our dedicated birth injury lawyers want to help you find those answers and obtain the funds necessary to improve the quality of life for your child.
If your child has been diagnosed with a birth injury and you suspect this may have been caused in part by medical mistakes, Miller Weisbrod Olesky will thoroughly investigate the facts and hold the responsible medical providers accountable by pursuing medical malpractice claims against them.
Sometimes families are hesitant to reach out to a medical malpractice attorney or law firm. They may feel overwhelmed by their circumstances or are worried that a law firm will not be able to help them. But the only way to find out if you have a case is to talk to an attorney who understands how birth injuries can lead to developmental delays and other birth complications that require long-lasting medical support.
What is the Statute of Limitations in a Birth Injury Lawsuit?
A statute of limitations (SOL) is a law that sets a time limit on how long an injured person has to file a lawsuit after an accident. It is essential to understand that statutes of limitations vary based on the type of case and the state where it is filed. For instance, the deadline for birth injury claims is typically different from other claims, such as injury to personal property, fraud, contract disputes, and collection of debts.
Generally, the clock starts ticking on the date the injury occurred. However, there are exceptions to this rule, and in some cases, the statute of limitations starts when a person discovers or reasonably should have discovered an injury. When dealing with government agencies, SOLs can become even more complex.
For example, if the party that injured you was:
- A federal employee
- Employed by a military hospital, Veterans Administration facility, or a federally funded medical entity
You may need to file a birth injury claim under the Federal Tort Claims Act (FTCA). In FTCA cases, claimants must go through certain administrative procedures before filing a lawsuit. In some states, if the negligent party was a local or state government hospital or the doctors and medical providers are employees of a governmental entity, the time period in which you must give "notice" may be shorter.
If your case is filed outside of the statute of limitations, it will typically be dismissed, and you will not be eligible to recover compensation for your injuries. Determining when a statute of limitations begins on your case can be tricky. If you're considering pursuing compensation for a birth injury, contacting an attorney as soon as possible is in your best interest.
How Can the Birth Injury Attorneys at Miller Weisbrod Olesky Help?

Injuries from placental complications can usually be prevented, but it takes a detailed expert review of the facts and circumstances of an infection case determine whether the injury was the result of medical malpractice.
Our Process
At Miller Weisbrod Olesky, a team of specialized birth injury malpractice attorneys, nurses and paraprofessionals uses our detailed medical negligence case review process to assess your potential birth injury case.
We start by learning more about you and your child and the status of meeting/missing developmental milestones. We then gather medical records to determine what happened before, during, and after your delivery. We call in skilled medical experts who review your records and let us know if they think medical errors could have caused you or your child's injuries.
If we feel medical negligence caused or contributed to complications with your pregnancy or your child's injuries, we meet with you to discuss how you can receive compensation from the medical professionals who made the errors.
At no point in our legal intake process will we ask you to pay anything. The medical review of your case and the consultation are free. We only receive payment when you do. The sooner you reach out to us, the sooner we can begin investigating your case and gathering the evidence needed to support your claim.
We work on a contingency fee basis, meaning you won't pay any legal fees unless we win your case. Contact us today to schedule your free legal consultation by calling our toll-free line at (888) 987-0005 or by filling out our online request form.
Contact Miller Weisbrod Olesky
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.