Fetal Alcohol Syndrome
What is Fetal Alcohol Syndrome (FAS)
Fetal Alcohol Spectrum Disorders (FASDs) is an umbrella term for a group of conditions that affect babies whose mothers consumed alcohol during pregnancy. This exposure to alcohol in the womb can cause the child to suffer a wide range of disabilities related to developmental milestones including behavior, learning, and physical developments.
While fetal alcohol syndrome is primarily associated with alcohol consumption during pregnancy and not typically linked to medical errors, doctors and other healthcare providers have a responsibility to provide adequate care to both the mother and her baby throughout pregnancy, labor, and delivery.
If a healthcare provider fails to meet the expected standard of care and causes your child to suffer a preventable birth injury, you may have grounds to seek compensation for the harm caused.

Fetal Alcohol Syndrome (FAS) is considered the most severe type. Some children diagnosed with FAS may experience only mild effects while others face more severe challenges like growth deficiencies and intellectual disabilities.
The severity of symptoms often depends on factors such as how much alcohol a mother consumed during her pregnancy and when the exposure occurred during the developmental stages.
Children exposed to higher levels of alcohol or exposed to harmful substances during critical periods of fetal development are more likely to experience more severe developmental issues, including secondary conditions such as Attention-Deficit/Hyperactivity Disorder (ADHD).
It is important to understand that no amount or type of alcohol is considered safe to drink if you're pregnant or thinking about becoming pregnant. From the moment of conception through to the end of pregnancy, alcohol can interfere with the normal growth and development of your baby's brain and body.
Talk to your doctor or other medical provider as soon as possible if you suspect your child may be affected by prenatal alcohol exposure. Early intervention can make a significant difference in improving outcomes for affected newborns.
At Miller Weisbrod Olesky, our team of dedicated medical malpractice attorneys understand the profound impact that birth injuries can have on victims of medical negligence and their families.
With decades of combined experience successfully handling birth injury cases for our clients in over 20 states, we are confident in our ability to help you secure the justice and compensation you need to move forward and give your child the best possible future.
What Causes Fetal Alcohol Syndrome?
Fetal Alcohol Spectrum Disorders, including Fetal Alcohol Syndrome, occur when a baby is exposed to alcohol before birth. When a pregnant mother consumes alcohol during her pregnancy, it goes into her bloodstream and quickly reaches the fetus by passing through the placenta.
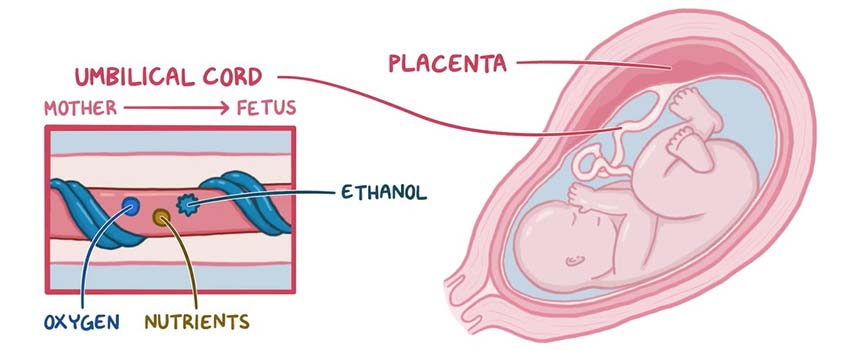
Unlike adults, babies metabolize alcohol much more slowly. As a result, alcohol remains in their system for a much longer period of time compared to the mother, leading to higher blood alcohol concentrations in the fetus.
This prolonged exposure to alcohol and other harmful substances can interfere with the normal development of the fetus in several ways, including:
- Cell Death and Abnormal Physical Development: Alcohol can damage or kill cells in various parts of the fetus's body, leading to abnormalities in physical development.
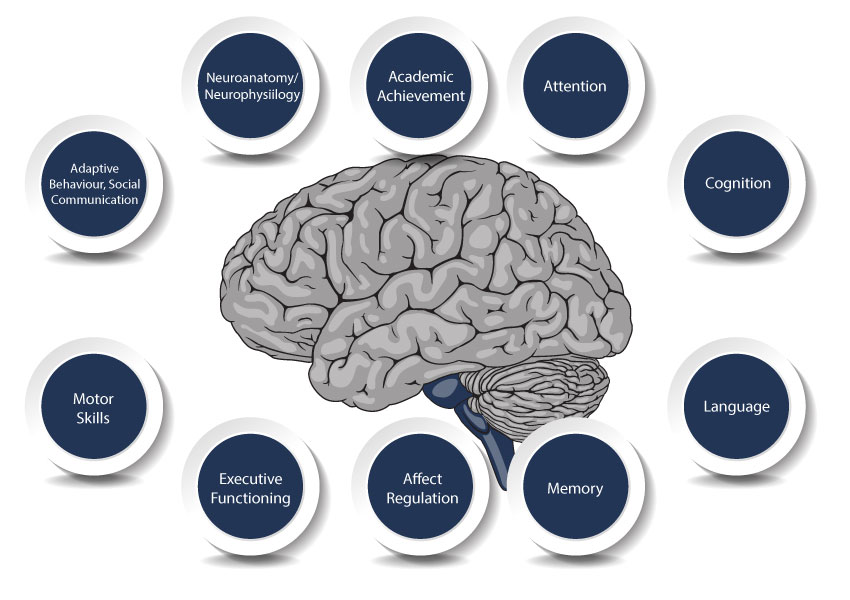
- Disruption of Brain and Nerve Cell Development: Alcohol disrupts the development of nerve cells and affects their ability to properly form connections in different areas of the brain. This disruption impairs the normal functioning of the brain, which can result in cognitive impairments, learning disabilities, and developmental delays.
- Restricted Blood Flow to the Placenta: Alcohol constricts blood vessels, reducing the blood flow to the placenta. This limits the delivery of oxygen and essential nutrients to the fetus, resulting in potential developmental delays, growth restrictions, and increased risk of birth complications such as low birth weight or preterm birth.
- Toxic Byproducts in the Baby's Brain: As the body processes alcohol, it produces toxic byproducts that can concentrate in the baby's brain cells and cause damage. These byproducts, such as acetaldehyde, interfere with the normal growth and function of brain cells. The resulting damage may affect memory, attention, language skills, and overall brain function, often leading to challenges with learning, behavior, and social interactions.
As even small amounts can cause permanent harm to the developing fetus and increase the risk of miscarriage, as soon as you learn of your pregnancy, it is essential to cut out all alcohol from your diet immediately. Similarly, despite its growing popularity for various health conditions, medical marijuana should also be avoided during pregnancy.
Consuming alcohol or using substances like marijuana during the early weeks of pregnancy can impact the development of vital organs, including the brain, heart, and nervous system.
Additionally, as the baby continues to develop, the risk of long-term developmental issues increases with continued exposure to alcohol or marijuana. Provide your baby with the best chance for a healthy start by making the decision to avoid these substances throughout pregnancy.
Diagnosing Fetal Alcohol Syndrome
With no single blood test or other medical test available to diagnose this disorder, healthcare providers must rely on observing a combination of physical, cognitive, and behavioral symptoms over time. Additionally, diagnosing FAS can be tricky because pregnant mothers may not give a complete history of their alcohol intake during pregnancy.

Expectant mothers are encouraged to share this information openly with their child's medical team, as providing a complete health history can help healthcare providers better anticipate the child's needs and the challenges they might face as they grow.
In some cases, a healthcare provider can identify signs of fetal alcohol syndrome at birth if the child is unusually small or exhibits specific physical characteristics. However, for some children, the effects of FAS may not become evident until later in childhood or even adulthood.
Pediatric providers typically evaluate several factors when diagnosing fetal alcohol syndrome (FAS), including:
- The history of alcohol use by the child's mother during pregnancy.
- Distinctive facial features in the child, such as a smooth ridge between their nose and upper lip, a thin upper lip, and small eyes.
- Smaller-than-average size at birth and through childhood.
- Emotional and behavioral difficulties, including trouble focusing, hyperactivity, and poor judgment.
In cases were children experience only a few of the symptoms associated with the condition they may be diagnosed with partial fetal alcohol syndrome. For instance, sometimes, the distinctive physical facial features of FAS may not develop in a child whose mother drank alcohol later in pregnancy.
If you suspect your child has FAS, you should consider discussing your concerns with your doctor. Your child's doctor may refer you to a specialist who can perform a more comprehensive evaluation of your child's condition.
This evaluation may involve collaboration among a team of specialists, including a developmental pediatrician, neurologist, speech therapist, psychologist, and occupational therapist. These professionals can provide a clearer picture of areas where your child may need support and recommend targeted interventions to help optimize their potential.
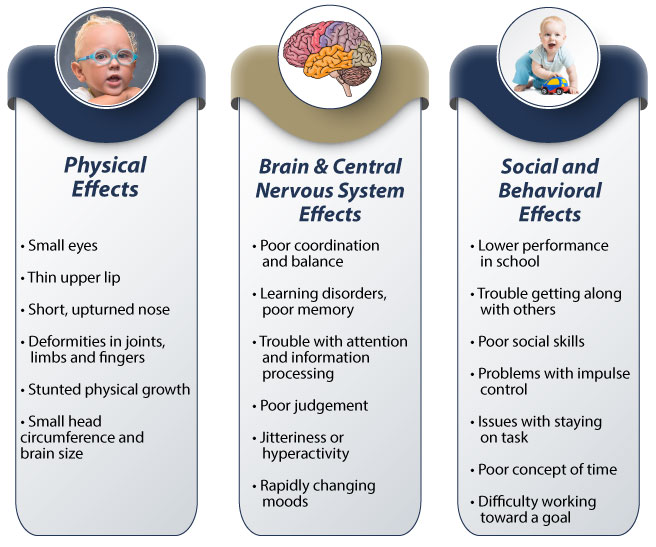
Signs and Symptoms of Fetal Alcohol Syndrome
The severity of FAS varies and depends on several factors, such as the amount of alcohol consumed by the mother and what stage of pregnancy the mother was in when the alcohol was consumed. While some children may exhibit only a few signs, others may experience a full spectrum of challenges.
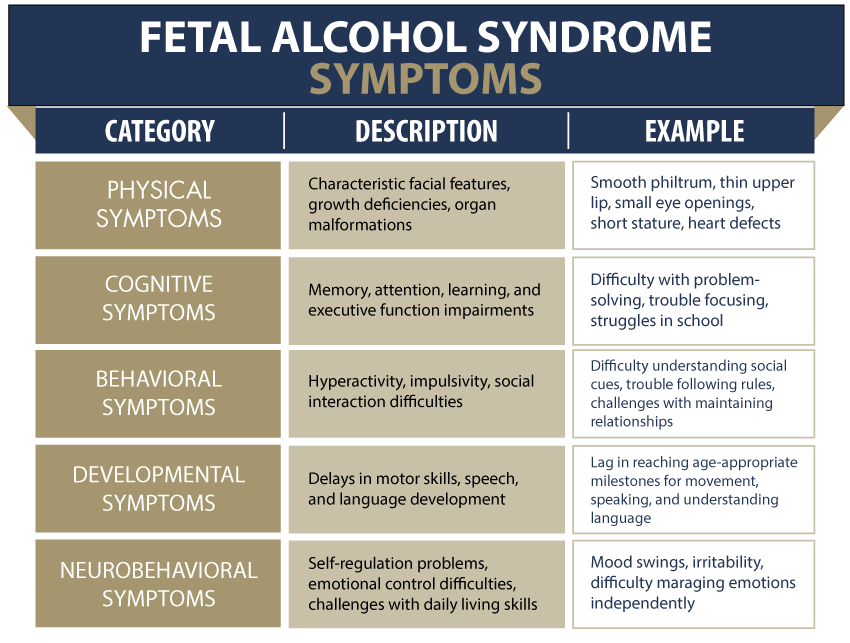
Children with fetal alcohol syndrome often experience symptoms that affect different aspects of their development, ranging from physical growth issues to cognitive and behavioral challenges. The level of support a child born with fetal alcohol syndrome may require will depend on how severe their disability is and how early the condition is diagnosed and treated.
Physical Characteristics and Developmental Delays
- Small eye openings, a smooth area between the nose and upper lip (philtrum), a flat nose bridge, and a thin upper lip. These features may remain the same as the child grows or fade over time
- Low birth weight, slow physical growth, and shorter-than-average height
- Smaller head size or brain abnormalities
- Skeletal malformations or issues with vital organs, especially the heart and kidneys.
- Poor coordination or balance and difficulty reaching developmental milestones (i.e. sitting, walking, talking)
- Sleep and sucking difficulties as a baby
- Vision or hearing problems
Cognitive and Learning Challenges
- Issues with memory, understanding, and following directions
- Low IQ, difficulty learning new information, and a short attention span
- Learning disabilities, particularly in subjects like math, language, and problem-solving
- Challenges with reasoning, judgment, and decision-making in daily situations
- Poor concept of time that affects following schedules, knowing when to leave to arrive on time, and understanding how long tasks will take
- Trouble with organizing and planning or working toward a goal
Behavioral and Emotional Difficulties
- Hyperactivity, impulsivity, and difficulty focusing
- Problems with social interactions, including struggles with communication, emotional regulation, and adapting to changes
- Difficulty distinguishing between reality and fantasy
- Trouble forming friendships with peers or adults because they may behave younger than or inappropriately for their age
- Easily influenced by others or taken advantage of
Over time, some children with FAS may develop secondary conditions including:
- Attention-deficit/hyperactivity disorder (ADHD), intellectual disabilities, and seizure disorders
- Increased risk for mental health disorders (i.e., anxiety, depression, mood disorders) and substance misuse
- Impulsivity and social issues that may lead to trouble with the law or engaging in risky behaviors
Although Fetal Alcohol Syndrome is typically not caused by medical negligence, there are situations where inadequate prenatal care or failure to address potential risks during pregnancy could exacerbate the effects of fetal alcohol syndrome.
In these cases, a skilled medical malpractice attorney can determine whether medical negligence played a role in the child's condition and ensure that affected families receive the compensation they need to support their child's long-term care and development.
Types of Fetal Alcohol Spectrum Disorders
Fetal alcohol spectrum disorder is a broad term that encompasses a range of physical, cognitive, and behavioral issues caused by alcohol exposure during pregnancy. When a fetus is exposed to alcohol before birth, it can affect their development in various ways.
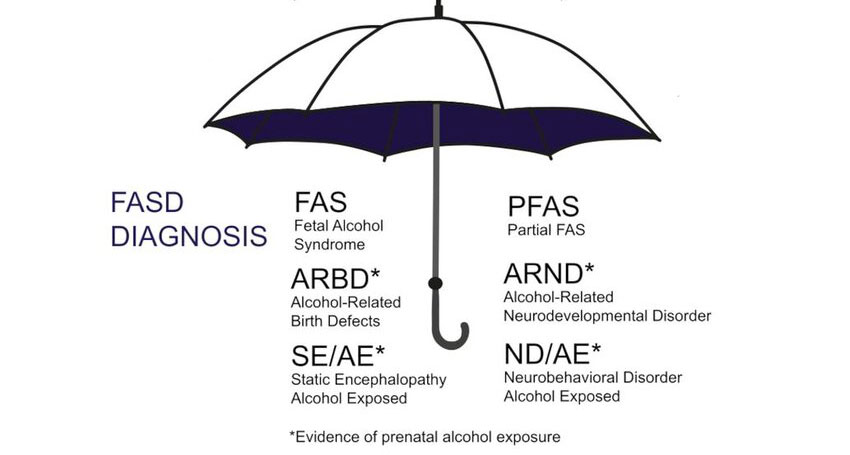
The effects of alcohol can range from mild to severe, with different disorders falling under the FASD umbrella. Fetal alcohol syndrome is the most severe form within this spectrum. FAS is characterized by a combination of distinct physical features and severe cognitive impairments that typically affect the child's ability to function and engage in day-to-day activities.
There are other conditions within the FASD spectrum that are less severe but still linked to prenatal alcohol exposure. These include:
- Partial fetal alcohol syndrome (pFAS): Children with partial fetal alcohol syndrome may exhibit some of the characteristics of FAS, such as specific facial abnormalities and growth delays. However, they typically do not display all the symptoms associated with FAS.
- Alcohol-related neurodevelopmental disorder (ARND): This condition primarily affects cognitive functions, including memory, attention, and problem-solving skills. Children with ARND may struggle with impulse control, judgment, and academic performance but generally do not have the physical traits of FAS.
- Alcohol-related birth defects (ARBD): These are physical defects that can affect various organs, such as the heart, kidneys, eyes, ears, and skeletal system. Some children may be born with heart abnormalities, such as atrial or ventricular septal defects. Others might experience kidney issues, including structural malformations or reduced function that affect their body's ability to maintain fluid and waste balance.
- Neurobehavioral disorder associated with prenatal alcohol exposure (ND-PAE): This condition occurs in children who were exposed to substantial amounts of alcohol before birth. These children may struggle with daily tasks, such as bathing and dressing, and can face challenges in social situations due to intense behavioral issues like severe tantrums. Additionally, they often experience difficulties with memory, focus, and problem-solving skills.
While each condition presents unique challenges, early diagnosis, and timely intervention can help children living with FASDs manage their symptoms more effectively, improve their cognitive and social skills, and promote greater independence. A healthcare provider can play a crucial role in developing a personalized treatment plan that addresses the child's specific needs and equips them with the skills they need to succeed in daily life.
Treatment for Fetal Alcohol Syndrome
Fetal alcohol syndrome or other FASDs aren't curable. Children born with this syndrome will be impacted by the symptoms throughout their lives. However, many of these symptoms can be effectively managed with early intervention, tailored support, and ongoing care.

Treatment options for FAS may include:
- Medication: Doctors may prescribe medications to address specific symptoms like attention and behavior issues. These medications can help children manage conditions such as ADHD, anxiety, depression, and aggression. However, it is crucial for parents and caregivers to work closely with medical professionals to monitor the effects of medications and adjust them as needed.
- Behavioral Therapy: Children can benefit from therapy to address emotional and learning concerns. Behavioral therapy can help children develop coping strategies to manage impulsivity and improve their emotional regulation. For example, a child with FAS may struggle with outbursts when they become frustrated or overwhelmed. Through behavioral therapy, the child could learn to recognize the early signs of frustration and use coping techniques, such as deep breathing, to calm themselves before reacting.
- Physical and Occupational Therapy: These therapies work together to support children with FAS in improving their physical abilities and daily functional skills. Physical therapy focuses on enhancing gross motor skills, such as strength, coordination, balance, and mobility. On the other hand, occupational therapy focuses on teaching children how to perform daily activities like dressing, using utensils, and writing. Additionally, occupational therapists often work with children to enhance sensory processing skills. This aspect of therapy focuses on helping children become more comfortable with sensory stimuli, such as touch, sound, or light.
- Speech and Language Therapy: Many children with FAS experience speech and language development delays. Speech and language therapy focuses on improving communication skills, such as articulation, vocabulary, and comprehension. This therapy helps children express themselves more clearly, understand others, and engage in meaningful conversations.
- Special Education Services: Children with FAS may struggle with academic challenges, including difficulties with reading, writing, and math. Special education services and tutoring can help these children overcome learning barriers and improve their academic performance. Additionally, special education services often include social skills groups. Children living with FAS can enhance their ability to interact with peers and form relationships through these groups.
- Counseling with a mental health professional: A mental health professional can work with the child to address emotional challenges such as anxiety, depression, or frustration. Through counseling, children can learn coping mechanisms to manage stress, express their emotions in a healthy way, and build confidence. Mental health support can also provide parents and caregivers with strategies to handle difficult behaviors and create routines that promote stability.
In managing the challenges of fetal alcohol syndrome, family education is an essential component of a comprehensive treatment plan. Providing a stable, nurturing, and safe home environment can also significantly reduce the long-term impact of FASD on a child's development.
In looking for ways to ease the problems of your child living with fetal alcohol syndrome, don't be afraid to get help. Your child's doctor or other members of your child's care team can guide you toward the appropriate resources and support systems.
For example, through parent training, caregivers can learn how to create a predictable environment that supports their child's growth. Additionally, a birth injury attorney can be a valuable ally for families who may be struggling with the financial burden associated with caring for a child living with a birth injury.
Can Fetal Alcohol Syndrome (FAS) Be Prevented?
In the United States, alcohol use during pregnancy is a leading cause of preventable birth injuries, birth defects, and intellectual disabilities. The good news is that fetal alcohol syndrome is entirely preventable when alcohol is avoided throughout the entire pregnancy.

Women who are trying to conceive or who suspect they may be pregnant should avoid alcohol altogether. If a woman does consume alcohol during pregnancy, stopping as soon as possible can significantly reduce the risks to her baby's health and minimize the chances of FAS-related complications.
Here are some essential steps to take to prevent fetal alcohol syndrome:
- Stop drinking if you're trying to get pregnant: It's important to avoid alcohol while trying to conceive. If you're not yet pregnant but suspect you may be, stop drinking immediately. It can take four to six weeks to confirm a pregnancy, and alcohol can impact the developing fetus during this time.
- Avoid alcohol during early pregnancy: The early stages of pregnancy are crucial for fetal development. During this time, the baby's organs and brain are rapidly forming, and any exposure to alcohol can interfere with this delicate process.
- Consider avoiding alcohol during your childbearing years: If you are sexually active and not using reliable contraception, it's wise to avoid alcohol. Many pregnancies are unplanned, and the early weeks of fetal development can occur before you even realize you're pregnant. By eliminating alcohol during this time, you reduce the risk of harming a potential pregnancy.
- Be mindful of alcohol consumption while breastfeeding: After giving birth, it's essential to be mindful of alcohol consumption if you are breastfeeding. Alcohol can pass into your breast milk, potentially affecting your baby's development and health. To minimize the risks, waiting at least two hours after consuming one drink before nursing or pumping milk is recommended. It's also a good idea to talk to your child's healthcare provider to learn the best practices for alcohol use while breastfeeding.
If you struggle with alcohol use, talking to a healthcare provider or mental health professional before you get pregnant is crucial. They can help you assess your alcohol intake and work with you to develop a tailored plan to quit. Remember, it's never too late to make a positive change. The sooner you stop drinking, the greater the chances of reducing the risks of fetal alcohol syndrome and related complications during pregnancy.
How Common Is Fetal Alcohol Syndrome (FAS) and Alcohol Use During Pregnancy?
The exact prevalence of fetal alcohol spectrum disorder (FASD) is difficult to determine due to factors such as underreporting, misdiagnosis, and lack of awareness. Estimates suggest fewer than 0.5 to 2 cases of FASD occur per 1,000 live births in the U.S. However, according to a study supported by the National Institute on Alcohol Abuse and Alcoholism (NIAAA), broader estimates indicate that 1% to 5% of U.S. first graders may be affected by FASD.

Alcohol use during pregnancy has remained a significant concern over the years. Data from the National Survey on Drug Use and Health (2015-2018) revealed the following alarming statistics:
- About 1 in 10 (9.8%) pregnant women reported current alcohol use
- Approximately 1 in 22 (4.5%) reported that they engaged in binge drinking.
- Alcohol consumption was most prevalent during the first trimester, with 1 in 5 (19.6%) women reporting alcohol use and 1 in 10 (10.5%) engaging in binge drinking.
- Nearly 40% of pregnant women who reported alcohol use also reported using other substances, such as tobacco and marijuana.
Recent reports indicate a slight shift in alcohol use during pregnancy:
- A 2021 CDC report found that 14% of pregnant women reported drinking during pregnancy, with 5% admitting to binge drinking.
- Between 2018 and 2020, 13.5% of pregnant women reported current drinking, and 5.2% reported binge drinking in the past 30 days.
This marks a slight increase from previous years and highlights the ongoing challenge of alcohol and substance abuse during pregnancy. The 2018-2020 period also highlighted that pregnant women without a regular healthcare provider and those experiencing frequent mental distress were more likely to report alcohol use.
- Pregnant women experiencing frequent mental distress were 2.3 times more likely to report current alcohol consumption and 3.4 times more likely to engage in binge drinking compared to those without mental distress.
- Expectant mother’s women without a regular healthcare provider were 1.7 times more likely to report current alcohol use compared to those with consistent access to healthcare.
These statistics underscore the ongoing challenges of increasing access to prenatal care and resources for substance abuse treatment that can help prevent fetal alcohol spectrum disorders. Additionally, healthcare providers must be proactive in screening for alcohol use, offering nonjudgmental support, and connecting expectant mothers with resources for mental health care.
Who Can Be Held Liable for Birth Injuries When Risk Factors Are Ignored?
Birth injuries can lead to severe health issues, disabilities, and even death in infants. While some arise from natural complications, many result from the negligence and errors of medical professionals during labor and delivery. When a child and their family have been affected by sub-standard medical care, pursuing a birth injury malpractice lawsuit against any party whose negligence contributed to a baby, or mother's injuries can help them recover the compensation they need and deserve.

Common examples of those who may be held accountable for birth injuries include (but are not limited to):
- Obstetricians (OB-GYN)
- Other obstetric professionals
- Surgeons
- Pediatricians, including pediatric neurologists
- Anesthesiologists
- Labor and delivery nurses
- Midwives
- Nurses
- Hospitals and medical facilities
- Hospital administrators
- Other hospital staff
- Neonatal intensive care nurses and aids
- Neonatologists or pediatricians providing neonatal care
- Respiratory therapists
- Maternal-fetal medicine physicians and specialists (MFM)
- Laboratory staff
Hospitals may also be held vicariously liable for injuries or harm a patient suffers due to the negligent actions and omissions of an employee acting within the scope of their employment. It is also possible for a hospital to be held directly liable for its own negligence. For example, a hospital may be held directly liable if they fail to establish proper patient safety protocols or violate patient confidentiality by mishandling patient records. Seeking the guidance of a birth injury attorney is the best way to ensure all avenues for compensation are explored and effectively pursued.
Types of Legal Damages in a Birth Injury Lawsuit
If you suspect that medical negligence contributed to your child's birth injuries, taking prompt legal action is essential to securing the compensation needed for your child's medical expenses and ongoing care. In a birth injury lawsuit, damages can be divided into two main categories: economic and non-economic.

Economic Damages are quantifiable financial losses that directly result from the birth injury. These damages can be calculated based on the cost of actual losses and/or projected future expenses. Some examples of these damages include:
- Medical bills and life care expenses (including the cost of any future medical care)
- Rehabilitation and therapy costs (occupational, physical, speech, behavioral, and cognitive)
- The cost of attendant and home health care
- Parents loss of income or wages due to caring for their child if they are unable to or must take time off work (including future loss of income)
- The cost of medication
- The cost of adaptive equipment and technology (hearing aids, specialized keyboards, and wheelchairs)
- Lost future earning capacity (if the child's birth injury impacts the child's ability to work in the future)
- The cost of special education and tutors
- Home and vehicle modification costs (such as ramps or accessible bathrooms)
- The cost of surgery or other specialized treatment
- The cost of diagnostic testing
Non-economic damages address the intangible losses that often have a tremendous impact on the victim's well-being and quality of life.
Here are some examples of these damages
- Pain and suffering
- Diminished quality of life
- Disability and Physical Impairment
- Disfigurement and permanent scarring
- Mental Anguish
- Anxiety, depression, or post-traumatic stress disorder (PTSD)
- Loss of consortium
Punitive or exemplary damages may be awarded in cases where the actions of the at-fault party demonstrate gross negligence, recklessness, intent, or malice. These damages aim to hold the negligent healthcare provider accountable for their extreme carelessness and discourage others from committing similar acts.
Several factors are considered in determining the potential settlement award you may receive, these include the severity of your child's birth injury, the extent of your economic losses, and the long-term impact of the injury on your child's quality of life. A qualified birth injury malpractice attorney will thoroughly investigate your case to determine the type and amount of damages that may be available in your case.
Statute of Limitations in a Birth Injury Lawsuit
Statutes of limitations (SOL) are established by law in each state and dictate the timeframe within which a personal injury lawsuit must be initiated. Typically, the countdown begins on the date of the injury. However, the discovery rule provides an exception to this rule in cases where the injury was not immediately apparent. Under this rule, the clock doesn't start ticking until the injured person discovers or reasonably should have discovered their injury. This can be confusing, so it's advisable to contact a knowledgeable birth injury attorney to discuss your and your child's legal rights and options.
According to Chapter 74 of the Texas Civil Practices & Remedies Code, there are several deadlines for filing a birth injury case in the state.
These include:
- For damages (other than medical expenses) incurred until age 18, a lawsuit must be filed by the time the child turns 14.
- To recover medical expenses for the child from birth until age 18, the lawsuit must be filed within two years of the date of the accident.
If the statute of limitations expires in your case, you may lose the opportunity to seek compensation. A medical malpractice lawyer can determine the specific deadlines that apply to your unique situation and ensure paperwork is filed on time.
How Can Our Birth Injury Lawyers Can Help?

If your child has been affected by fetal alcohol syndrome related birth injury, it's essential to have a trusted advocate on your side. At Miller Weisbrod Olesky, our knowledgeable and compassionate birth injury attorneys are committed to working tirelessly to hold those responsible accountable for the harm caused.
We have successfully helped countless families obtain the compensation they need to cover the cost of their child's care and ensure they have access to necessary treatments, therapies, and support for their future.
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.