Birth Injury Risk Factors
Risk Factors Leading to Birth Injuries
From early pregnancy to the delivery room, medical professionals are responsible for closely monitoring the mother’s and baby’s health.

Every parent hopes for their child to be safe, healthy, and happy at birth. But the reality is not every birth goes according to plan.
Complications during pregnancy or during delivery can put the baby’s safety at risk. In the worst cases, this risk results in a serious birth injury.
Birth injuries like brain damage at birth have the potential to permanently affect the rest of the newborn’s life. Due to the high stakes, medical professionals must take every precaution to prevent the mother or baby from experiencing harm.
This involves conducting various screenings, diagnostic tests, and routine prenatal check-ups to manage conditions and identify potential risks. Unfortunately, even the most experienced doctors and nurses may overlook early signs of birth complications. This oversight can lead to devastating injuries that leave families facing a lifetime of questions, concerns, and expensive medical care.
Those responsible for these preventable injuries often refuse to take accountability, especially in cases involving severe complications during pregnancy. But an experienced birth injury attorney can help uncover the evidence that links a child’s birth injuries to medical malpractice.
Birth Injury Malpractice Attorneys
Our birth injury lawyers help families seek justice and compensation for preventable injuries to mothers or their babies during childbirth. If you or your baby suffered preventable harm from mismanaged birth injury risk factors, don’t hesitate to contact our firm. We can answer difficult legal and medical questions and investigate the facts on your behalf.
Free Legal Consultation
Birth Injury Lawyers
(888) 987-0005Our Birth Injury Lawyers are available to meet you in your home or the hospital.
Our vast network of medical experts and in-house nursing staff and nurse-attorneys gives us the edge over our competition. When we take your case, we assign you with not just an attorney but an entire medical team. This team includes attorneys, experienced nursing advocates, and seasoned medical experts.
Your team is available to assist with any day-to-day treatment you or your child may need. This includes assistance with obtaining medical records, scheduling doctors’ appointments, providing transportation, and any other problems that may arise.
We offer all of this on a contingency fee basis. This means you will not pay any fees until after we win your case and secure a settlement. Our firm’s unmatched track record of birth injury results sets us apart from other birth injury law firms.

Recent Birth Injury Settlement:
Birth Injury settlement against a hospital in which nurses and physicians failed to properly monitor the mother's blood pressure during delivery causing an HIE event resulting in neonatal seizures and cerebral palsy at birth. Our team of top-rated birth injury lawyers recovered $13,750,000 for the family to help with future medical expenses and developmental therapy.
What is a Birth Injury?
Birth injuries are any physical harm a mother or otherwise healthy infant suffers before, during, or after delivery.

Some birth injuries are minor and often heal on their own in a few days or weeks. However, other birth injuries can result in life-long disabilities that affect a child for the rest of their life.
Birth injuries are unlike birth defects, which are usually genetic abnormalities present at birth that often result from hereditary factors. Instead, birth injuries typically arise from preventable birth complications related to the delivery process or the newborn phase.
Healthcare providers have a duty to take proactive measures to address birth injury risks and complications. Overlooking warning signs can result in critical delays in intervention, leading to severe outcomes for both the mother and infant.
In such cases, a knowledgeable birth injury attorney can provide essential support. They can help gather medical records, consult with experts, and build a strong case to hold negligent healthcare providers accountable.
Types of Birth Injury Risks
Understanding the risk factors associated with birth injuries is essential for expectant mothers and healthcare professionals alike. These risk factors typically reveal themselves during proper medical evaluations throughout pregnancy, labor, and delivery.

Certain birth injury risk factors, like the mother's age or fetal presentation inside the womb, are out of a medical provider’s control. However, they must still consider these factors when making decisions about how to minimize the risk of injury.
What Are Maternal Birth Injury Risk Factors?

The likelihood of serious injury increases considerably when healthcare professionals fail to recognize and address these risk factors:
Maternal Obesity

Medical professionals classify an expecting mother as obese when her body mass index (BMI) reaches 30 or higher. Studies suggest that infants of morbidly obese mothers (BMI >40) have a notably higher risk for birth injuries.
Obesity can make it harder for the mother’s body to break down sugars and control blood pressure. This can cause pregnancy complications like gestational diabetes and preeclampsia, which can lead to numerous birth complications.
Mothers with a high BMI often experience a prolonged first stage of labor, increasing the likelihood of prolonged or arrested labor. Additionally, obese mothers who have had a previous C-section are less likely to achieve a successful vaginal birth after cesarean (VBAC).
Preeclampsia
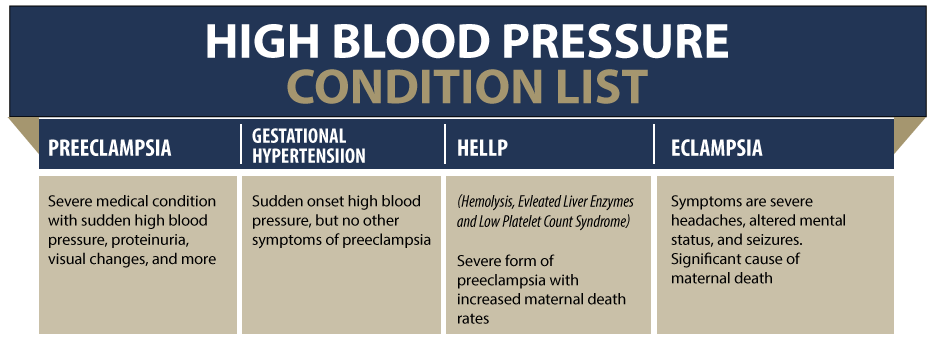
Preeclampsia is a serious pregnancy complication causing high blood pressure and high protein count in the mother’s urine. It usually occurs midway through pregnancy (around 20 weeks gestation).
High protein in the urine can indicate kidney or liver damage. This can put the mother at risk for organ failure and more severe hypertensive disorders like HELLP syndrome. It can also increase the baby’s risk for premature birth.
Additionally, maternal hypertension (high blood pressure) can affect blood flow in the placenta. A baby suffering from restricted blood flow to their brain (ischemia) is at risk for potentially severe brain injuries. These injuries can result in permanent conditions like cerebral palsy when medical professionals fail to intervene or identify the risk.
Gestational Diabetes

Gestational diabetes mellitus (GDM) occurs when the mother’s body develops resistance to insulin during pregnancy. This results in high blood sugar (glucose buildup), which can potentially affect the baby’s development.
A glucose surplus can increase the baby’s size to an unsafe level during pregnancy. This increases the risk for complications like macrosomia or cephalopelvic disproportion, which can make vaginal labor difficult or even impossible.
Babies larger in size are at a greater risk for birth injuries like bone fractures, shoulder dystocia, and brachial plexus injuries. These injuries are more likely when medical professionals fail to address a mother’s gestational diabetes through medication or nutrition changes.
HELLP Syndrome
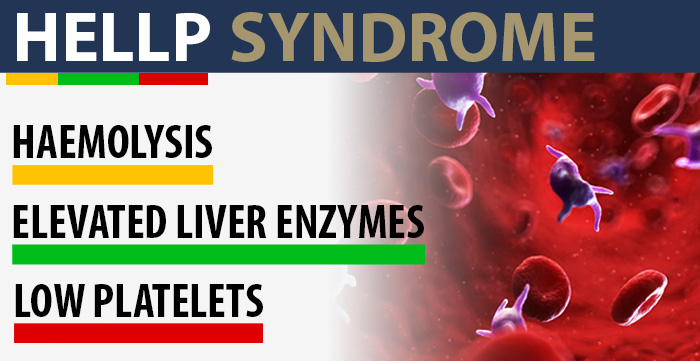
HELLP syndrome stands for hemolysis (red blood cell destruction), elevated liver enzymes (liver damage), and low platelets (affecting blood clots). The condition is a medical emergency that normally occurs during the third trimester or shortly after childbirth.
Research links HELLP syndrome with blood clotting disorders like disseminated intravascular coagulation (DIC). This is a condition that causes many “micro” blood clots throughout the body, including the placenta. Studies suggest that HELLP syndrome is a risk factor in causing DIC-induced placental abruptions, which can severely injure the baby.
Blood Clots During Pregnancy

Changes in hormone production during pregnancy can increase blood clotting. Large clots can pose a risk to the mother and her baby by obstructing placenta blood flow. Low blood flow can cause intrauterine growth restriction and other more serious complications like hypoxia and ischemia.
Additionally, large blood clots can put the mother’s life at risk. If a piece of the clot breaks off into the mother’s bloodstream, it can reach its way to her lungs. This can cause a pulmonary embolism, which is a life-threatening medical emergency putting both the mother and baby at risk.
About Blood Clots During Pregnancy
Maternal Infections

A mother can transmit maternal infections to her baby via the placenta during pregnancy or the birth canal during delivery. Common bacterial and viral infections include chorioamnionitis, group B Streptococcus (GBS), hepatitis B, and rubella.
Even though they may cause only mild symptoms in the mother, these infections can lead to severe complications for the baby. Group B strep is a particularly concerning bacterial infection as it can lead to sepsis, pneumonia, or meningitis.
The presence of maternal infections can have a negative effect on the fetal and placental membranes. Infections in pregnancy also complicate the delivery process by triggering a fever in the mother, which disrupts fetal oxygen supply. These disruptions can deprive the baby of essential oxygen, which may result in severe brain injuries like HIE.
Medication Misuse

A mother may receive medications for many different reasons. She might receive antibiotics to treat an infection, regional anesthesia during labor, or even medications to induce labor.
Incorrect dosages of antibiotics or antiviral medications during pregnancy can increase the risk of birth defects. Also, an overdosage of labor inducing medications like Pitocin or Cytotec can cause unsafe labor contractions. These forceful contractions can restrict oxygen flow past the point of safety, increasing the baby’s risk for brain damage.
Birth Injuries From Medications
Cholestasis of Pregnancy

Intrahepatic cholestasis of pregnancy (ICP) is a liver condition resulting from the buildup of bile acids (fluids that aid digestion). It can cause unbearable itching and discomfort for the mother.
When the buildup of bile acids crosses the placenta, it can make the uterus more sensitive to oxytocin. High sensitivity to oxytocin can induce premature labor contractions, increasing the baby’s risk of preterm birth. Babies born too early carry a high risk for birth injuries and complications.
Amniotic Fluid Complications

Before birth, a sac of amniotic fluid surrounds the baby. This protective liquid regulates the baby’s temperature, allows for fetal movement, and guides organ development. A mother’s “water” breaks when the amniotic sac ruptures, typically indicating the start of labor.
Different amniotic fluid complications can increase a child’s risk for injuries at birth. Complications with the amniotic fluid can include:
Polyhydramnios

Polyhydramnios is a condition where the baby has an excess amount of amniotic fluid surrounding them. Too much amniotic fluid can contribute to premature birth due to the overly stretched uterus triggering labor contractions.
Polyhydramnios also often leads to increased fetal movement, increasing the risk of an abnormal delivery position. Abnormal positions like breech position or shoulder position can complicate birth and necessitate an emergency C-section.
Oligohydramnios

Oligohydramnios is a condition where the baby has too little amniotic fluid surrounding them. It can be a sign of underlying issues like placental insufficiency or a premature rupture of membranes.
Oligohydramnios can contribute to a baby’s underdeveloped organ systems, specifically to their respiratory development. Babies with underdeveloped lungs can suffer from respiratory distress syndrome and require supplemental oxygen at birth.
Premature Rupture of Membranes

Premature rupture of membranes (PROM) occurs when the mother’s amniotic sac ruptures before labor begins. It typically happens late into the third trimester and can be a symptom of post term pregnancy.
PROM can trigger premature birth and increase the chance for amniotic fluid infections like chorioamnionitis.
Placental Complications

During pregnancy, placental complications present serious risks to both the mother and her baby. Among the most concerning are placenta previa, placental abruption, and placental insufficiency.
Placenta Previa

Placenta previa describes a placenta moving toward the bottom of the womb, either fully or partially covering the cervix. A placenta is “low-lying” if it’s within 2 centimeters from the cervix.
A placenta's low position in the uterus can block the baby's passage through the birth canal. This can delay delivery and result in oxygen deprivation (indicated by fetal distress on the electronic heart rate monitor).
Science has also linked placenta previa with certain birth complications. According to researchers, placenta previa is the single most common placenta-related cause of anemia in infants.
Placental Abruption
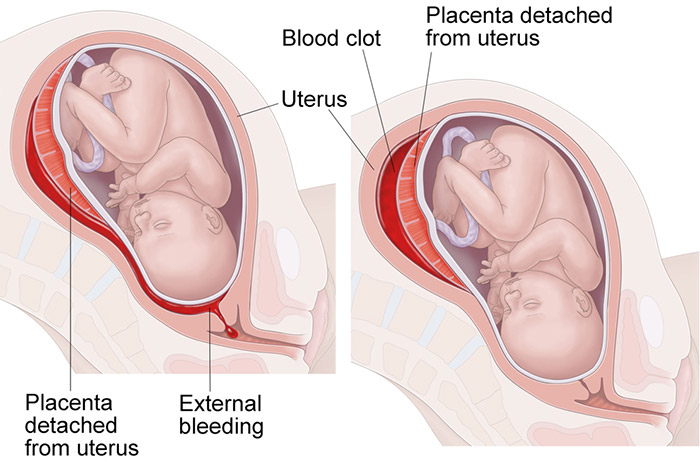
Placental abruption is another severe complication where the placenta prematurely detaches from the uterine wall. This can lead to intense abdominal pain, vaginal bleeding, and frequent contractions.
For the mother, placental abruption can cause significant blood loss and postpartum hemorrhaging. This raises her risk of multi-organ failure, infection, or even cardiac arrest without immediate intervention. Postpartum hemorrhage is one of the leading causes of maternal mortality in the world.
For the baby, the premature detachment can quickly disrupt the supply of oxygen and nutrients. This increases the likelihood for birth complications like fetal distress, premature birth, and even stillbirth.
Placental Insufficiency

Placental insufficiency happens when the placenta cannot deliver sufficient blood, oxygen, and nutrients to the fetus. This insufficiency can stem from maternal health issues like high blood pressure, diabetes, blood clotting disorders, or other pregnancy complications.
When the placenta fails to adequately supply nutrients to the fetus, it can restrict their growth and lead to complications. Risks can include preterm birth, intrauterine growth restriction, low birth weights, and developmental delays.
Early detection of placental complications is essential to managing risks effectively.
Medical professionals must conduct thorough prenatal testing to check for issues with the mother’s placenta. This may include ultrasounds to monitor placental position/functioning as well as blood tests to assess any potential abnormalities.
Incompetent Cervix
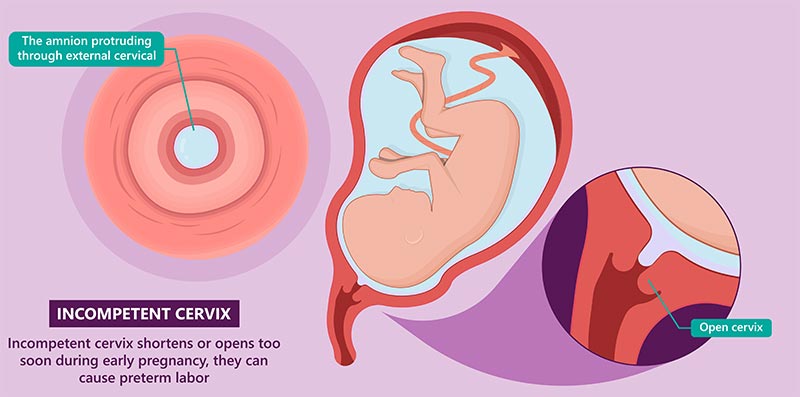
Cervical insufficiency occurs when the mother’s cervix softens and/or opens too early in pregnancy.
The cervix typically remains firm and closed until labor begins. During labor, it thins out (effaces) and opens (dilates) to allow the baby to exit out through the birth canal.
If the mother’s cervix effaces and dilates too soon during pregnancy, it increases the risk of premature birth. A baby’s preterm birth exposes them to injuries and complications like respiratory distress syndrome, low birth weight, and underdeveloped brains.
Twin Labor

Carrying twins comes with elevated risks for pregnancy complications and birth injuries. Research indicates that around 60% of twins have premature births. Twins in the womb also carry a higher risk for intrauterine growth restriction (IUGR).
Injuries and complications are quite common during twin labor. A long interval after the first baby’s delivery can cause issues for the second twin. High inter-delivery time gaps will lead to a progressive decrease in the umbilical cord pH level. This increases the second twin’s risk for fetal acidosis and hypoxia shortly before delivery.
Additionally, the mother faces up to a 25% chance of experiencing postpartum hemorrhage after a twin delivery.
About Twin Birth Complications
Precipitous Labor

Doctors classify a mother’s labor as “precipitous” or “rapid” when she delivers in under 3 hours of her water breaking. The speed and intensity of a mother’s precipitous labor contractions can damage the uterine lining and cause internal bleeding. It also increases her risk for a uterine rupture.
Additionally, the baby faces a higher risk of birth trauma from their rapid progression through the birth canal.
Prolonged and Arrested Labor

Labor lasting between 18 and 24 hours is a leading cause of birth injuries. Most medical standards state any labor that exceeds this time period requires an emergency C-section to prevent prolonged fetal distress.
Prolonged labor contractions will threaten the baby’s oxygen supply. If the child experiences restricted oxygenation, they become at risk for birth asphyxia and subsequent fetal hypoxia and anoxia. Oxygen deprivation can cause irreversible brain damage at birth that permanently affects a child’s physical capabilities.
Labor Inducing Medications

In cases of a prolonged labor or post term pregnancy, doctors may opt to administer labor inducing medications. Medications like Pitocin and Cytotec can strengthen weak uterine contractions or soften a particularly stubborn cervix.
However, these medications can sometimes induce labor contractions that are too frequent and too forceful, known as uterine hyperstimulation. Harmful contractions from hyperstimulation can press too hard on a baby, limiting their oxygen supply. Babies with reduced oxygenation are at risk for fetal distress and related brain injuries like hypoxic ischemic encephalopathy.
Uterine Hyperstimulation

Uterine hyperstimulation refers to labor contractions that are too forceful. Signs of hyperstimulation include five or more contractions within 10 minutes, contractions lasting over 2 minutes, and fetal distress signals.
Extreme contractions can cause pain and internal hemorrhaging for the mother. In severe cases, they may even cause a uterine rupture.
For the baby, intense contractions can cut off their oxygen supply. This increases their risk of developing birth asphyxia, hypoxia, anoxia, and brain damage at birth from oxygen deprivation.
About Uterine Hyperstimulation
Post Term Pregnancy

Post term pregnancy refers to a labor that continues after 42 weeks gestation. It presents risks to the baby because the placenta becomes weaker at supplying oxygen and nutrients after 40 weeks.
A post term baby also has higher risks for growing too large (fetal macrosomia), which can complicate vaginal birth. They also have a higher likelihood of passing their first stool (called meconium) while still in the womb. If the baby attempts to breathe in, the meconium-stained amniotic fluid can enter their lungs.
Research shows that the risk of meconium aspiration syndrome (MAS) increases with gestational age.
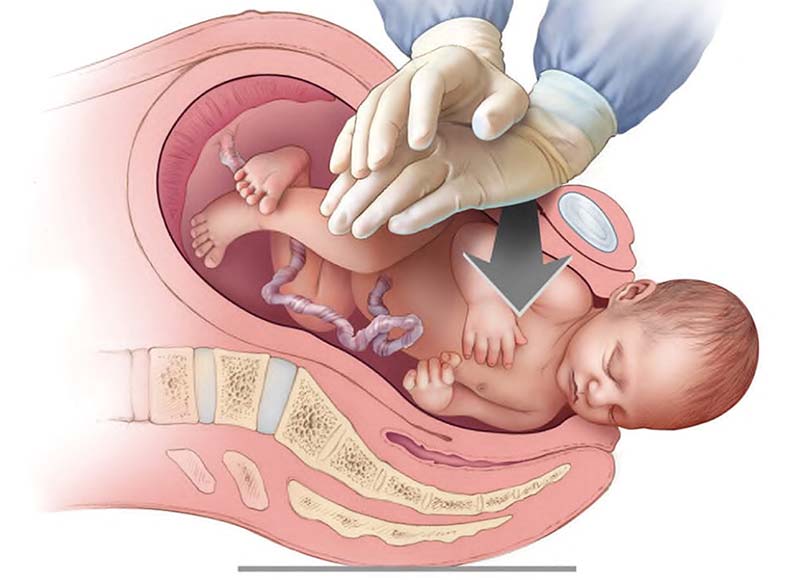
C-section

A Cesarean section (C-section) procedure involves surgeons cutting into the mother’s abdomen to deliver the baby. In 2023, doctors delivered nearly one third of live births via C-section in the United States.
A C-section presents multiple risks to both the mother and her baby. Recovering from the abdominal incision can take multiple months, and the site is prone to scarring and infection.
Typically, babies delivered via emergency C-section already carry a high risk for birth injuries. This may be because they’re in an abnormal fetal position or have a non-reassuring heart rate.
Delaying a C-section for too long can prolong their oxygen deprivation and result in hypoxic brain injuries at birth.
Vaginal Birth After C-section (VBAC)

Attempting a vaginal birth after a prior C-section can be dangerous and pose a risk for birth injuries. The primary concern is with the mother ripping her previous C-section scar, which can cause hemorrhaging and fetal oxygen deprivation.
Doctors will generally advise against attempting a vaginal birth after C-section (VBAC) for mothers with recent C-sections or uterine scarring. A potential uterine rupture can put both hers and her child’s life at risk.
Use of Delivery Instruments

For some difficult deliveries, doctors may use instruments like forceps and vacuum extractors to get the baby out.
These tools can save a baby with oxygen deprivation who is stuck inside the birth canal. However, delivery instruments pose a risk for serious birth injuries when medical professionals use excessive force.
Excessive force with a vacuum extractor on the baby’s head can expose them to potential skull fractures and intracranial hemorrhages. Brain damage from bleeding can impair critical motor function and result in a cerebral palsy diagnosis later in childhood.
Fetal Risk Factors

The following fetal risk factors can greatly increase the likelihood of a baby’s injury at birth:
Premature Birth

Premature birth is one of the largest risks for birth injuries. A baby born before their scheduled due date can:
- Have underdeveloped lungs, increasing the risk for respiratory distress syndrome (RDS)
- Have a weak immune system, making them vulnerable to neonatal infections
- Have heart problems like fetal bradycardia (slow heartbeat)
- Have a low birth weight
- Be more susceptible to bone fractures during birth
- Experience issues with temperature regulation
- Require an extended stay in the neonatal intensive care unit (NICU)
- Have a 30%-55% higher likelihood for developing cerebral palsy
Healthcare providers do not always know what causes premature birth. However, they can monitor high-risk pregnancies for risk factors such as preeclampsia, placental complications, and twin pregnancy.
Fetal Macrosomia

Macrosomia is a condition where a baby grows excessively large for its gestational age. Doctors classify any baby weighing more than 8 pounds, 13 ounces as macrosomic.
If the baby is excessively large, the likelihood of injury during vaginal delivery significantly increases.
Macrosomic babies experience a higher incidence rate for shoulder dystocia when travelling through the birth canal. They also have a higher likelihood of cephalohematoma, which is bleeding that occurs between the baby's skull and bone membranes.
Cephalopelvic Disproportion (CPD)

Cephalopelvic disproportion (CPD) is a complication related to a mismatch in fetal head size and maternal pelvic shape. It occurs when the baby’s head is too large or when the mother's pelvis is too small for safe vaginal delivery.
This mismatch can lead to prolonged time in the birth canal, increasing the risk of complications like oxygen deprivation. Like with macrosomia, shoulder dystocia is also a serious risk associated with CPD.
CPD often forces medical professionals to use riskier delivery methods, including using forceps and vacuum extractors or performing a C-section. These methods can increase the likelihood of the baby experiencing a birth injury.
Shoulder Dystocia
Shoulder dystocia occurs when the baby's head emerges from labor, but the shoulders remain lodged behind the pelvic bone.
Prolonged entrapment in the birth canal can cause the baby to suffer from oxygen deprivation or even brain damage. These complications can lead to severe birth injuries, including cognitive impairments, developmental delays, and physical disabilities.
In some cases of difficult deliveries, medical professionals may utilize assistive devices like vacuum extractors or forceps. However, improper application of these tools can put the baby at risk of brain injury, head trauma, or nerve damage.
Abnormal Delivery Position
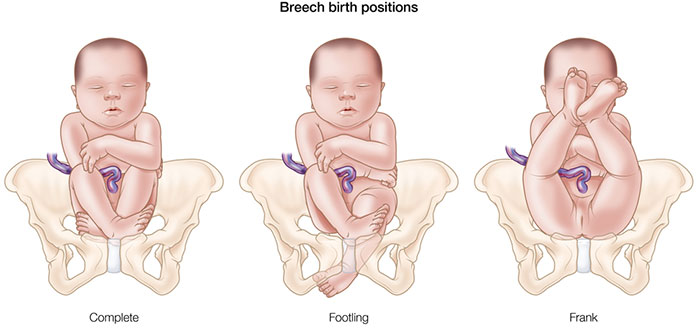
An abnormal fetal position before delivery can complicate vaginal delivery and increase the risk of a birth injury.
Most babies present headfirst, known as cephalic presentation. Abnormal presentation positions may include breech, face, brow, breach, and shoulder.
In breech or face-first presentations, doctors may use obstetrical tools like forceps or vacuum extractors to assist in delivery. However, improper usage of these tools can raise the risk of physical trauma, bone fractures, or brachial plexus injuries.
The risks associated with abnormal delivery positions can also impact the mother during childbirth. An abnormal fetal position can prolong labor and increase the risk of postpartum hemorrhage, severe vaginal tearing, and perineal lacerations.
Umbilical Cord Complications

The umbilical cord, a tube attaching from the baby's stomach to the placenta, acts as a lifeline throughout pregnancy. It plays a crucial role in supporting the baby's growth and development by delivering essential oxygen while removing waste products. Any disruption in the umbilical cord's function can deprive the baby of vital resources necessary for healthy growth and development.
The most common umbilical cord issues that can interfere with a baby's health are umbilical cord compression and nuchal cord.
Nuchal Cord

A nuchal cord describes a complication where the umbilical cord wraps around the baby’s neck. It can become more common with cases of long cords or polyhydramnios because the baby moves around more than usual.
The biggest concern is that the nuchal cord will restrict the baby’s access to oxygenated blood. If the cord is tight enough, this cutoff can result in brain injuries like hypoxic ischemic encephalopathy upon birth.
Umbilical Cord Compression

Umbilical cord compression is a condition that occurs when the baby’s weight squeezes the umbilical cord during labor. This can compromise blood flow and deprive the baby of necessary oxygen and nutrients needed for healthy development.
Oxygen deprivation from umbilical cord compression can lead to serious conditions such as hypoxic ischemic encephalopathy or cerebral palsy.
Umbilical Cord Prolapse

Umbilical cord prolapse happens when the cord moves down the birth canal before or alongside the baby. Ideally, the cord should exit the birth canal after the baby.
If the cord precedes the baby or moves alongside it, it can create a dangerous blockage of oxygen. The blockage may result in birth asphyxia, hypoxic ischemic encephalopathy, and other birth injuries.
Vasa Previa
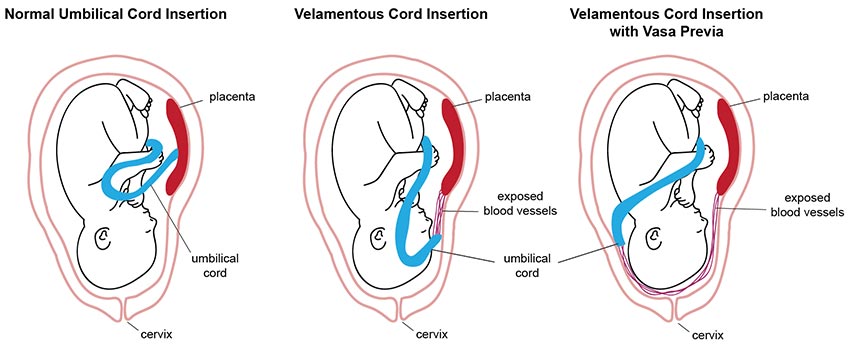
Vasa previa is a condition where exposed umbilical cord vessels cover the opening of the cervix. This is problematic because the vessels will rupture if the baby attempts vaginal delivery, resulting in major fetal blood loss.
Ruptured umbilical cord vessels from uncaught vasa previa significantly increase the risk of stillbirth from hemorrhaging.
When umbilical cord complications disrupt this flow of nutrients, it puts the baby at risk for developing serious birth complications. Healthcare professionals must watch for these risk factors during prenatal testing visits and respond accordingly to prevent later harm.
Improper Fetal Heart Rate Monitoring

A baby’s heart rate before birth can tell healthcare providers how they are responding to conditions within the womb. For example, fetal bradycardia (heart rate <110 bpm) can suggest the baby is suffering from oxygen deprivation.
Other factors of a baby’s heart rate (such as the baseline, variability, or decelerations) can also reveal vital information. When medical professionals fail to conduct attentive fetal heart rate monitoring, they may miss signs of fetal distress. This increases the baby’s risk of dangerous injuries like hypoxia, ischemia, and brain damage at birth.
What Are Common Birth Injuries from Medical Malpractice?

Physicians and other healthcare professionals receive extensive education and training to respond effectively in emergencies during childbirth. Despite this, numerous birth injuries still arise from their mistakes or negligence during labor and delivery.
Some of the most common examples include:
Perinatal Asphyxia

Oxygen deprivation is often the first step in causing a child’s brain damage at birth. Brain cells begin to die off within minutes of birth asphyxia, resulting in permanent dysfunction and impairment.
Common risk factors for fetal oxygen deprivation include:
- Placental complications
- Umbilical cord problems
- Preeclampsia
- Blood clots during pregnancy
- Prolonged labor
- Uterine hyperstimulation
- Size abnormalities like macrosomia
- Maternal infections
- Shoulder dystocia
Perinatal asphyxia can lead to preventable brain injuries, gross motor function impairment, and delayed developmental milestones. Healthcare professionals can conduct careful fetal heart rate monitoring during labor to prevent or minimize the effects of these outcomes.
Hypoxic ischemic Encephalopathy (HIE)
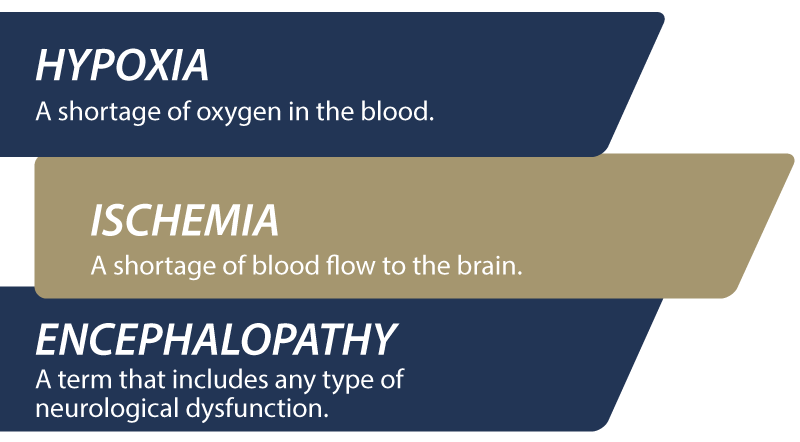
Hypoxic ischemic encephalopathy is one of the more severe types of brain injuries. It stems from a lack of oxygen and blood flow to the brain during labor and delivery.
HIE affects approximately 1.5 to 2.5 per 1,000 live births in developed countries. Of babies diagnosed with moderate to severe HIE, up to 40% may not survive infancy.
Several known risk factors may contribute to the development of HIE. These include:
- Insufficient blood flow to the placenta
- Preeclampsia
- Neonatal infections
- Placental previa or a placental abruption
- Umbilical cord problems like nuchal cord, compression, or prolapse
- Uterine rupture
- Fetal distress
- Respiratory distress syndrome
HIE’s severity and long-term consequences often depend on how long the baby goes without oxygen or blood flow. Some children who experience HIE may experience mild to moderate symptoms, while others face severe disabilities.
Cerebral Palsy

Cerebral palsy (CP) is a group of neurological disorders that affect a person’s ability to move. These disorders are often result from a brain injury occurring shortly before or during birth.
There is no cure for cerebral palsy. It is not a progressive disorder, but symptoms and impairments may change or worsen over time. Children with cerebral palsy will require regular medical care, ongoing therapy, specialized educational support, and adaptive equipment to manage symptoms.
Spinal Cord Injuries

Each year, approximately 17,500 individuals experience a spinal cord injury in the United States. However, only about 5% of these cases involve children.
Spinal cord injuries can disrupt the essential nerve connections between the brain and the rest of the body. Such disruptions can lead to severe injuries that may have lasting effects on the child's health and development.
The severity of spinal cord injuries can vary significantly, from mild bruising to severe, long-term disabilities requiring extensive medical intervention. Early intervention is essential to minimizing potential long-term complications.
Did Doctors Ignore My Child’s Birth Injury Risk Factors?

When a child suffers harm during childbirth, it can have devastating and lasting effects on both them and their family. Our firm can help hold negligent healthcare professionals accountable and successfully file a birth injury medical malpractice claim. Your lawyer will need to prove that their failure to uphold the standard of care directly contributed to the injury.
If you believe medical malpractice harmed you or your baby, contact one of our birth injury attorneys. We can help you determine the strength of your case and explain your legal rights and options.
Families who have experienced the effects of birth injuries from negligent medical care deserve to know whether they were avoidable. Our top rated birth injury lawyers help you seek justice and compensation for preventable injuries by proving medical negligence occurred. We handle medical malpractice cases involving birth injuries to babies and for mothers injured from mismanaged pregnancy complications.
What is the Statute of Limitations in a Birth Injury Case?
A Statutes of limitations (SOL) is a law that sets a time limit on how long an injured person has to file a lawsuit after an accident.
It is essential to understand that statutes of limitations vary based on the case and the state where you file. For instance, the deadline for birth injury claims is typically different from other claims, such as injury to private property.
Generally, the clock starts ticking on the date the injury occurred. However, there are exceptions to this rule. In some cases, the statute of limitations starts when a person discovers or reasonably should have discovered an injury. When dealing with government agencies, SOLs can become even more complex.
For example, if the party that injured you was:
- A federal employee
- Employed by a military hospital, Veterans Administration facility, or a federally funded medical entity
You may need to file a birth injury claim under the Federal Tort Claims Act (FTCA). In FTCA cases, claimants must go through certain administrative procedures before filing a lawsuit. In some states, you may have less time to give notice if:
- The negligent party was a local or state government hospital
- The doctors and medical providers are employees of a governmental entity
If you file your case outside of the statute of limitations, the court will typically dismiss it. This means you will not be eligible to recover compensation for you or your child’s injuries.
Determining when a statute of limitations begins on your case can be tricky. Our birth injury lawyers can help inform you of all the important filing cutoff dates in your state. We will help your family seek justice and compensation for preventable injuries to you or your baby.
How Can Our Birth Injury Lawyers Can Help?

Medical malpractice is responsible for thousands of birth injuries each year, impacting the lives of countless families. However, it takes an expert review of the facts of your birth to determine whether medical professionals made preventable errors.
Our Process
Our team of committed attorneys, nurses and paraprofessionals works to answer these questions and seek compensation. We use our detailed medical negligence case review process to assess your potential birth injury case.
We start by learning more about your pregnancy by gathering records to determine what happened before and during your delivery. This includes evaluating prenatal testing procedures and any preventative action taken to address pregnancy complications.
We will call in skilled medical experts who review your records and provide insight into where medical professionals went wrong. If we feel medical negligence caused your baby’s birth injuries, we contact you to discuss further. We will help your family seek justice and compensation for preventable injuries by proving medical negligence occurred.
At no point in our legal intake process will we ask you to pay anything. The medical review of your case and the consultation are free. We only receive payment once you do. The sooner you reach out, the sooner we can investigate your case and gather the evidence to support your claim.
We work on a contingency fee basis, meaning you will not pay any legal fees until we win your case. We do not purse any medical malpractice cases unless we fully believe we can win.
Contact us today to schedule your free consultation by calling our toll-free line at (888) 987-0005. You can also reach us by filling out our online request form.
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.