Labor Complications With Twins
Risks of a Twin Pregnancy for Mother and Babies
Nearly 3% of all live births in the US are twin births. Some twin pregnancies occur without any known cause, while others involve specific factors, such as older maternal age, hormonal changes, or use of in-vitro fertilization (IVF) and other assistive reproductive techniques.
The labor and delivery of twins involves a much higher risks of birth injury and birth complications including hypoxic ischemic encephalopathy (HIE). HIE is a brain injury pattern caused by a lack of oxygen flowing to the baby’s brain. HIE is the leading cause of cerebral palsy.
Because twin pregnancy and deliveries carry much higher risks, monitoring and prenatal testing during the pregnancy are keys to prevent well-known birth complications. Medical providers should perform regular ultrasound tests, fetal heart rate monitoring and be prepared for an emergency cesarean section where needed. The risks and complications can vary for monozygotic (identical twins) and dizygotic (fraternal twins). Therefore, the obstetric care plan should be developed according the unique risks associated with different twin gestations.
Many expectant mothers with twins are referred to obstetricians that specialize in high risk pregnancies called maternal fetal medicine (MFM) specialists. All twin pregnancies are considered high risk.

Known birth complications of twin pregnancies and deliveries include premature birth, premature rupture of membranes (PROM), intrauterine growth restriction (IUGR), placental abruption, gestational diabetes, preeclampsia, Twin to Twin transfusion syndrome (TTTS) and umbilical cord compression.
The most common complications include the following:
- Preterm labor and birth
Over 60 percent of twins and nearly all higher-order multiples are premature. - Gestational hypertension
Women with multiple fetuses are more than twice as likely to develop high blood pressure of pregnancy. - Anemia
Anemia is more than twice as common in multiple pregnancies. - Birth defects
Multiple birth babies have twice the risk of congenital abnormalities including neural tube defects, gastrointestinal, and heart abnormalities. - Miscarriage
Vanishing twin syndrome in which more than one fetus is diagnosed, but vanishes (or is miscarried) is more likely in multiple pregnancies. - Twin-to-twin transfusion syndrome
TTTS is a condition of the placenta that develops only with identical twins that share a placenta.
Types of Twins
Based on the number of placentas (chorionicity) and the number of amniotic sacs or inner membranes (amnionicity) surrounding the babies, the twin babies can be clinically defined.
Dichorionic Diamniotic Twins (DCDA)

In DCDA twin gestations, two amniotic sacs and two placentas are involved. About 75% of all twins are DCDA twins, where each baby has their own amniotic sac and own placenta. In recent decades, the incidence of DCDA twins has been rising because of the use of IVF and other assistive reproductive technologies as well as ovulatory drugs to treat fertility.
Monochorionic Twins
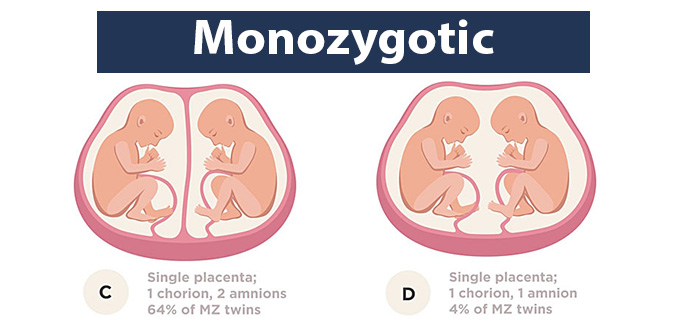
In monochorionic twin gestations, a single placenta is involved—meaning the twin babies share a placenta for oxygen and nutrients. Monochorionic twins constitute about 20 to 25% of twin pregnancies. Monochorionic twins are also known as monozygotic twins because they develop from the fertilization of one ovum. These twins share the same gender and same genetic background (identical twins).
About 99% of monochorionic twins are diamniotic (common placenta but separate amniotic sacs), and are known as monochorionic diamniotic (MCDA) twins. The remaining 1% share a single placenta and amniotic sac, and are therefore known as monochorionic monoamniotic (MCMA) twins.
Because monochorionic twins share the same placenta, they are at an increased risk of antenatal in-utero complications, such as Intra-Uterine Growth Retardation Syndrome (IUGR) and Twin-to-Twin transfusion syndrome (TTTS).
IUGR is a condition where the fetus does not grow as would be expected for the stage of pregnancy. In case of twins, the shared placental tissue may sometimes fail to bring sufficient nutrients to the developing babies, resulting in growth restriction. In case of TTTS, the shared placenta may cause blood flow imbalance, with one baby receiving excessive blood volume, while the other too little. This can cause serious heart complications.
About 15% of MCDA twins will develop severe TTTS, most likely between 16 and 24 weeks of gestation. Fetal growth restriction (IUGR) also affects more than half of MC (monochorionic) pregnancies with TTTS and about 15% of non-TTTS MC pregnancies.
Ultrasound Scans in Twin Gestation

The prenatal team of obstetricians, maternal fetal medicine specialists (MFM) and nurses should have experience in caring for expectant mothers having twins or triplets. Apart from the routine ultrasound monitoring, they should perform an ultrasound test between 11 and 14 weeks of gestation for an expectant mother with multiple pregnancy. This is the ideal time to determine which type of chorionicity and amnionicity (placenta and amniotic sacs) the twins have.
Another ultrasound scan between 18 and 20 weeks should be performed to determine whether the babies have developed an anomaly. In case of MCDA twins, more scans and regular fetal monitoring are necessary because these twins have a high risk of developing twin-to-twin transfusion syndrome (TTTS).
Ultrasound scans and fetal monitoring should also be more frequent in case of MCMA twins because these pregnancies carry a high risk of some form of umbilical cord entanglement is higher, which can create complications such as cord compression. While DCDA twins have a relatively lower risk of birth complications, but they should still be scanned every four weeks.
Biophysical profile (BPP), amniotic fluid tests, and nonstress tests (NST) should also be performed more frequently in case of twin gestations. The medical team should also document key features, such as the character of placental cord insert and the location of placental implantation.
When IUGR is detected during an ultrasound scan or the expectant mother is diagnosed with anemia, more intensive Doppler ultrasound tests should be performed for fetal monitoring. Doppler studies can evaluate the blood flow in the utero-placental vessels and the umbilical cord.
Time and Mode of Twin Delivery

To determine the appropriate delivery mode in a twin gestation, the doctors should consider a number of factors, such as gestational age, the first twin’s presentation, chorionicity, and fetal status (whether complications, such as IUGR or TTTS have been detected). A cesarean section delivery should be planned if there is a significant risk of complications during labor and delivery.
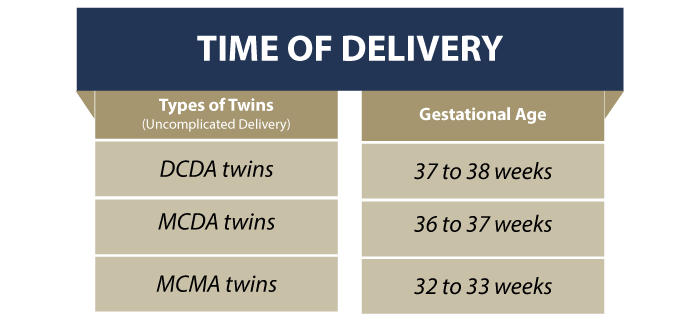
The National Institute for Health and Care Excellence (NICE) and the Royal College of Obstetricians and Gynecologists (RCOG) recommend an uncomplicated DCDA twins delivery between 37 and 38 weeks, and an uncomplicated MCDA twins delivery between 36 and 37 weeks.
Available evidence also indicates that a planned delivery at 36 weeks for uncomplicated MCDA twins and 37 weeks for uncomplicated DCDA twins can help lower the risk of stillbirth.
The medical team should make this decision in consultation with the expectant mother after carefully balancing the risks and benefits that are unique to the individual mother’s condition. For instance, a cephalic presentation baby (baby is head down, facing the spine) who is significantly smaller than the second twin could increase the risk of birth complications such as fetal distress and fetal hypoxia/fetal anoxia, and a planned cesarean delivery should usually be recommended.
In case of MCMA twins, a cesarean section delivery between 32 and 33 weeks of pregnancy is advised because of the high risk of umbilical cord entanglement and a catastrophic birth injury or even death. According to a research study, the incidence of cord entanglement in MCMA twins is as high as 72%. Retrospective studies show that in MCMA twin gestations, the risk of fetal death outweighs the risks of premature birth at 32 weeks’ pregnancy.

Are Trimesters Different With Twins?
First Trimester of Twin Labor
When an expectant mother with a twin gestation presents in labor, the medical team should be ready with appropriate preparations. A greater level of anesthetic, obstetric and neonatal expertise is usually required in twin delivery because of the higher risks of assisted delivery, prolonged or arrested labor, and PPH (postpartum hemorrhage or heavy bleeding after birth).
The medical provider should begin with a review of any fetal or maternal complications, and determine the first twin’s presentation. A bedside ultrasound scan is also recommended to determine the second twin’s presentation. Anesthesia team and a neonatologist should also be informed and necessary equipment should be prepared for the twin delivery.

Continuous fetal heart rate monitoring (CFHM) is critical t at this stage. Care should be taken to ensure that both babies are monitored, rather than just one baby’s tracing being repeated twice. Labor augmentation with Oxytocin/Pitocin may be considered as per guidelines. Considering the postpartum hemorrhage risks, ample IV access is recommended for blood transfusion.
Second Trimester of Twin Labor (Delivery)
A key difference between a singleton and twin pregnancy is that both babies must be actively monitored. If the medical provider finds any fetal distress or birth complication concern such as fetal hypoxia in the second twin, they should be prepared to expedite the delivery of both babies. Even a small delay in delivery when the baby is oxygen deprived can cause hypoxic-ischemic encephalopathy (HIE), which may lead to cerebral palsy.
Twin vaginal delivery involves 3 stages: (a) first twin delivery; (b) inter-delivery time gap (the time between delivering the first twin and second twin); and (c) second twin delivery. The time interval after the first baby’s delivery poses a high risk of complications for the second twin. Increase in inter-delivery time gap will lead to a progressive decrease in the umbilical cord pH level—which is indicative of fetal hypoxia and metabolic acidosis (both leading causes of brain injury). Therefore, longer inter-delivery time gaps increase the risk of fetal hypoxia, HIE and eventually cerebral palsy.
During this high-risk intervening phase, continuous fetal heart rate monitoring of the second twin is critically important. The presence of medical team members with experience in twin deliveries helps in making prudent clinical judgments for timely management. Overuse or early use of Pitocin at this stage may cause a prolapsed umbilical cord, while under-use or late intervention, such as a cesarean or assisted delivery, may result in longer inter-delivery interval, depriving the second twin of oxygen.
In case of monochorionic twins, the medical provider must clamp and cut the umbilical cord immediately in order to lower the risk of TTTS (twin-to-twin transfusion syndrome) at birth. The use of separate clamps for each twin is recommended so that cords can be differentiated if paired blood specimens are required.
If fetal monitoring of the second twin does not show any signs of fetal hypoxia, the medical team may manage the delivery as planned with an infusion of Pitocin/Oxytocin to optimize contractions (if necessary). Assisted delivery intervention is indicated if there are any signs of fetal distress or the second twin delivery is delayed despite the mother’s pushing effort.
Third Trimester of Twin Labor
It is equally important to actively monitor and manage the third stage of labor in twin gestations because of the increased risk of hemorrhage. In twin deliveries, the incidence of postpartum hemorrhage is known to be as high as 25%. Active management at this stage involves Pitocin/ Oxytocin infusion, clamping and cutting of the umbilical cords, and controlled cord traction to enable early delivery of the placenta.
Planned C-Section for Twins Delivery
The obstetrician or maternal fetal medicine specialist in consultation with the expectant mother and her partner should make a decision regarding planned cesarean section for twins. In case of breech presentation of the presenting twin, an elective c-section should be recommended. But even when a vaginal delivery has been planned, there is about 40% chance that an emergency c-section may be required for a twin delivery.
This is because there are risks of fetal distress of one or both twins, labor dystocia, or maternal infection risks. Even when the first twin’s vaginal delivery is completed, there is a possibility that the second twin may have to be delivered by cesarean section. Studies have shown that this risk to be up to 7%.
When c-section delivery for twins is performed, it is a good medical practice to perform an ultrasound exam before the operation in order to determine the fetal lie (the relationship between the long axis of the baby with respect to the mother’s long axis). Whether the twin delivery is vaginal or cesarean, the risk of postpartum hemorrhage should be accounted for. There must be proper communication with the anesthesiologist, timely infusion of Oxytocin, and a fast decision to use brace sutures or IU balloons if necessary to control bleeding.
Benefits of a Scheduled Early Twin Delivery
An inherent advantage of a scheduled early twin delivery is that an experienced care team, medical equipment and appropriate treatments are ready to use immediately if needed. In a scheduled early delivery or even otherwise, twins may require medical intervention immediately on birth. These may include neonatal resuscitation, respiratory support, cardiovascular support, and blood transfusions.
Moreover, when premature birth of twins is planned, the medical provider can administer important drugs, such as magnesium sulfate and antenatal steroids in-utero to reduce the risk of brain damage and other birth injuries due to inadequate lung development. By preventing PROM (premature rupture of membranes) and SPROM (spontaneous preterm rupture of membranes) with a scheduled early delivery, it may be possible to reduce to the twin babies’ risks of maternal infections, such as sepsis and meningitis, which can lead to permanent brain damage or mortality.
Birthing twin babies or triplets increases the risks during pregnancy, labor, and delivery. The best outcomes can be expected when an inter-professional medical team of doctors and nurses with experience in multiple deliveries provides appropriate care during labor and delivery in a well-coordinated manner.
Is Your Child’s Birth Injury the Result of Medical Malpractice?
Parents whose children suffer from birth injuries or birth complications want and deserve answers as to cause of their child’s injury and whether mistakes by the doctors and nurses contributed to the injury.
- Were there signs of a birth injury during the pregnancy, labor, and delivery process, or presence of risk factors, which were either not recognized or properly treated?
- Did the medical team fail to order a series of tests to diagnose a suspected birth complication in a timely manner?
- Was the decision to perform a cesarean delivery delayed?
- During the labor and delivery, were there clear indications that their baby was suffering from fetal distress, but appropriate actions were not taken by the obstetrician or nurses?
- Did the neonatal resuscitation team delay in providing important breathing support after birth?
- Were serious neonatal conditions like hypoglycemia or jaundice missed or treated incorrectly?
- Should brain cooling (also called “hypothermia therapy”) have been offered to your baby, but the doctors and nurses failed to perform the appropriate tests or ignored the results of the tests?
The experienced birth injury lawyers at Miller Weisbrod Olesky, who have been through the legal battlefields before, will help you determine if mistakes of the medical providers caused a birth injury to your child, including Hypoxic-Ischemic Encephalopathy (HIE) or cerebral palsy. Our profound and proven birth injury attorneys have represented families all over the United States in their time of need after a birth injury. We use our experience and expertise to obtain you and your child a medical malpractice settlement that will help provide specialized medical therapy in order to maximize the quality of life and independence of your child throughout their life.
Sometimes families are reluctant to contact a medical malpractice lawyer. It’s also not uncommon for parents to feel overwhelmed by the responsibilities they encounter in caring for their injured child and worried that they will not be able to help out in a lawsuit involving their child’s birth injury. Our birth injury attorneys and nursing staff will address these hesitations and concerns, so you can focus on your child and maximizing their care.
Registered Nurses and Nurse-Attorneys Are a Vital Part of Our Birth Injury Team…and Yours

Most birth injury law firms will employ one or two nurses to assist the review of cases and medical research. But Miller Weisbrod Olesky offers an unmatched number of nurses and nurse-attorney employees support to both the birth injury attorneys and our clients.
Our team of registered nursing staff and nurse-attorneys bring a deep level of medical and personal insight to every client’s case. Our nursing team includes both an experienced labor and delivery nurse as well as an ICU nurse. Working closely with the rest of the team, they investigate the reasons behind a birth injury and how medical professionals breached their standard of care.
Why Should You Talk with the Knowledgeable Attorneys at Miller Weisbrod Olesky?

The only way to find out if you have a birth injury case is to talk to a lawyer experienced in birth injury lawsuits. It’s not uncommon that a birth related complication results in a preventable birth injury, including cerebral palsy, but it takes a detailed expert review by a birth injury attorney of the medical records from your child’s birth to determine if the birth injury was the result of medical malpractice.
At Miller Weisbrod Olesky, a team of committed lawyers, nurses and paralegals uses our detailed medical negligence case review process to assess your child’s potential birth injury case. We start by learning more about you and your child and the status of meeting/missing developmental milestones. Then we gather medical records to determine what happened before, during, and after your delivery. We call in skilled medical experts who review your records and let us know if they think medical errors could have caused your child’s injuries.
If we feel medical negligence caused or contributed to your child’s injuries, we meet with you to discuss how you can receive compensation from the medical professionals who made the errors. Our birth injury attorneys have recovered millions of dollars in settlements for families of children that have suffered a birth injury.
At no point in our legal intake process will we ask you to pay anything. The medical review of your case and the consultation are free. We only receive payment when you do.
Contact Our National Birth Injury Lawyers
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.