Labor and Delivery Complications
Complications During Labor and Delivery

A mother’s complications during labor and delivery can put both her life and her child’s life at serious risk. During this vulnerable time, she entrusts her life into the hands of the healthcare specialists in the room with her.
OB-GYNs, maternal fetal medicine specialists, nurses, midwives, and other healthcare providers have a duty to protect their patients from harm. When they breach this duty (known as the “standard of care”) and cause preventable birth injuries, it constitutes medical malpractice.
Birth Injury Malpractice Attorneys
Our top-rated birth injury attorneys specialize in identifying mismanaged labor and delivery complications. If you or someone you know sustained injuries after a mismanaged delivery, don’t hesitate to contact our firm. We can answer difficult legal and medical questions and investigate the facts on your behalf.
Free Legal Consultation
Birth Injury Lawyers
(888) 987-0005Our Birth Injury Lawyers are available to meet you in your home or the hospital.
Our vast network of medical experts and in-house nursing staff and nurse-attorneys gives us the edge over our competition. When we take your case, we assign you with not just an attorney, but an entire medical team. This team not only consists of attorneys, nursing advocates, and medical experts.
Your team is available to assist with any day-to-day treatment you or your child may need. This includes assistance with medical records, scheduling doctors’ appointments, providing transportation, and any other problems that may arise.
We offer all of this on a contingency fee basis. This means you will not pay any fees until after we win your case and secure a settlement. Miller Weisbrod Olesky’s unmatched track record of birth injury results sets us apart from other birth injury law firms.

Recent Birth Injury Settlement:
Birth Injury settlement against a hospital in which nurses and physicians failed to properly monitor the mother's blood pressure during delivery causing an HIE event resulting in neonatal seizures and cerebral palsy at birth. Our team of top-rated birth injury lawyers recovered $13,750,000 for the family to help with future medical expenses and developmental therapy.
What Are Labor and Delivery Complications?

Labor and delivery complications are issues or abnormalities that arise while the mother is giving birth to her child. These abnormalities can range from placental complications and umbilical cord problems all the way to neonatal infection and maternal mortality.
It is critical for healthcare providers to be prepared for anything and everything that can go wrong during childbirth. This starts with monitoring for pregnancy complications during prenatal testing and carefully planning for how to address them during labor.
Without the proper diagnosis and treatment of labor and delivery complications, a newborn can suffer from devastating birth injuries. These injuries can come with lifelong consequences and conditions, such as hypoxic ischemic encephalopathy (HIE) or cerebral palsy.
What Are The Most Common Labor and Delivery Complications?
Perinatal Asphyxia

No two things are more important to an unborn baby than oxygen and sufficient blood flow.
A baby’s inadequate oxygen supply is the leading cause of brain damage at birth. Experts use several clinical terms to describe this condition:
- Hypoxia: A deficiency in oxygen.
- Anoxia: The complete lack of oxygen.
- Birth Asphyxia: The medical term experts use to diagnose infants who have suffered from prolonged hypoxia or anoxia.
Many related complications can restrict a baby’s access to enough oxygen. The most common reasons for asphyxia at birth include placental complications, umbilical cord problems, and prolonged or arrested labor.
When medical professionals fail to properly address a baby’s oxygen deprivation, it can have detrimental effects. Perinatal asphyxia can lead to brain injuries like periventricular leukomalacia and hypoxic ischemic encephalopathy (HIE).
These brain injuries often lay the groundwork for a lifetime of seizure disorders, vision impairments, mobility limitations, and developmental delays. It’s also one of the first signs that the baby may receive a cerebral palsy diagnosis later in childhood.
Prolonged And Arrested Labor

A prolonged labor is one that progresses at a slower rate than average. A mother’s first labor typically lasts around 12-18 hours and usually shortens to around 8-10 hours for future pregnancies.
Doctors usually consider a mother’s labor prolonged if her contractions last longer than 20 hours. They sometimes make this call a bit before or after the 20-hour mark, depending on other pregnancy-related factors.
A mother’s labor becomes arrested when progress has ceased completely. This can mean her cervix has stopped dilating and/or her uterus is no longer contracting sufficiently.
The most common causes of prolonged and arrested labor include:
- Fetal Macrosomia: Babies larger in size may have more difficulty progressing through the mother’s birth canal.
- Cephalopelvic Disproportion: Prolonged labor can occur when there’s a mismatch between the baby’s head size and the width of the mother’s pelvis.
- Fetal Malpresentation: Babies with their feet or side pointed toward the birth canal may not be able to fit.
- Hypotonic Labor: A mother’s weak contractions can sometimes prolong or even arrest her labor.
Both prolonged and arrested labor pose a threat to the baby’s oxygen supply. Uterine contractions during labor squeeze on the baby’s head and temporarily restrict their oxygen supply. This process is natural, but the baby can only withstand limited oxygenation for so long before problems start to arise.
Babies deprived of oxygen from prolonged or arrested labor are at a substantial risk for brain damage at birth. It’s important that medical professionals intervene when the mother’s labor shows no signs of progressing. They may need to administer labor-inducing medications or perform an emergency C-section delivery, depending on the circumstances.
Fetal Distress

Fetal distress is a term that describes a condition where a baby’s fetal heart rate pattern is abnormal. Irregular fetal heart rates are almost always a sign that the baby isn’t receiving enough oxygen during the delivery process.
Fetal heart monitoring is an essential tool during childbirth. Healthcare providers typically use an electronic Doppler transducer attached to the mother’s abdomen to monitor the baby’s heart rate.
Medical professionals must carefully monitor several characteristics of the baby’s heart rate, including the baseline, accelerations, decelerations, and variability. A healthy fetal heart rate:
- Accelerates (increases) in response to uterine contractions.
- Has moderate variability (fluctuations) between 6 beats per minute and 25 beats per minute.
- Has a baseline (average heart rate over 10 minutes) between 110 beats per minute and 160 beats per minute.
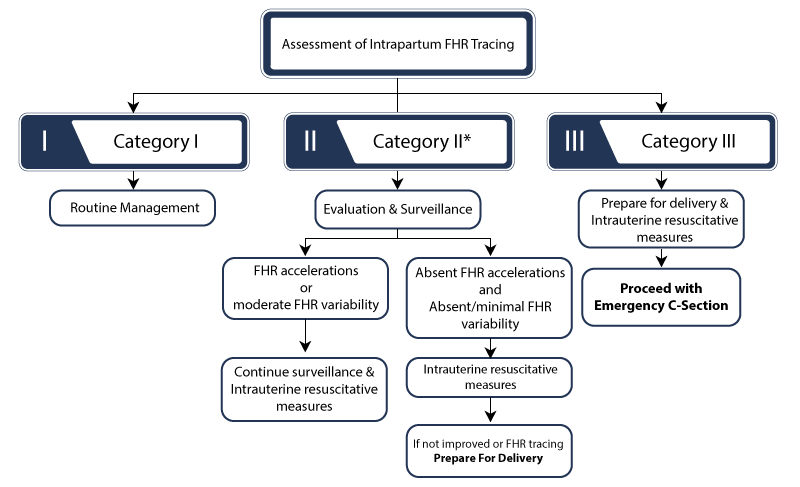
When a baby displays non-reassuring fetal heart rate patterns, it is a sign for doctors to intervene. Specific intervention measures will depend on the severity of each case. Category II heart rates (moderate fetal distress) may require closer evaluation and intrauterine resuscitative measures such as administering supplemental oxygen.
However, category III heart rates (severe fetal distress) may require more urgent measures, such as an emergency C-section delivery.
Fetal Bradycardia
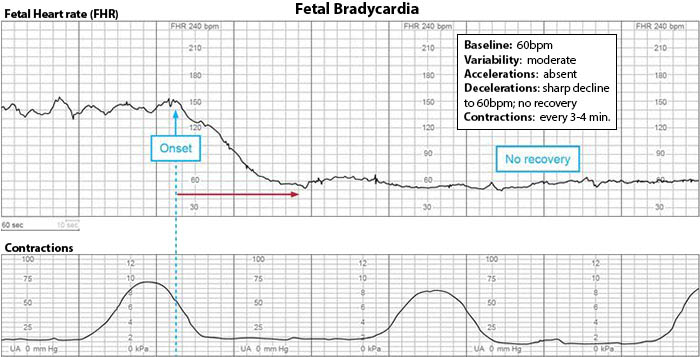
Fetal bradycardia is a type of non-reassuring heart rate pattern where the baby’s baseline heart rate rests under 110 bpm. The most common complications that cause fetal bradycardia include hypoxia and anoxia, umbilical cord complications, placental insufficiency, and prolonged labor.
Doctors must speed up delivery when they identify a baby’s abnormally low heart rates. This can include using delivery instruments or performing an emergency C-section delivery. Delayed reactions increase the risk of hypoxic brain injuries like HIE or even fetal demise.
Fetal Tachycardia
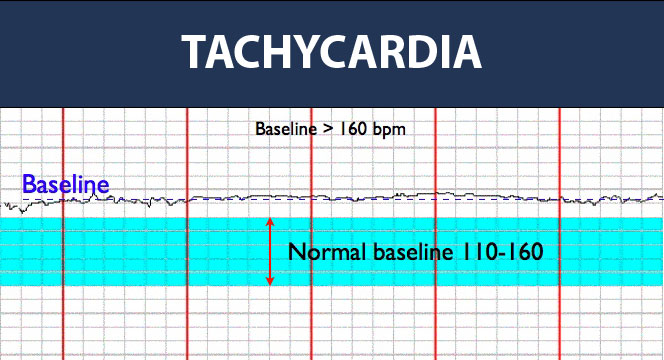
Fetal tachycardia (the opposite of bradycardia) occurs when the baby’s baseline heart rate rests above 160 bmp. Certain factors like infections or fetal anemia can trigger an immune response that causes the baby’s heart to beat faster. Other factors, like prolonged hypoxia or ischemia, can also cause rapid heartbeats to compensate for insufficient oxygenation in the tissues.
Just like with fetal bradycardia and other forms of fetal distress, doctors must carefully monitor the baby’s baseline heart rate. Failing to properly monitor or respond to non-reassuring fetal heart rates can lead to birth injuries and constitute medical malpractice.
Placental Complications

The placenta is an organ that forms within the uterus during an expecting mother’s pregnancy. It is responsible for removing waste and providing oxygen and vital nutrients to the fetus. The fetus receives these nutrients from the placenta via the umbilical cord.
Placental complications during labor and delivery can displace or damage the placenta. When this happens, it can jeopardize the baby’s blood and oxygen supply and put the mother at risk. These types of complications include:
Placental Abruption
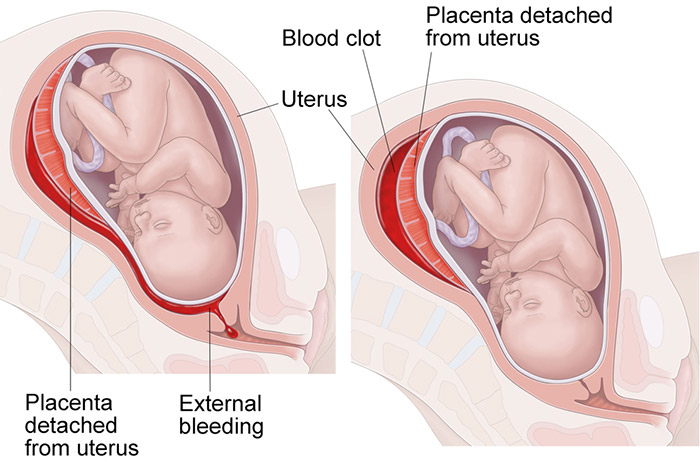
A placental abruption occurs when the placenta prematurely and unexpectedly detaches from the uterine lining. When this happens, the mother can suffer excessive bleeding, shock, and organ failure.
Placental abruptions can also cause ischemia in the baby and deprive them of oxygenated blood flow. As a result, the baby can go into fetal distress and sustain brain injuries like hypoxic ischemic encephalopathy (HIE).
When doctors do not immediately address placental abruptions, there becomes a high risk for both maternal mortality and infant mortality.
Placenta Previa

Placenta previa is a pregnancy complication where the placenta either fully or partially covers the cervix (the uterus opening). Medical professionals can usually identify the condition before labor with ultrasound exams during prenatal testing.
A mother’s placenta previa make the blood vessels connecting placental tissue to the uterus more likely to rupture during delivery. This can cause severe bleeding which will result in fetal distress if doctors do not immediately perform an emergency C-section.
Placenta previa can even cause severe postpartum hemorrhaging after birth, endangering the mother’s life if doctors can’t stop the bleeding.
Retained Placenta
A retained placenta occurs when the mother’s placenta or traces of placental tissue remain stuck inside her uterus. Healthcare providers may also refer to this condition as retained products of conception (RPOC). This can happen after a traditional birth or in cases of miscarriage, such as an ectopic pregnancy or a blighted ovum miscarriage.
Retained products of conception are more likely after C-section deliveries or assisted deliveries with instruments like forceps and vacuum extractors. While it does not cause complications to the baby, the tissue can become infected and make the mother sick.
Doctors and all other medical professionals must carefully monitor the mother’s placenta during pregnancy and labor for any visible complications.
Umbilical Cord Problems

The umbilical cord is the baby’s lifeline during pregnancy. It plays a vital role in delivering oxygen and nutrients to the fetus while in utero.
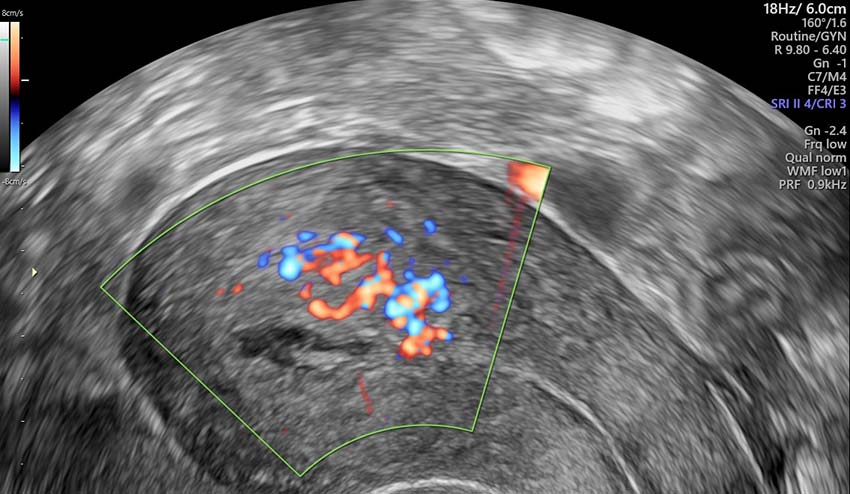
Certain abnormalities and complications can disrupt the cord’s ability to function properly. Doctors and medical providers can use ultrasound technology during prenatal testing to diagnose many of these umbilical cord problems.
The most common types of umbilical cord complications to affect labor and delivery include:
Umbilical Cord Prolapse

Umbilical cord prolapse is a complication where one or more loops of the cord slip through the cervix before the baby.
This causes the baby’s head to press against the cord. This completely compresses the cord, either reducing or fully stopping the flow of blood and oxygen to the baby.
Umbilical cord prolapse is a medical emergency requiring immediate intervention from medical professionals in the delivery room. Doctors must perform an emergency C-section to prevent the risk of birth asphyxia or brain damage at birth.
Nuchal Cord

A nuchal cord is a type of umbilical cord problem where the cord gets wrapped around the baby’s neck. Nuchal cords commonly develop during labor but can sometimes occur earlier in pregnancy, depending on the amount of fetal movement.
The most common causes of nuchal cords include:
- Polyhydramnios: Excessive amniotic fluid within the womb will give the baby freedom to move around more.
- Long Umbilical Cord: A typical umbilical cord is between 19 and 23 inches. Doctors generally consider cords longer than 27 inches to be “long.” Naturally, a baby is at an increased risk to wrap a longer cord around their neck as they move around.
- Complications with Twins: When a mother is carrying twins or even more children, it becomes easier for them to get tangled.
- Post Term Pregnancy: Babies with more time in the womb (past 40 weeks gestation) have more opportunities to move around and get tangled.
While many cases of nuchal cord resolve on their own, tightly wrapped cords put the baby’s oxygen supply at risk. Prolonged hypoxia from nuchal cords can increase the baby’s risk for fetal distress and associated brain injuries from oxygen deprivation.
Major disruptions to the umbilical cord can fully stop the flow of oxygenated blood from reaching the baby’s brain. This often leads to hypoxic ischemic encephalopathy (HIE) and other forms of brain damage that cause cerebral palsy.
Emergency C-Section Delivery

A cesarean section delivery (or C-section delivery) is a medical procedure where doctors cut into the mother’s abdomen and uterus. They deliver the baby through this incision in cases where vaginal birth is either impossible or too risky to attempt.
Doctors can pre-plan a mother’s C-section in cases where known pregnancy complications will rule out a vaginal birth. But in other cases, certain labor and delivery complications will require an emergency C-section. Examples of such complications include:
- Fetal distress
- Prolonged hypoxia or birth asphyxia
- Prolonged or arrested labor
- Uterine Rupture
- Umbilical Cord Prolapse or Compression
The current standard of care dictates that doctors perform a C-section no later than 30 minutes after determining its necessity. In some cases, however, doctors will need to perform the procedure even faster to avoid birth complications for the baby.
C-section deliveries have longer recovery periods and increase the mother’s risk for complications like postpartum hemorrhage and retained placental tissue. Doctors must assess the risk factors and swiftly perform the operation to limit the mother’s and baby’s risks for injury.
Uterine Rupture
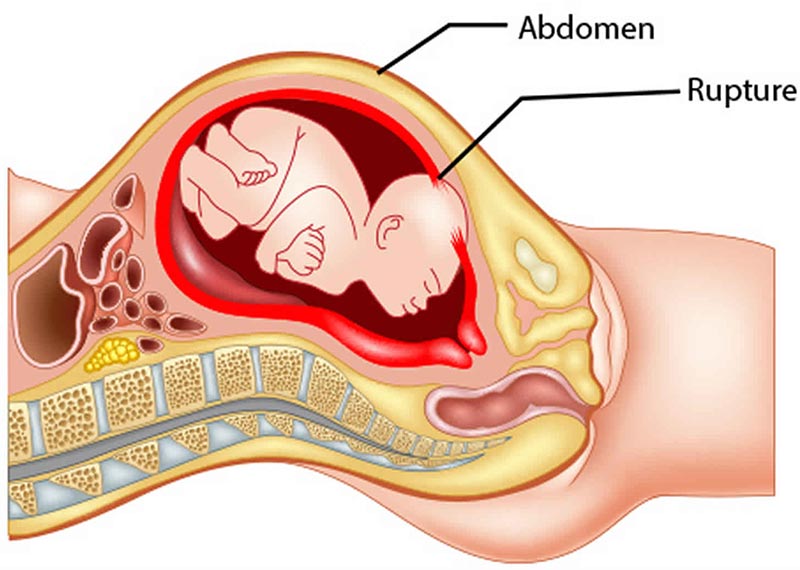
A uterine rupture is a serious labor complication that is somewhat rare but life-threatening. It occurs when one or multiple layers of uterine tissue split or rupture while the baby is still inside.
Common causes of uterine ruptures include:
- Uterine Hyperstimulation or Tachysystole: Intense or overly frequent contractions place additional stress on the uterus, making it prone to tearing.
- Precipitous Labor: A rapid labor can increase a mother’s risk for uterine tearing and lacerations.
- Vaginal Birth After Cesarean (VBAC): Uterine incisions from previous C-sections can increase the risk of ruptures when the mother attempts to deliver vaginally.
- Abnormal Fetal Positioning: A baby in breech position or shoulder position can cause rupturing as they attempt to exit the mother’s uterus.
A uterine rupture is always a medical emergency that requires an emergency delivery of the baby.
Babies born after their mother’s uterine rupture could suffer severe, permanent physical damage. Some may suffer from brain injuries like hypoxic-ischemic encephalopathy (HIE). Newborns with HIE will have life-long disabilities, including cerebral palsy and related physical and cognitive impairment.
Uterine Tachysystole and Hyperstimulation
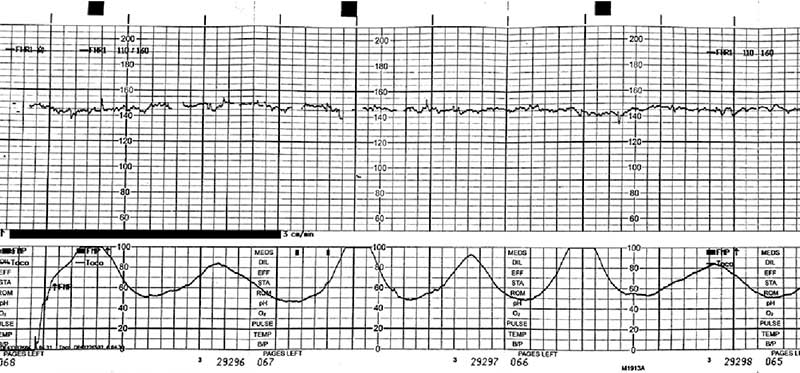
During labor and delivery, the term uterine tachysystole refers to excessive uterine activity or contractions.
A series of abnormally strong contractions during labor is associated with fetal heart rate decelerations. Prolonged decelerations are a sign of fetal distress and indicate the baby isn’t receiving enough oxygen.
A baby can withstand a certain degree of diminished oxygenation. However, when uterine tachysystole contractions occur too frequently, they can cause dangerous levels of oxygen deprivation.
Uterine hyperstimulation occurs whenever there is any increase in uterine activity associated with an irregular fetal heart rate. Like uterine tachysystole, it can result in more frequent contractions. But hyperstimulation also increases the intensity of these contractions as well, increasing the risk of uterine ruptures or placental abruptions.
Uterine hyperstimulation and tachysystole can both lead to oxygen deprivation and fetal distress. Early detection through fetal heart rate monitoring is crucial to preventing excessive uterine from causing a birth injury.
About Uterine Hyperstimulation
Uterine Atony

Uterine atony occurs when the uterus fails to contract after delivery. When left untreated or insufficiently treated, it can cause excessive bleeding that threatens the mother’s life. Globally, postpartum hemorrhage is one of the leading causes of maternal mortality.
Healthcare providers must understand and be alert to the signs of uterine atony and the methods for treating it. When they make negligent errors that worsen a mother’s injuries or cause her untimely death, it can constitute medical malpractice.
Postpartum Hemorrhage
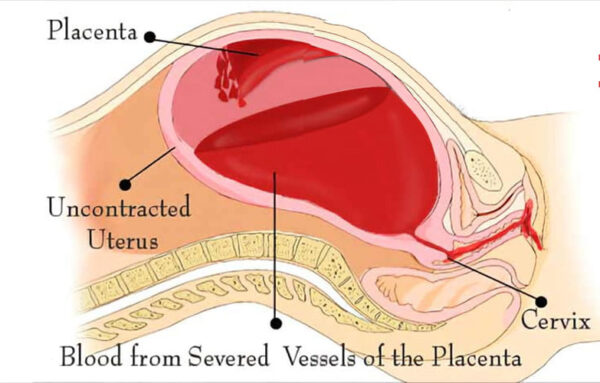
A postpartum hemorrhage refers to severe vaginal bleeding after childbirth.
Doctors expect minimal to moderate bleeding after the mother’s delivery. However, losing over a liter (33 fluid ounces) of blood is abnormal and grounds for immediate medical intervention.
A postpartum hemorrhage can occur from several labor and delivery complications, including uterine atony, blood clots, and birth trauma. A mother can suffer from birth trauma after a uterine rupture or injury from forceps or vacuum extractors.
Doctors should identify postpartum hemorrhage when the mother’s vaginal bleeding is heavy, persistent, and uncontrollable.
Meconium Aspiration Syndrome

Meconium is a baby’s first feces. Meconium aspiration syndrome (MAS) occurs when the baby breathes in a mixture of amniotic fluid and meconium into their lungs.
MAS is a major cause of serious medical complications or death in infants. Common causes and risk factors include both premature birth and post term pregnancy, prolonged labor, and oligohydramnios.
On X-rays and ultrasounds, doctors can see when meconium lines the intestines of the fetus. Oxygen deprivation during labor, infection, and other causes of fetal distress can all make the baby gasp for breath. As this happens, the baby may inhale meconium mixed with amniotic fluid into their lungs.
Quick aspiration of the meconium at childbirth can present serious lung injuries like respiratory distress syndrome (RDS). It can also increase the risk of asphyxia leading to brain injuries from the oxygen deprivation.
Medial providers’ alertness to the signs of MAS can help prematurely predict the baby’s risk and prepare for timely treatment.
Mismanaged Fetal Malposition

Fetal position is very important when it’s time for labor and delivery. The best position for the unborn child is known as occiput anterior. This means that the baby is facing head down in its mother’s pelvis toward her spine.
Unborn babies will usually spin and flip within their mother’s uterus until a few weeks before delivery. But by around the 36th week of pregnancy, most babies eventually settle into one position.
Positions like breech or shoulder presentation can make it impossible for the baby to fit through the mother’s birth canal. This can cause prolonged labor and contribute to oxygen deprivation and fetal distress during labor.
Medical professionals should catch dangerous positions and presentations during prenatal testing visits using ultrasound or physical examinations. The baby’s delivery will often require medical intervention when position or presentation is not optimal. Failing to diagnose and manage abnormal fetal positions and presentations is medical malpractice.
Shoulder Dystocia
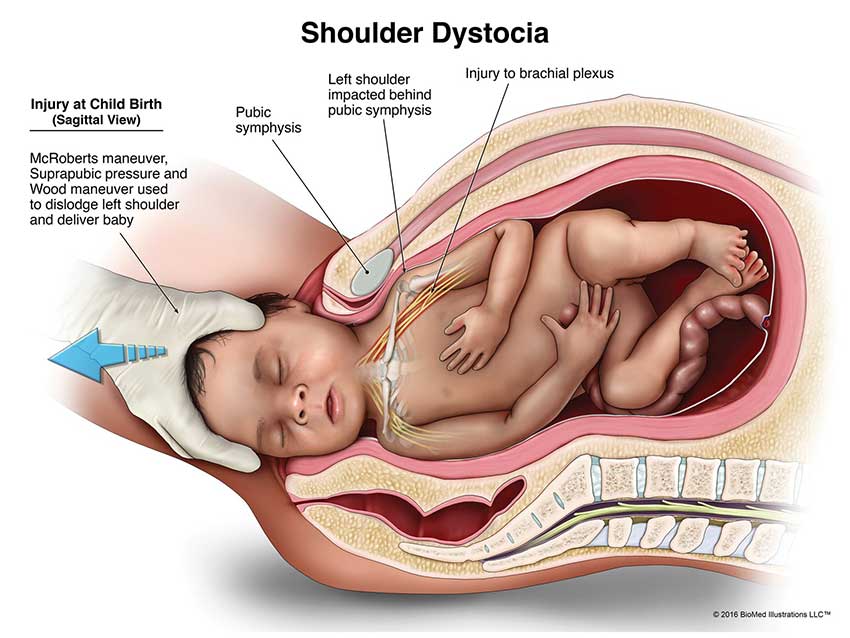
Shoulder dystocia occurs when the baby’s shoulders become stuck behind the mother’s pubic bone in the pelvis.
The complication is rare, occurring in between 0.7% and 3% of all births. Macrosomia, when the baby is larger in size than average, is the most common cause of shoulder dystocia. Other factors, such as maternal obesity or an abnormal pelvic shape, can also contribute to a baby’s risk.
Shoulder dystocia can cut off circulation to the baby’s head and increase their risk for a brachial plexus injury. It can also cause collarbone fractures during birth and increase the risk for nerve damage and paralysis.
When shoulder dystocia occurs, doctors should apply suprapubic pressure to the mother’s lower abdomen to ease the baby out. They may also consider using delivery instruments such as forceps and vacuum extractors.
Applying fundal pressure, using excessive force with delivery instruments, or failing to intervene at all can worsen a baby’s injuries. When this happens, it can be grounds for a medical malpractice claim.
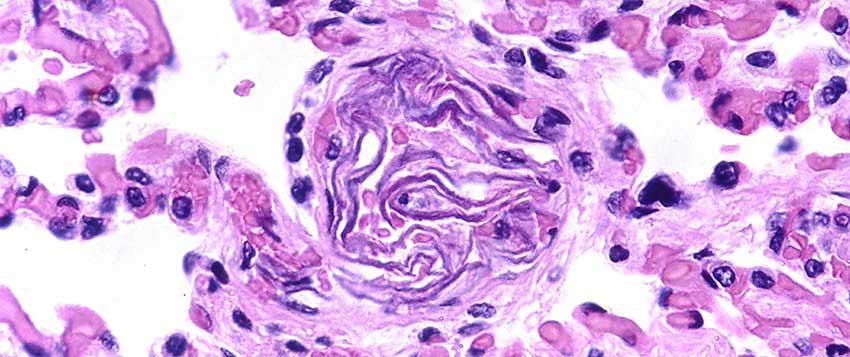
Jaundice (Kernicterus)

Newborn babies sometimes develop jaundice, which is a yellowish color in their skin and eyes shortly after birth.
The substance causing the yellow discoloration is bilirubin, a waste product created after red blood cells break down. The bilirubin normally travels to the liver, which breaks it down further before excreting it from the body.
When the baby’s liver is unable to get rid of bilirubin through this process, they may develop “hyperbilirubinemia.” This means the baby’s blood has a high level of bilirubin, resulting in a yellowish discoloration of the skin.
Jaundice is highly treatable and relatively low risk to the baby’s overall wellbeing, but untreated cases can progress into kernicterus. Kernicterus is a more serious complication that occurs when prolonged high bilirubin levels cross through the blood-brain barrier. Bilirubin then seeps into the brain, causing severe brain damage.
Brain injuries resulting from kernicterus can often be a precursor to a cerebral palsy diagnosis later in childhood. It is important for doctors to treat jaundice cases early before it advances to this level.
Premature Birth

The final weeks of pregnancy are vital for the full development of the baby’s lungs, brain, and liver. Babies with a premature birth (especially before 32 weeks gestation) are at higher risk for severe birth injuries.
Common complications premature babies may experience include low birth weight, developmental delays, breathing problems, vision impairments or hearing problems. They are also at an increased risk for infant death.
Doctors can sometimes delay premature delivery using various medications and treatments. They do this to give the baby more time to fully develop. When premature delivery is unavoidable, medical providers should administer medications that speed up development of critical organs like the lungs. A common medication used for lung development is Betamethasone.
Specialized care teams like neonatal intensive care specialists must immediately treat common complications of a premature birth. They must prepare to provide respiratory therapy or neonatal resuscitation in the neonatal intensive care unit. Failing to immediately treat complications can increase the risk for long term conditions like cerebral palsy.
Precipitous Labor

A precipitous labor occurs when the mother gives birth in under three hours after her water breaks.
The contractions a mother undergoes during precipitous labor can be so forceful that they damage the uterine lining. If this happens, it can cause severe internal bleeding and postpartum hemorrhage. Perineal tears and vaginal lacerations can also contribute to heavy bleeding after a mother’s rapid labor.
Rapid labor is also associated with birth trauma for the child is they progress too quickly through the birth canal. In some cases, rapid labor can also trigger a placental abruption or cause the placenta to remain inside the uterus. Both complications pose serious risks to the mother’s health.
Healthcare providers must carefully monitor a mother for any complications following her precipitous labor.
Labor Complications with Twins

Twin labor involves a much higher risk for birth injuries and birth complications. The most common complications include:
- Premature Birth: Over 60 percent of twins and nearly all higher-order multiples are premature.
- Gestational Hypertension: Mothers with multiple fetuses are more than twice as likely to develop high blood pressure during pregnancy.
- Anemia: Anemia is more than twice as common in pregnancies with multiples.
- Birth Defects: Twin babies have twice the risk of congenital defects, such as neural tube defects, gastrointestinal, and heart abnormalities.
Twin labor also increases the likelihood for prolonged labor and fetal demise. Because of this, doctors sometimes pre-plan to perform a C-section delivery to avoid those risks. Regardless of the planned delivery method, healthcare professionals must monitor mothers expecting multiples more carefully than other labors.
About Complications with Twins
Infections at Birth

Maternal infections can lead to direct transmission to the fetus or a newborn during labor and delivery. Direct transmission may also occur during labor and delivery with infected maternal blood or genital secretions.
Some of the most common infections that pose a risk to a mother and her baby include:
Group B Strep
Chorioamnionitis Bacterial Infection
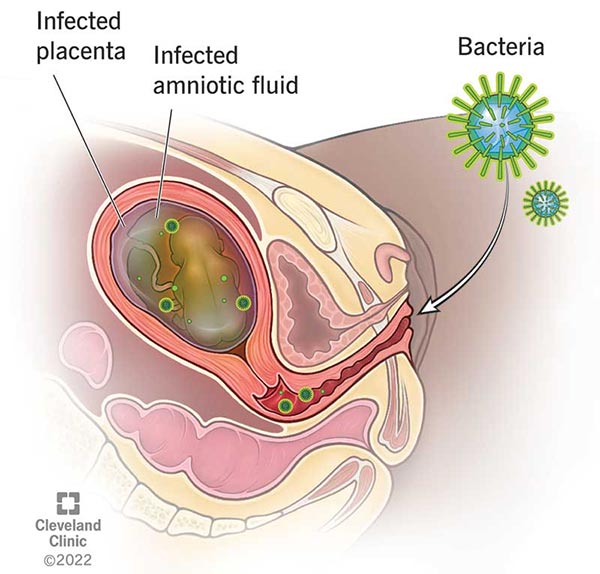
Chorioamnionitis is an acute bacterial infection that enters the mother’s uterus and infects the amniotic fluid surrounding the baby. The most common bacteria causing chorioamnionitis are Group B Strep and E.coli.
Chorioamnionitis typically occurs when the amniotic sac breaks prematurely prior to birth. This complication is known as “premature rupture of membranes” or PROM. Amniotic fluid is also more likely to become infected during a prolonged labor.
Untreated or mismanaged chorioamnionitis infections can lead to serious complications for the baby. Some of the most serious complications can include preterm birth, neonatal meningitis, neonatal sepsis, pneumonia, and cerebral palsy.
Birth-Acquired Herpes
Herpes simplex virus (HSV) is an infection that a mother can transfer to her child during pregnancy. A mother’s unhealed genital herpes outbreak during labor can infect the child as they pass through the vaginal cavity.
There are two main types of herpes. HSV-1 can present as skin lesions/blisters around the eyes and mouth, while HSV-2 affects areas on or around the genitals.
For newborns, however, doctors can identify herpes from other symptoms outside of blistered skin. Symptoms may include low-grade fevers, breathing difficulties, blue appearance around the skin, or extreme irritability with high-pitched cries.
It is highly important that medical professionals carefully monitor expecting mothers for infections during prenatal testing visits. When doctors either fail to catch or fail to treat a maternal infection, it can develop into a neonatal infection. If a baby becomes infected through uncaught maternal infections, it may constitute medical malpractice.
Amniotic Fluid Embolism
An amniotic fluid embolism occurs when amniotic fluid enters the mother’s bloodstream and causes an allergic-like reaction.
The mother’s immune system registers the fluid in her blood as an external threat, triggering an inflammatory response. The inflammation causes blood clotting in blood vessels that travel to the lungs, which results in an amniotic fluid embolism.
Damage to the placenta during the baby’s delivery can allow amniotic fluid to exit the womb and enter the bloodstream. For the child, this can affect the flow of blood and oxygen and result in several serious complications. This can include brain injuries, birth asphyxia, fetal distress, and even fetal demise in extreme cases.
Amniotic fluid embolisms are rare and estimated to occur in 1 in 40,000 deliveries. But despite its rarity, it is important healthcare providers recognize the signs so they can prevent further harm during delivery.
About Amniotic Fluid Embolisms
Anesthesia Errors

Doctors will administer local, regional, or general anesthesia for pain relief during labor procedures like C-section deliveries. However, anesthesia errors can increase the risk of injury to both the mother and her baby.
Common anesthesia errors include:
- Prescribing too high of a dosage of the anesthetic medication.
- Intubation errors (incorrect tube positioning in the airway or disconnected, overinflated or damaged tube).
- Communication errors between the anesthesiologist and the rest of the perinatal team.
- Failing to properly monitor fetal heart rates in response to the anesthesia.
Mistakes when prescribing or administering anesthesia put the baby at an increased risk for hypoxia, fetal acidosis, and fetal distress. In some cases, the adverse outcomes for the baby may include hypoxic-ischemic encephalopathy (HIE), which is a major cause of cerebral palsy.
Misuse of Delivery Instruments
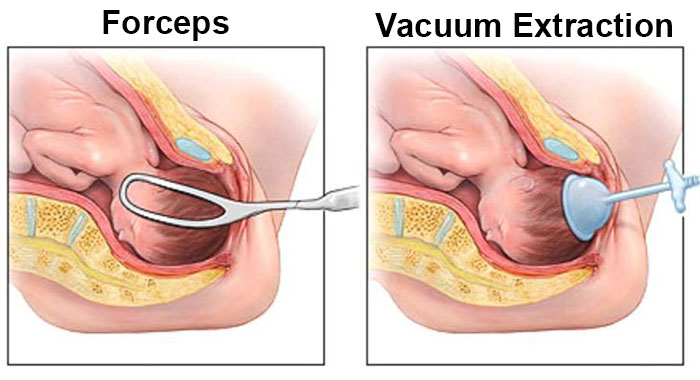
Physicians sometimes recommend assisted vaginal delivery when a baby has difficulty travelling through their mother’s birth canal. Forceps and vacuum extraction are two types of equipment doctors may use for assisted vaginal delivery.
Delivery instruments can protect a baby from injury in cases of prolonged labor or shoulder dystocia. However, when used incorrectly, they can also contribute to several birth injuries and adverse neonatal outcomes.
Using excessive force can increase a baby’s risk for neonatal head injuries like skull fractures, caput succedaneum or intracranial hemorrhages. These kinds of injuries can come with long term neurological effects such as cerebral palsy later in childhood.
Doctors must exercise extreme caution when performing an assisted delivery. If the delivery instruments prove to be unsuccessful, they should perform an emergency C-section delivery. Delaying a C-section or not abandoning a failing assisted delivery can cause further injury and constitute medical malpractice.
About Forceps Extraction Injury
Maternal Mortality Risk

A mother’s death during labor or shortly thereafter can be painfully devastating for the people she leaves behind. It only becomes more devastating with the knowledge that her death was preventable.
The most common causes of maternal mortality include:
- Postpartum Hemorrhage: Excessive blood loss following a labor and delivery complication is the leading cause of maternal death.
- C-Section Errors: Failing to perform a C-section in time can be the difference between life and death for an expecting mother.
- Maternal Infections: Severe infections like meningitis, tuberculosis, or sepsis can be fatal when doctors fail to treat them.
Healthcare professionals commit medical malpractice when they make errors that result in a mother’s preventable death. These errors can include mistakes before labor and delivery, such as missing pregnancy complications.
Did Medical Malpractice Cause My Labor Complication?

Many common complications arising during labor and delivery are preventable, or can at least be treated, with proper medical care. Birth Injury Medical negligence, such as a misdiagnosis or failure to catch early symptoms of a problem, or operating errors during delivery can cause injury to you or a birth injury for your child.
If a family believes medical negligence contributed to a birth complication or birth injury, legal support may be an option. A knowledgeable birth injury attorney can review the medical records and circumstances to assess whether a claim exists.
Parents whose children suffer from the long-term effects of birth complications, as well as parents who have suffered the loss of their baby, deserve to know whether it could have been prevented. Our top-rated birth injury lawyers want to help you find those answers and obtain the funds necessary to improve the quality of life for your child.
If your child has been diagnosed with a birth injury and you suspect this may have been caused in part by medical mistakes, Miller Weisbrod Olesky will thoroughly investigate the facts and hold the responsible medical providers accountable by pursuing medical malpractice claims against them.
Sometimes families are hesitant to reach out to a medical malpractice attorney or law firm. They may feel overwhelmed by their circumstances or are worried that a law firm will not be able to help them. But the only way to find out if you have a case is to talk to an attorney who understands how birth injuries can lead to developmental delays and other complications that require long-lasting medical support.
What is the Statute of Limitations in a Birth Injury Lawsuit?
A statute of limitations (SOL) is a law that sets a time limit on how long an injured person has to file a lawsuit after an accident. It is essential to understand that statutes of limitations vary based on the type of case and the state where it is filed. For instance, the deadline for birth injury claims is typically different from other claims, such as injury to personal property, fraud, contract disputes, and collection of debts.
Generally, the clock starts ticking on the date the injury occurred. However, there are exceptions to this rule, and in some cases, the statute of limitations starts when a person discovers or reasonably should have discovered an injury.
When dealing with government agencies, SOLs can become even more complex.
For example, if the party that injured you was:
- A federal employee
- Employed by a military hospital, Veterans Administration facility, or a federally funded medical entity
You may need to file a birth injury claim under the Federal Tort Claims Act (FTCA). In FTCA cases, claimants must go through certain administrative procedures before filing a lawsuit. In some states, if the negligent party was a local or state government hospital or the doctors and medical providers are employees of a governmental entity, the time period in which you must give "notice" may be shorter.
If your case is filed outside of the statute of limitations, it will typically be dismissed, and you will not be eligible to recover compensation for your injuries. Determining when a statute of limitations begins on your case can be tricky. If you're considering pursuing compensation for a birth injury, contacting an attorney as soon as possible is in your best interest.
How Can Birth Injury Attorneys at Miller Weisbrod Olesky Help?

Birth injuries that trace back to labor and delivery complications can be prevented in many cases, but it takes a detailed expert review of the facts and circumstances of your pregnancy and your child's birth to determine whether the injury was the result of medical malpractice.
Our Process
At Miller Weisbrod Olesky, a team of committed attorneys, nurses and paraprofessionals uses our detailed medical negligence case review process to assess your potential birth injury case. We start by learning more about you and your child and the status of meeting/missing developmental milestones. Then we gather medical records to determine what happened before, during, and after your delivery. We call in skilled medical experts who review your records and let us know if they think medical errors could have caused you or your child's injuries.
If we feel medical negligence caused or contributed to complications with your pregnancy or your child's injuries, we meet with you to discuss how you can receive compensation from the medical professionals who made the errors.
At no point in our legal intake process will we ask you to pay anything. The medical review of your case and the consultation are free. We only receive payment when you do. The sooner you reach out to us, the sooner we can begin investigating your case and gathering the evidence needed to support your claim.
We work on a contingency fee basis, meaning you won't pay any legal fees unless we win your case. Contact us today to schedule your free consultation by calling our toll-free line at (888) 987-0005 or by filling out our online request form.
Contact Miller Weisbrod Olesky
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.

