APGAR
Understanding APGAR Scores
An Important Test Every Newborn Is Given
Labor and delivery place a great deal of stress on both the mother’s and baby’s bodies. Medical professionals must rely on testing and observation immediately after delivery to assess the baby’s risk for any birth complications.

The APGAR test is one of the quickest and most universal methods labor and delivery specialists use for identifying serious issues upon birth.
Low APGAR scores are often the first sign of a baby having a serious birth injury that needs immediate treatment. Common examples of these injuries include birth asphyxia, neonatal strokes, and brain injuries like hypoxic ischemic encephalopathy.
APGAR Scores and Medical Malpractice
Doctors and medical professionals can use APGAR scores to quickly and succinctly communicate a baby’s status. This is important because complications like fetal distress or brain damage at birth require immediate intervention.
Sometimes, however, healthcare providers misinterpret a baby’s status or miss the critical signs of a complication at birth. Assigning an inaccurate APGAR score can needlessly delay a child’s timely treatment and risk its effectiveness.
Birth injury treatments like neonatal resuscitation and therapeutic hypothermia are most effective immediately after birth. Delaying urgent treatment for any reason can have lifelong consequences. A child’s mismanaged treatment at birth can be the catalyst for delayed developmental milestones and debilitating conditions like cerebral palsy.
Birth Injury Medical Malpractice Attorneys

When child receives improper treatment at birth and it leads to avoidable future complications, it qualifies as medical malpractice. Our specialized birth injury attorneys have a long track record of results securing compensation for victims of birth injury negligence.
If you believe birth injury medical malpractice contributed to your child’s current conditions, you may be eligible for compensation. The attorneys, nurses, and staff of Miller Weisbrod Olesky are committed to ensuring your child receives the best possible support. We will fight tirelessly to obtain justice on your behalf by holding all negligent parties accountable for their mistakes.
If you live within any of our service areas, we are available to analyze the facts of your case. You can call us today at (888) 987-0005 or fill out our convenient online form to schedule a free consultation.
At no point in our legal intake and lawsuit process will you have to pay any attorneys’ fees or expenses. The medical review of your case and the legal consultation are free. We only receive payment once you do.

Recent Birth Injury Settlement:
Birth Injury settlement against a hospital in which nurses and physicians failed to properly monitor the mother's blood pressure during delivery causing an HIE event resulting in neonatal seizures and cerebral palsy at birth. Our team of experienced birth injury lawyers recovered $13,750,000 for the family to help with future medical expenses and developmental therapy.
What Is An APGAR Score?
The APGAR test is a routine, standardized assessment of a newborn’s physical qualities immediately upon delivery. Medical professionals award “points” across 5 separate categories:
- Appearance: Analyzing the baby’s skin color and blood circulation.
- Pulse: Analyzing the baby’s heart rate.
- Grimace: Analyzing the baby’s reflexes and response to its surroundings.
- Activity: Analyzing the baby’s muscle tone and movement.
- Respiration: Analyzing the baby’s breathing and lung capacity.

Each category receives a score from 0 to 2, with 2 being the most reassuring and 0 being extremely alarming. Doctors then sum up the scores from all categories to deliver the official APGAR score.
Medical professionals assign an APGAR score to all babies after birth, even standard births without labor and delivery complications. They will typically conduct the evaluation and assign a score all within the child’s first minute of life.
How to Interpret APGAR Scores?
A baby’s APGAR score will range from 0 to 10.
- Score of 7-10 = reassuring: The baby appears to be normal based on the APGAR score. However, doctors must always consider the score in context. Even newborns who suffered from birth injuries may have a normal APGAR score.
- Score of 4-6 = moderately abnormal: Doctors consider any APGAR score below 7 to be low. The baby will need immediate intervention until their APGAR score increases above 7.
- Score of 0-3 = abnormal: The baby requires immediate attention and likely admission to the Neonatal Intensive Care Unit (NICU) for further observation and assessment.

The APGAR score gives the medical team a quick and standardized way to determine the baby’s next steps for treatment. It also makes it easier to report the status and communicate to other team members in language they immediately understand.
What Does the Total APGAR Score Mean?
The medical person assessing the baby adds the scores for each category (0 – 2) to arrive at a total ranging from 10 (the highest) to 0.
- Score of 7-10 = reassuring. The baby appears to be normal based on the Apgar score. However, the score should always be considered in context. Newborns that suffered birth injuries may have a normal Apgar score.
- Score of 4-6 = moderately abnormal. Immediate intervention is needed until the baby’s Apgar score increases above 7.
- Score of 0-3 = abnormal. The baby requires immediate attention and likely admission to the Neonatal Intensive Care Unit (NICU) for further observation and assessment.
A score of 10 is unlikely because most newborns have some blue tinge on their hands and feet. The lowest score is very serious and causes concern for possible intrauterine problems during labor.
How Do Medical Professionals Calculate APGAR Scores?
Medical professionals look for specific criteria immediately after delivery when calculating the baby’s score. Some specific examples include:
- The color of the baby’s lips, hands and feet.
- Neonatal heart rates above or below 100 bpm (beats per minute).
- The tone of the baby’s cry (or lack thereof).
- Flexed arms and legs or “floppy” appearance.

Doctors, nurses, and nurse practitioners will sometimes conduct the APGAR test multiple times:
One Minute APGAR Score
The one-minute APGAR score is the first and arguably most important score for determining a baby’s need for intervention. If the baby scores above a 7, doctors do not need to intervene nor conduct further APGAR testing.
However, it’s important to note that even healthy infants can have a slightly low APGAR score in the first minute. Categories like Appearance or Grimace may appear low at first but naturally improve within a few minutes.
Even still, medical professionals must contextualize the score with what they know about the mother’s delivery when determining next steps. Taking extra precaution and intervening is always better than delaying intervention out of fear that it’s unnecessary.
Five Minute APGAR Score
Medical professionals assess the baby again at five minutes if they received a concerning score the first time around. Many infants with a low one-minute APGAR scores recover by their five minute test after receiving treatment like neonatal resuscitation.
The five-minute APGAR score becomes even more important for babies with a low one-minute APGAR. If low scores continue, the infant is at greater risk for brain damage and cerebral palsy. A score of 0-3 at the five-minute mark can be a sign of brain injuries like hypoxic ischemic encephalopathy (HIE).
Neonatal resuscitation often begins immediately after birth and before the one-minute APGAR score. An improvement between the one-minute and five-minute scores can indicate the newborn is responding well to treatment.
When a baby’s score is less than 7 at the five-minute mark, medical professionals should continue interventions. Thery can repeat the APGAR assessment every five minutes for up to twenty minutes after birth.
What Causes Low APGAR Scores?

A number of factors during labor and delivery can negatively impact a baby’s APGAR score. Different labor and delivery complications will affect separate categories, including:
Birth Asphyxia

Birth asphyxia occurs in the womb when any type of blockage stops oxygenated blood from flowing to the baby’s brain. Prolonged birth asphyxia for even a short time can increase the chance of brain injuries like hypoxic ischemic encephalopathy and periventricular leukomalacia.
Prolonged birth asphyxia has the potential to affect all five categories of the APGAR score.
Fetal Distress

Fetal distress is a term used to describe a baby with a non-reassuring fetal heart rate. “Non-reassuring” can mean that the baby’s heart rate is abnormally high, abnormally low, or rapidly shifting from high to low. Abnormal fetal heart rates are typically a sign that the baby isn’t receiving adequate levels of blood and oxygen.
A baby who suffers from fetal distress during delivery is at high risk for breathing complications like Respiratory Distress Syndrome. They are likely to score lower on the Respiration and Pulse categories of the APGAR assessment.
Premature Birth

Doctors consider babies born before 37 weeks gestation to be premature. Premature babies (especially before 32 weeks gestation) are at risk for underdeveloped organs, most notably underdeveloped lungs, brain, and liver.
A baby with a premature birth may score lower on the Respiration category of the APGAR assessment if their lungs remain underdeveloped. If their brain is underdeveloped, it can negatively affect the Grimace and Activity categories as well.
Placental Complications
Umbilical Cord Problems

The umbilical cord is just as important as the placenta in delivering blood, oxygen, and nutrients to the baby. Umbilical cord problems like knots, compression, or nuchal cords can similarly increase the risk of fetal distress.
Umbilical cord complications, when causing fetal distress, can primarily affect the Respiration category of the APGAR test. However, like with placental problems, serious complications can affect the brain and lead to lower scores for Grimace and Activity.
Risk Factors for Low APGAR Scores

Multiple complications during labor and delivery can increase the baby’s risk for a low APGAR score. Examples of these risk factors include:
- C-sections: Babies born by cesarean section (C-section) often have lower one-minute Apgar scores. Most recover quickly unless other conditions are present.
- Birth Trauma: If a baby suffers from a traumatic birth injury, it will almost certainly impact their APGAR score. Examples include injuries from forceps and vacuum extractors and neonatal head injuries like intracranial hemorrhaging when doctors use excessive force.
- Pregnancy Complications: A mother’s complications during pregnancy like gestational diabetes or preeclampsia can contribute to complications that lower a baby’s APGAR score.
It is important for both the mother’s and baby’s wellbeing that doctors accurately identify potential complications before birth. They should catch any concerning pregnancy complications during routine prenatal testing and carefully plan any potential operations during delivery.
How Do Medical Providers Treat Low APGAR Scores?

Treatment for a baby with low APGAR scores will depend on the specific categories they scored low in. Not all low APGAR scores have the same cause, so it’s important for doctors to pinpoint specific complications to treat.
Neonatal Resuscitation

Neonatal resuscitation is the most common form of treatment for infants who score poorly in Respiration and Pulse. Babies with blueish lips, weak heart rate, and shallow breaths should receive immediate supplemental oxygen in the neonatal intensive care unit.
During neonatal resuscitation, healthcare providers stabilize the baby and provide ventilation either through machines or performing positive pressure ventilation. They may also perform chest compressions or administer medications.
Neonatal breathing mismanagement such as delaying resuscitation can lead to hypoxia and cause brain injuries or even death.
Therapeutic Hypothermia

Brain cooling treatment or therapeutic hypothermia involves cooling the baby’s core temperature to around 92.3 degrees Fahrenheit. Medical providers place the baby in a thermal regulating machine, which are present in many neonatal intensive care units (NICUs).
Babies with the lowest APGAR scores often have some form of hypoxic-ischemic brain damage. Brain cooling can slow cell depolarization and death and limit the extent of these injuries.
Medical professionals have a responsibility to administer urgent treatment when they notice a baby’s low APGAR scores. Delaying these two critical treatments can lead to more serious disabilities in the future.
Low APGAR Scores and Medical Malpractice
Medical professionals should develop a treatment plan for every baby upon birth. However, they must base this plan on more than just the APGAR score. They must consider other potential factors, including:
- whether the baby showed signs of fetal distress before birth
- whether the baby displays any signs of brain damage like hypoxic-ischemic encephalopathy
- any pre-existing maternal or fetal medical conditions
- which category of the APGAR score is low

The APGAR score is meant to be a snapshot of the baby’s condition shortly after birth. However, medical professionals generally do not use a newborn’s APGAR score to predict their long-term outcome. In fact, an infant could have an acceptable APGAR score but still have suffered brain damage during birth.
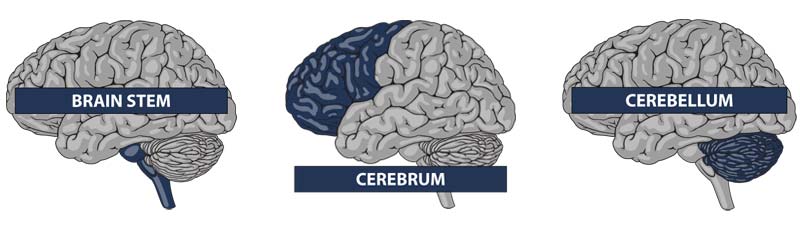
Several parts of the APGAR score assess activity that the baby’s brainstem controls. While the brainstem may have escaped injury, damage to the cerebrum or cerebellum is entirely possible. These kinds of brain injuries may not appear for months or even years after the baby’s birth.
Another reason why high APGAR scores might not correlate to the baby’s outcome is the potential for bias and subjectivity. Most of the time, the medical professional calculating the APGAR score is also involved in the delivery. As such, there is potential for bias to providing a higher score.
It is common in medical malpractice cases where doctors assign high APGAR scores that contradict clear cut evidence of injuries. Therefore, while the APGAR score is an important marker, parents should understand there is a high error rate.
It is possible for medical professionals to improperly analyze and treat a baby with one or more low scores. Without timely treatment, medical conditions can worsen, lead to the potential of hypoxic-ischemic encephalopathy (HIE) and other conditions will lead to cerebral palsy and cognitive disabilities.
Is Your Child’s Birth Injury the Result of Medical Malpractice?

The parents of children who suffered birth injuries often want answers. Many times parents see evidence at birth, including low Apgar scores, that their baby suffered a complication during labor. They want to know what happened to harm their child. Were there signs of fetal distress that the doctors and nurses failed to recognize and/or failed to respond to in a timely manner? Was a c-section not performed as early as it should have been or not performed at all?
Our dedicated birth injury lawyers want to help you find those answers.
We diligently investigate the facts, including a detailed examination of the fetal heart rate monitoring strips and labor and delivery records. We look closely at the Apgar scores and all of the surrounding evidence to determine the validity of these scores.
If this review shows the medical providers did not diagnose or respond to fetal distress, we hold responsible parties accountable by pursuing medical malpractice claims against them. The compensation our clients receive helps them pay for their child’s current and future medical treatment, assistive technology and equipment, attendant care, and the other expenses associated with caring for a child with brain injuries, seizure disorders, and cerebral palsy.
Sometimes families are afraid to talk to lawyers about their child’s case because they worry there is a fee. There is never a fee unless and until we make money recovery for our clients.
What Is the Statute of Limitations in a Birth Injury Lawsuit?
A statute of limitations (SOL) is a law that sets a time limit on how long an injured person has to file a lawsuit after an accident. It is essential to understand that statutes of limitations vary based on the case and the state where you file. For instance, the deadline for birth injury claims is typically different from other claims, such as injury to private property.
Generally, the clock starts ticking on the date the injury occurred. However, there are exceptions to this rule. In some cases, the statute of limitations starts when a person discovers or reasonably should have discovered an injury. When dealing with government agencies, SOLs can become even more complex.
For example, if the party that injured you was:
- A federal employee
- Employed by a military hospital, Veterans Administration facility, or a federally funded medical entity
You may need to file a birth injury claim under the Federal Tort Claims Act (FTCA). In FTCA cases, claimants must go through certain administrative procedures before filing a lawsuit. In some states, you may have less time to give notice if:
- The negligent party was a local or state government hospital.
- The doctors and medical providers are employees of a governmental entity.
If you file your case outside of the statute of limitations, the court will typically dismiss it. This means you will not be eligible to recover compensation for you or your child’s injuries. Determining when a statute of limitations begins on your case can be tricky. If you are considering pursuing compensation for a birth injury, contact an attorney as soon as possible.
How Can Our Birth Injury Attorneys Help You?

Low APGAR scores are not always preventable, but medical errors and improper delays in lifesaving treatment are. It takes an expert review of the facts of your birth to determine whether medical professionals mismanaged your child’s delivery.
At Miller Weisbrod Olesky, our team of committed birth injury attorneys, nurses and paraprofessionals works to answer these questions and seek compensation. We use our detailed medical negligence case review process to assess your potential birth injury case.
We start by learning more about you and your child and the status of meeting/missing developmental milestones. We then gather medical records to determine what happened before, during, and after your premature birth. This includes a detailed review of the treatment doctors provided, or the treatment doctors failed to provide. Failing to administer hypothermia therapy can count as medical malpractice when it leads to avoidable future diagnoses like cerebral palsy.
We will call in skilled medical experts who review your records and provide insight into where medical professionals went wrong. If we feel medical negligence caused or contributed to your child’s low APGAR score, we meet with you to discuss.
At no point in our legal intake process will we ask you to pay anything. The medical review of your case and the consultation are free. We only receive payment when you do. The sooner you reach out, the sooner we can investigate your case and gather the evidence to support your claim.
We work on a contingency fee basis, meaning you won't pay any legal fees unless we win your case. Contact us today to schedule your free consultation by calling our toll-free line at (888) 987-0005. You can also reach us by filling out our online request form.
Contact Miller Weisbrod Olesky
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.
