Placenta Previa
What is Placenta Previa?
Placenta previa is a medical condition that may occur during pregnancy when the placenta fully or partially covers the cervix (the uterus opening). In normal conditions, the placenta is attached to the top of the inner uterine walls, but with placenta previa, it attaches lower.
The condition can usually be diagnosed early during the pregnancy with an ultrasound exam. Some patients with undiagnosed placenta previa may experience painless vaginal bleeding and visit the ER during the second or third trimester.

When an expectant mother has placenta previa, it may cause the blood vessels connecting the placental tissue to the uterus to tear at the time of labor or delivery. This can cause severe bleeding which will result in fetal distress if not immediately addressed with an emergency c-section.
Placenta previa can even cause severe bleeding after birth endangering the life and welfare of the mother if the bleeding is not stopped.
What Causes Placenta Previa?

Placenta Previa Risk Factors
According to the available data, up to 2% of pregnancies in the third trimester are affected by placenta previa. With that said, researchers have not identified the exact underlying causes of this condition. There is some evidence of an association between uterine scarring and endometrial damage. Some of the known risk factors for placenta previa include:
- Advanced maternal age (over 35 years)
- Previous childbirths (multiparity)
- History of c-section(s)
- History of placenta previa
- Use of in-vitro fertilization
- Multiple birth (pregnant with twins, triplets, or quad)
- Previous internal reproductive organ surgery, such as D&C (dilation and curettage) or myomectomy (removal of uterine fibroids)
- Use of tobacco, cocaine, or other substance use
Diagnosing Placenta Previa

Routine ultrasound exams in the first and second trimester usually help medical providers detect placenta previa. It’s noteworthy that the earlier during the pregnancy placenta previa has been present, the greater are the chances that it will resolve on its own. About nine out of 10 “low lying” placenta conditions will naturally resolve by the third trimester. Nevertheless, Obstetricians and Maternal Fetal Medicine specialists should always order follow-up ultrasound exams at 28 to 32 weeks gestation to identify unresolved or persistent placenta previa.
When an expectant mother presents with painless vaginal bleeding during the second or third trimester of pregnancy, the doctor or nurse should take care to avoid a digital (use of fingers) vaginal examination until a transabdominal ultrasound has been conducted. This is because a finger could accidentally cause damage to the placenta or uncontrolled bleeding. If the provider suspects the occurrence of placenta previa after this ultrasound test, they should order a transvaginal ultrasound to determine the precise location of the placenta.
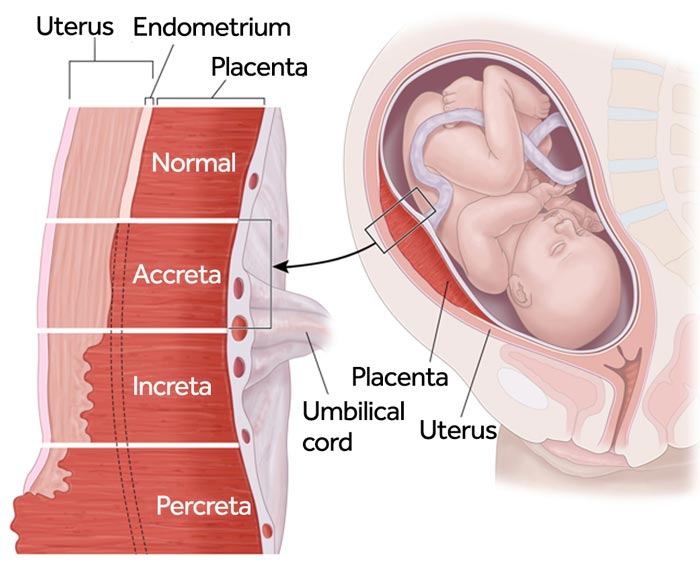
At the time of ultrasound examination, the medical team must also evaluate the patient for placenta accreta spectrum (PAS). Medical providers should suspect PAS when placenta previa is diagnosed, and keep this as an important consideration during follow-up tests and management of the condition. PAS covers a range of placental pathologies, including: (a) placenta accreta; (b) placenta increta; and (c) and placenta percreta.
In all these three conditions, the placenta remains fully or partially attached at the time of childbirth, which may cause major blood loss during or after delivery.
- Placenta Accreta: This condition develops when the placenta grows excessively deep into the uterine wall and beyond the normal myometrium boundary (the muscular external layer of the uterus).
- Placenta Increta: This condition occurs when the placenta gets even more firmly and deeply attached to the uterus, invades the myometrium, and eventually gets embedded in the outer muscular wall.
- Placenta Percreta: In this condition, the placenta invades the uterine serosa (the tissue layer coating the outside of the uterus). As a result, the placenta extends beyond the uterus and possibly invades surrounding organs (such as the bladder).
Placenta accreta spectrum (PAS) may result in massive hemorrhage. Therefore, the medical providers must have an integrated team strategy in place prior to the delivery. PAS diagnosis with ultrasound offers high specificity and sensitivity. But when potential bladder invasion is suspected, an MRI exam may be useful.
When PAS is highly suspected, the medical provider should discuss with the expectant mother a plan for cesarean hysterectomy (full uterus removal at the time of cesarean delivery). The goal in this case is to leave the placenta in situ (in its original position) in order to prevent massive hemorrhage.

Birth Complications caused by Placenta Previa
Placenta previa may cause serious complications that endanger the safety of the mother and the baby. Some of the key placental complications may include:
Massive Hemorrhage
Massive hemorrhage (severe, life-threatening vaginal bleeding) is the biggest risk of placenta previa. Bleeding usually occurs in the third trimester in these cases as the lower portion of the uterus thins during this period. Studies have shown that 52% of expectant mothers with this condition experience antepartum (pre-delivery) hemorrhage, while 22% may have postpartum (post-delivery) hemorrhage.
Excessive bleeding can cause “shock” which will put both the mother and the baby at high risk for catastrophic injury or even death.
Premature Birth
Severe vaginal bleeding due to placenta previa may necessitate an emergency cesarean delivery before the baby has reached full term. Nearly 15% of expectant mothers with placenta previa will deliver before the 34th week of pregnancy. This increases the baby’s risk of preterm birth related complications, such as fetal distress due to lack of oxygen or hypoxic-ischemic encephalopathy (HIE), which could lead to cerebral palsy.
Placenta Accreta Spectrum (PAS)
PAS is a likely complication in expectant mothers with placenta previa. PAS occurs when the placenta gets deeply attached to the uterine wall, making it difficult to detach at the time of delivery. To avoid the risk of hemorrhage (which may occur while removing the placenta in this condition), the medical team may perform hysterectomy (uterus removal). PAS also increases the baby’s risk of fetal hypoxia, HIE, and cerebral palsy.
Placental Abruption
Placenta previa can sometimes cause the tearing of the placental tissue, which increases the risk of placental abruption (separation of the placenta from the inner uterine wall). In some cases, no visible bleeding may occur because the blood could get trapped within the uterus. Placental abruption may cause oxygen deprivation for the baby, possibly resulting in HIE. Electronic fetal heart monitoring (EFHM) may show non-reassuring fetal heart rate patterns.
How does Maternal Hemorrhage Harm the Baby?
If there is a delay in the diagnosis of placenta previa or the medical providers fail to perform an emergency cesarean section in a case of severe placenta previa, the mother is at a risk of massive hemorrhaging. Severe bleeding not only threatens the mother’s life, but may also result in serious birth injuries for the baby. According to researchers, placenta previa is the single most common placenta-related cause of neonatal anemia.

In placenta previa patients, neonatal anemia along with premature birth is a major risk factor (4 to 8% risk) of perinatal mortality (baby’s death around the time of labor and delivery). The baby is also at a risk of fetal hemorrhage if the mother hemorrhages because the baby’s source of blood is through the umbilical cord.
In case of a fetal hemorrhage, the baby may experience a hypovolemic shock, resulting in loss of oxygenated blood supply to the brain. This can lead to birth asphyxia or hypoxic-ischemic encephalopathy, which may eventually cause cerebral palsy.
Placenta previa is also associated with lower APGAR scores, low birth weight, and intrauterine growth restriction (IUGR), which is another important risk factor for perinatal mortality. This can happen because in placenta previa, the lower uterine portion receives less blood supply. Moreover, fetal growth may also be affected because of repeated episodes of vaginal bleeding.
Relationship between Placenta Previa & Cerebral Palsy
A research study showed the correlation between vaginal bleeding in expectant mothers with placenta previa and cerebral palsy. Researchers reviewed 60 babies born to mothers diagnosed with placenta previa. Preterm deliveries occurring before 26 weeks of pregnancy and cases of placenta accreta were excluded from the study.
Researchers measured for two possible outcomes: occurrence of cystic periventricular leukomalacia (PVL) and cerebral palsy. Results showed that 5 babies had PVL, out of which 4 babies developed cerebral palsy. Massive and acute bleeding (more than 500 ml within 8 hours) occurred in these cases at around 30 to 31 weeks gestation, leading to emergency c-section delivery.
The researchers concluded that placenta previa related massive hemorrhage at around 30 to 31 weeks of pregnancy could be a risk factor for cerebral palsy. Close neonatal follow-up is required in these cases.
Preventing Placenta Previa Birth Complications
A multidisciplinary team approach should be adopted when placenta previa is diagnosed through ultrasound or when the patient presents with painless vaginal bleeding. Bed rest, avoiding digital examinations, and avoiding sexual intercourse are recommended because any form of manipulation of the placenta may cause hemorrhage.
The medical providers should review the patient’s history of cesarean sections or a previous diagnosis of placenta previa because these factors can increase the risk of PAS. An expectant mother diagnosed with placenta previa should be informed about the possible management strategies and expectations. She should be advised to visit the ER if she has an episode of vaginal bleeding.
The medical team should obtain the patient’s consent for potential blood transfusions (multiple transfusions may be required in case of hemorrhage). They should also obtain the patient’s consent for possible cesarean hysterectomy (uterus removal) and uterine artery embolization (removal of uterine fibroids).

Each member of the inter-professional team should be aware about the patient’s condition. These may include labor & delivery physicians, interventional radiologist, anesthesiologist, urology surgeon, vascular surgeon as well as neonatal and surgical nurses.
Examples of Medical Negligence in Placenta Previa Cases
- Failure to diagnose placenta previa early through sonography.
- Failure to educate the expectant mother diagnosed with placenta previa about avoiding intercourse, aggressive exercises, and travel.
- Performing a digital examination (pelvic examination) when placenta previa is suspected, resulting in severe vaginal bleeding.
- Performing a vaginal delivery even when placenta previa remains unresolved.
- Failure to plan for or perform a timely emergency cesarean section.
- Failure to monitor the expectant mother to identify any changes in placenta previa or development of placental complications, such as PAS.
- Failure to monitor the baby during pregnancy, labor and delivery or in the event of massive hemorrhage, resulting in fetal hypoxia, seizures, HIE, cerebral palsy, or fetal mortality.
- Failure to identify or manage placenta previa complications, such as placental abruption or PAS.
Is Your Child’s Placenta Previa Related Birth Injury or Complication the Result of Medical Malpractice?
Parents whose children suffer from placenta previa related birth injury or birth complications want and deserve answers as to the cause of their child’s injury and whether mistakes by the doctors and nurses contributed to the injury.
Were there signs of placenta previa during the pregnancy, labor, and delivery process, or presence of risk factors such as advanced maternal age, prior cesarean sections, or history of placenta previa, which were either not recognized or properly treated? Did the medical team fail to order a series of ultrasound monitoring tests to diagnose suspected placenta previa in a timely manner? Was the decision to perform a cesarean delivery delayed?
During the labor and delivery, were there clear indications that the baby was suffering from fetal distress, but appropriate actions were not taken by the obstetrician or nurses? Did the neonatal resuscitation team delay in providing important breathing support after birth? Were serious neonatal conditions like fetal hypoxia, hypoglycemia, or jaundice missed or treated incorrectly?
The experienced birth injury lawyers at Miller Weisbrod Olesky will help you determine if mistakes of the medical providers caused a birth injury to your child. Our hard working and successful birth injury attorneys have represented families all over the United States in their time of need after a birth injury. We use our experience and expertise to obtain for you and your child a medical malpractice settlement that will help provide specialized medical therapy in order to maximize the quality of life and independence of your child throughout their life.
Sometimes families are reluctant to contact a medical malpractice lawyer. It’s also not uncommon for parents to feel overwhelmed by the responsibilities they encounter in caring for their injured child and worried that they will not be able to help out in a lawsuit involving their child’s birth injury. Our birth injury attorneys and nursing staff will address these hesitations and concerns, so you can focus on your child and maximizing their care.
Registered Nurses and Nurse-Attorneys Are a Vital Part of Our Birth Injury Team…and Yours

Most national birth injury law firms will employ one or two nurses to assist the review of cases and medical research. But Miller Weisbrod Olesky offers an unmatched number of nurses and nurse-attorney employees support to both the birth injury attorneys and our clients.
Our team of registered nursing staff and nurse-attorneys bring a deep level of medical and personal insight to every client’s case. Our nursing team includes both an experienced labor and delivery nurse as well as an ICU nurse. Working closely with the rest of the team, they investigate the reasons behind a birth injury and how medical professionals breached their standard of care.
Why Should You Talk with the Knowledgeable Attorneys at Miller Weisbrod Olesky?

The only way to find out if you have a birth injury case is to talk to a lawyer experienced in birth injury lawsuits. It’s not uncommon that a birth related complication results in a preventable birth injury, including cerebral palsy, but it takes a detailed expert review by a birth injury attorney of the medical records from your child’s birth to determine if the birth injury was the result of medical malpractice.
At Miller Weisbrod Olesky, a team of committed lawyers, nurses and paralegals uses our detailed medical negligence case review process to assess your child’s potential birth injury case. We start by learning more about you and your child and the status of meeting/missing developmental milestones. Then we gather medical records to determine what happened before, during, and after your delivery. We call in skilled medical experts who review your records and let us know if they think medical errors could have caused your child’s injuries.
If we feel medical negligence caused or contributed to your child’s injuries, we meet with you to discuss how you can receive compensation from the medical professionals who made the errors. Our birth injury attorneys have recovered millions of dollars in settlements for families of children that have suffered a birth injury.
At no point in our legal intake process will we ask you to pay anything. The medical review of your case and the consultation are free. We only receive payment when you do.
Contact Our National Birth Injury Lawyers
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.