Neonatal Sepsis
Sepsis During and After Pregnancy
When an expecting mother or newborn child go into sepsis, it is a life-threatening emergency that requires urgent medical attention. Symptoms can begin suddenly as inflammation and the infection spreads through the bloodstream.

Anyone who has contracted an infection is at risk of developing sepsis. Newborn babies are at a higher risk because of their underdeveloped immune systems at birth. An expecting mother may be at risk for sepsis during her pregnancy, during labor and delivery, or even after birth.
Newborns can sustain devastating birth injuries if the inflammation from sepsis reaches their brain. When this happens, the child is at high risk for blood clots, and brain injuries like hypoxic-ischemic encephalopathy (HIE). HIE is the leading cause of cerebral palsy and can cause irreversible developmental delays.
Healthcare providers must act quickly when they recognize the initial signs of a septic reaction. Even slightly delayed responses can have fatal consequences. Healthcare professionals commit medical malpractice when they miss or mistreat neonatal infections and fail to identify the onset of sepsis.
Birth Injury Malpractice Attorneys
Our top rated birth injury attorneys specialize in identifying how mismanaged neonatal infections can lead to severe septic reactions. If your baby suffered from sepsis during delivery or after birth, don’t hesitate to contact our firm. We can answer difficult legal and medical questions and investigate the facts on your behalf.
Free Legal Consultation
Birth Injury Lawyers
(888) 987-0005Our Birth Injury Lawyers are available to meet you in your home or the hospital.
Our vast network of medical experts and in-house nursing staff and nurse-attorneys gives us the edge over our competition. When we take your case, we assign you with not just an attorney but an entire medical team. This team includes attorneys, experienced nursing advocates, and seasoned medical experts.
Your team is available to assist with any day-to-day treatment you or your child may need. This includes assistance with obtaining medical records, scheduling doctors’ appointments, providing transportation, and any other problems that may arise.
We offer all of this on a contingency fee basis. This means you will not pay any fees until after we win your case and secure a settlement. Miller Weisbrod Olesky’s unmatched track record of birth injury results sets us apart from other birth injury law firms.

Recent Birth Injury Settlement:
Birth Injury settlement against a hospital in which nurses and physicians failed to properly monitor the mother's blood pressure during delivery causing an HIE event resulting in neonatal seizures and cerebral palsy at birth. Our team of top-rated birth injury lawyers recovered $13,750,000 for the family to help with future medical expenses and developmental therapy.
What Is Sepsis?

Sepsis is an extreme bodily reaction to an infection. It starts with widespread inflammation that travels through the bloodstream and triggers fever-like conditions and even seizures in patients.
Sepsis can come on suddenly and rapidly progress to the point of causing permanent damage within hours. The CDC estimates that nearly 1.7 million American adults go into severe sepsis annually from infections. They estimate that more than 75,000 newborns develop the condition each year in the United States. One estimate from The University of Florida Health Center claims that more than 18 infants die from sepsis each day.
What Causes Sepsis During Pregnancy?
Maternal infections and neonatal infections trigger the immune system to respond by producing proteins, antibodies, and white blood cells.
These immune system components travel through the bloodstream to find the infection and attack it, which causes inflammation. Inflammation is what causes swelling, redness, pain or tenderness, and excess warmth around an infected area.
While inflammation can feel uncomfortable, it is a part of the body’s natural healing process. It usually is a sign that the immune system is doing its job.

Sometimes, however, the body’s immune system creates too many infection-fighting proteins (called cytokines). This causes widespread and unnecessary inflammation throughout the body and bloodstream. This can result in blood clots, tissue damage, organ dysfunction and failure, seizures, and even death.
What’s The Difference Between Sepsis and Septicemia?
Septicemia (blood poisoning) is the name of an infection that occurs when harmful bacteria enter the bloodstream. Septicemia can trigger sepsis, but the two terms are not interchangeable.
It’s important to remember that sepsis isn’t actually an infection, but rather a widespread bodily response to an infection. While almost all cases of septicemia lead into sepsis, septicemia is not always the cause of sepsis.
What Factors Increase the Risk for Sepsis?
Expecting mothers and newborns who have an underlying infection are at the highest risk for going into sepsis. Two of the most common infections that can trigger sepsis are Group B Streptococcus and Escherichia coli (E. Coli). However, it’s important to know that sepsis is more commonly for expecting mothers after pregnancy than during it.
A number of factors can increase the risk for contracting infections that can develop into sepsis:
Advanced Maternal Age

As people age, their immune system naturally weakens. Immunosenescence has stronger effects later in life (around age 60), but the process begins in early adulthood.
Expecting mothers on the later end of their reproductive years (ages 35+) may experience a greater immune system deficiency. This can increase their risk for a septic reaction from infections during and after pregnancy.
On the other side of things, newborns have the opposite problem. Their risk for sepsis increases because of their early age and underdeveloped immune systems.
Pregnancy Complications

A mother may have a weakened immune system for other reasons beyond age. Certain autoimmune disorders like gestational diabetes, rheumatoid arthritis or ulcerative colitis can cause excess inflammation in the body. This can increase a mother’s risk for going into sepsis whenever she contracts an infection.
Other conditions, such as lung and heart diseases and various types of cancer, can also diminish immune system function. This may sometimes serve as a catalyst for contracting a septic infection.
Extended Hospital Stay
A mother and her child’s risk for contracting infections increases the longer they stay in the hospital. Some babies have extended hospital stays in the neonatal intensive care unit (NICU). They may contract infections from unsterilized hospital equipment, interactions with other sick patients, or contact with infected healthcare workers.
C-Section Deliveries

When a mother requires a C-section delivery, there is a moderate risk for infection at or near the incision site. Any additional wounds or tears from the procedure may also collect bacteria and increase her risk for sepsis.
Invasive Medical Devices

Invasive medical devices like catheters, breathing and feeding tubes, and IVs can provide an entry point for infections. Mothers and newborns who need these devices may have a heightened risk for an infection that can develop into sepsis.
Healthcare professionals must identify these risks when they are present in expecting mothers or their newborns. They must take all necessary precautions to prevent infections from developing into a case of sepsis.
What Are the Early Warning Signs of Sepsis During Pregnancy?
Sepsis can be difficult to identify in the early stages because it starts out looking like a typical bodily reaction.

Sepsis is unique, however, in the sense that it is a systemic response to a localized issue. Instead of inflammation happening only at the infection site, the entire body reacts. This can have dire effects on the mother or her newborn, especially if it progresses into a more severe stage.
What Are the 3 Stages of Sepsis?
Sepsis has multiple stages, with each stage categorized by the onset of different symptoms:
STAGE ONE: Sepsis
In the beginning stages, the mother or newborn will often have a fever with chills and elevated heart rates (tachycardia). The inflammation in the bloodstream can cause low blood pressure and body aches. Treatment is most effective during this stage for avoiding long-term harm for the mother or her baby.
STAGE TWO: Severe Sepsis
Sepsis can develop into a severe case within a day or even multiple hours when left untreated or insufficiently treated. When a mother or newborn develops severe sepsis, they may begin to experience organ dysfunction.
Body aches will intensify into extreme pain, and blood pressure may drop even further below safe levels.
Strong changes in mood and mental ability may also occur, such as lethargy and confusion. This can be an indication that the inflammation is starting to reach the mother’s or baby’s brain.
STAGE THREE: Septic Shock
Septic shock is the final and most severe stage of sepsis. A mother or newborn going into septic shock is at risk for organ failure and death.
Septic shock can cause body convulsions, extremely low blood pressure, seizures and strokes, respiratory distress, and organ failure. In the most extreme cases, septic shock can cause maternal mortality or infant death.
A mother or newborn in septic shock will receive treatment in the intensive care unit or neonatal intensive care unit. Nearly a third of patients don’t survive septic shock, even when they receive timely treatment.
| SYMPTOM | STAGE OF SEPSIS |
|---|---|
| Fever | STAGE ONE (Sepsis) |
| Chills | STAGE ONE (Sepsis) |
| Elevated Heart Rate | STAGE ONE (Sepsis) |
| Low Blood Pressure | STAGE ONE (Sepsis) |
| Body Aches | STAGE ONE (Sepsis) |
| Rash | STAGE ONE (Sepsis) |
| Decreased Urine Output | STAGE ONE (Sepsis) |
| Mental Decline | STAGE TWO (Severe Sepsis) |
| Extreme Pain | STAGE TWO (Severe Sepsis) |
| Respiratory Distress | STAGE TWO (Severe Sepsis) |
| Slurred Speech | STAGE TWO (Severe Sepsis) |
| Extreme Lethargy/Listless | STAGE TWO (Severe Sepsis) |
| Lung Failure | STAGE THREE (Septic Shock) |
| Heart Failure | STAGE THREE (Septic Shock) |
| Kidney Failure | STAGE THREE (Septic Shock) |
| Convulsions | STAGE THREE (Septic Shock) |
| Seizures | STAGE THREE (Septic Shock) |
| Stroke | STAGE THREE (Septic Shock) |
| Death | STAGE THREE (Septic Shock) |
Symptoms of Sepsis by Stage
It’s important to note that as sepsis progresses, symptoms from earlier stages can still be present and intensify. Healthcare professionals must swiftly identify these symptoms (especially in the early stages) to avoid permanent injuries.

Sepsis in Newborns: Early-Onset Vs. Late-Onset
A newborn can develop early-onset sepsis if they contract an infection at birth from the mother (known as a congenital infection). This is more common in premature infants.
A newborn’s case of sepsis is late-onset if they contract the infection after delivery in the hospital. This is more common in babies with birth complications like low birth weight, or feeding through a G-tube. Babies with birth complications will usually stay longer in the neonatal intensive care unit, which can increase their risk.
Early-onset sepsis will occur within the first few days of life. Late-onset sepsis can occur from a week after birth up until the 28th day of life. Medical professionals treat both types using the same methods.
How to Identify and Treat Sepsis?

Healthcare providers must act with urgency when treating mothers and newborns suspected of undergoing sepsis. In 2006, a UK-based nonprofit called The Sepsis Trust coined “The Sepsis Six”. this is a bundle of medical treatment actions that healthcare professionals can take to reduce the risk of mortality from sepsis.
The Sepsis Six
- Taking blood cultures
- Starting intravenous (IV) antibiotics
- Starting intravenous (IV) fluids
- Providing high-flow oxygen
- Measuring serial serum lactate levels
- Measuring urine output
In addition to blood and urine tests, healthcare providers may also deem it necessary to run x-rays or CT scans. This is to monitor the effect sepsis has already taken on the body. They must also check the mother or child’s vital signs (blood pressure and respiratory rates) to check for any abnormalities.
Doctors should immediately administer antibiotics, oxygen, and fluids to a patient in suspected sepsis. Doctors may prescribe vasopressor medications to tighten the blood vessels for patients with a dangerously low blood pressure. The mother or child may require surgery later to remove damaged organ tissue.
The standard of care is to begin treatment before receiving the results of the blood and urine tests. This is because waiting for results to come back can take time that suffering mothers and newborns cannot afford.
Blood and urine cultures can also return false-negative results sometimes. This can happen when a viral infection causes sepsis instead of a bacterial one. Because of this, it is also standard for healthcare providers to test the mother or newborn for common viral infections. This includes widespread seasonal infections like influenza and COVID-19.
How Can Medical Professionals Mismanage Sepsis Cases?
The severity of sepsis makes it critical for doctors, nurses, and specialized healthcare teams to act quickly and competently. Examples of medical negligence when treating sepsis can include:
- Missing or failing to treat a maternal infection or neonatal infection that progresses into sepsis.
- Making an improper incision or would during a C-section delivery that causes a septic infection.
- Failing to recognize the signs of sepsis in time before it progresses.
- Failure to identify a case of viral sepsis due to a negative blood or urine culture.
- Delaying treatment of a suspected sepsis case until positive culture results come back.
- Failure to administer the proper antibiotics or sufficient fluids to the mother or newborn.
- Failure to remove damaged tissue following a case of sepsis.
It requires a detailed review of the facts and timeline of a sepsis case before determining whether medical malpractice occurred. A specialized birth injury attorney can investigate the role medical errors played in the mother’s or child’s sepsis-related birth injury.
Frequently Asked Questions About Sepsis During Pregnancy
What’s The Difference Between Sepsis and Septicemia?
Septicemia (blood poisoning) is the name of an infection that occurs when harmful bacteria enter the bloodstream. Septicemia can trigger sepsis, but the two terms are not interchangeable.
It’s important to remember that sepsis isn’t actually an infection, but rather a widespread bodily response to an infection. While almost all cases of septicemia lead into sepsis, septicemia is not always the cause of sepsis.
What Are Six Signs of Sepsis?
A mother or newborn can show multiple signs of sepsis; there aren’t necessarily six characteristics that define each sepsis case. In 2018, the nonprofit organization Sepsis Alliances launched It’s About TIME. Their campaign aims to promote early detection of sepsis using the T.I.M.E. acronym to identify symptoms:
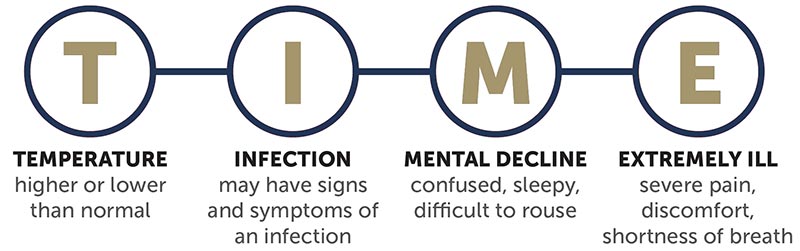
- T – Temperature (higher or lower than normal)
- I – Infection (signs or symptoms of an infection)
- M – Mental Decline (confusion, tiredness, etc.)
- E – Extremely Ill (severe pain, discomfort, shortness of breath)
In recent years, some researchers have tested out a new 6-part mnemonic S.E.P.S.I.S., but experts debate its effectiveness.
How Long Does Sepsis Have To Become Fatal?
Sepsis can become fatal in as short as 12 hours. However, it depends on numerous factors:
- the mother or newborn’s underlying conditions
- the severity of the initial infection that caused sepsis
- and how quickly medical professionals started treatment.
For newborns, the risk of death increases by about 7.6% with every hour that passes without treatment.
What Does a Sepsis Rash Look Like?
Sometimes, a blood infection called septicemia can cause a mother or newborn to go into sepsis. Septicemia often comes with a reddish, discolored skin rash around the infected area or even around the entire body.
Is Sepsis Contagious?
Sepsis is not contagious. It is a bodily response to an infection. However, the infection that causes a mother’s or newborn’s case of sepsis can be contagious. Whether or not that same infection will induce a septic response in someone else can depend on their risk factors. This includes their age, their underlying health conditions, and how long the infection goes untreated in their body.
Can You Get Sepsis From a Tooth Infection?
Yes, you can go into sepsis from a tooth infection. Bacterial infections can sometimes cause a tooth abscess, a pocket of pus that forms in the gums. It’s very easy for these infections to enter the blood stream and cause septicemia. Septicemia is a serious blood infection that can develop into sepsis when mismanaged or left untreated.
Can Sepsis Reoccur?
Yes, sepsis can reoccur. In fact, patients who have survived a septic episode have an increased risk of it happening again from future infections.
Did Doctors Mistreat My Child’s Neonatal Sepsis?

While sepsis can be life-threatening, a mother or her newborn can survive it without any permanent injury. Their prognosis dramatically improves when they receive quick and proper medical treatment.
Medical negligence, such as a misdiagnosis or missing early symptoms an infection, can worsen a mother’s or newborn’s health. A newborn who goes into sepsis may suffer from preventable birth injuries and birth complications like organ failure and death.
If a family believes medical negligence worsened a child’s neonatal infections, legal support may be an option. A specialized birth injury attorney can review the medical records and circumstances to assess whether a claim exists.
Families who have experienced the effects of septic reactions from negligent medical care deserve to know whether they were avoidable. Our top rated birth injury lawyers will help you find those answers and obtain the necessary funds to secure treatment.
Our National Birth Injury team will thoroughly investigate the facts, holding responsible parties accountable by pursuing medical malpractice claims.
What is the Statute of Limitations in a Birth Injury Lawsuit?
A statute of limitations (SOL) is a law that sets a time limit on how long an injured person has to file a lawsuit after an accident. It is essential to understand that statutes of limitations vary based on the case and the state where you file. For instance, the deadline for birth injury claims is typically different from other claims, such as injury to private property.
Generally, the clock starts ticking on the date the injury occurred. However, there are exceptions to this rule. In some cases, the statute of limitations starts when a person discovers or reasonably should have discovered an injury. When dealing with government agencies, SOLs can become even more complex.
For example, if the party that injured you was:
- A federal employee
- Employed by a military hospital, Veterans Administration facility, or a federally funded medical entity
You may need to file a birth injury claim under the Federal Tort Claims Act (FTCA). In FTCA cases, claimants must go through certain administrative procedures before filing a lawsuit. In some states, you may have less time to give notice if:
- The negligent party was a local or state government hospital
- The doctors and medical providers are employees of a governmental entity
If you file your case outside of the statute of limitations, the court will typically dismiss it. This means you will not be eligible to recover compensation for you or your child’s injuries.
Determining when a statute of limitations begins on your case can be tricky. If you are considering pursuing compensation for a birth injury, contact an attorney as soon as possible.
How Can Our Birth Injury Attorneys Help?

Doctors can sometimes prevent neonatal sepsis by taking quick action in treating bacterial and viral infections. However, it takes an expert review of the facts of your birth to determine whether medical professionals made preventable errors.
Our Process
Our team of committed attorneys, nurses and paraprofessionals works to answer these questions and seek compensation. We use our detailed medical negligence case review process to assess your potential birth injury case.
We start by learning more about your pregnancy by gathering records to determine what happened during and after your delivery. This includes evaluating the fetal heart rate strips during labor and blood culture and urine testing procedures after birth.
We will call in skilled medical experts who review your records and provide insight into where medical professionals went wrong. If we feel medical negligence caused or worsened your baby’s neonatal infection, we meet with you to discuss further.
At no point in our legal intake process will we ask you to pay anything. The medical review of your case and the consultation are free. We only receive payment once you do. The sooner you reach out, the sooner we can investigate your case and gather the evidence to support your claim.
We work on a contingency fee basis, meaning you will not pay any legal fees until we win your case. We do not purse any medical malpractice cases unless we fully believe we can win.
Contact us today to schedule your free consultation by calling our toll-free line at (888) 987-0005. You can also reach us by filling out our online request form.
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.