HELLP Syndrome
What is HELLP Syndrome?
HELLP Syndrome is a rare but dangerous medical condition that affects a small percentage of pregnant women. When HELLP Syndrome develops during pregnancy is poses high risks to both the health and life of not only the mother, but the baby as well.
HELLP Syndrome is a medical condition that affects the blood and liver. HELLP has historically been classified as a severe form of preeclampsia *(gestational high blood pressure complication accompanied by protein in the urine or proteinuria). Based on this, in recent years, some researchers have suggested that HELLP syndrome is an independent condition on its own.
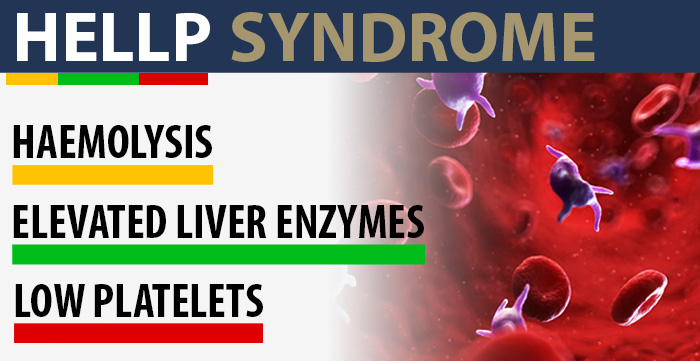
HELLP stands for the three characteristics of the disease, namely:
- H – Hemolysis: It is the destruction or rupture of red blood cells (RBCs). RBCs perform the critical role of transporting oxygen from the lungs to various parts of the body.
- EL – Elevated Liver Enzymes: High levels of liver enzymes in the bloodstream may indicate damage or inflammation of the cells in the liver (which triggers the leakage of these enzymes).
- LP – Low Platelet Count: Platelets are a vital blood component that helps in clotting. Low platelet count or thromobocytopenia may indicate that the body is rapidly destroying an abnormally high number of platelets.
What is Hellp Syndrome During Pregnancy?
HELLP syndrome occurs in about one percent of all pregnancies. But in women with severe preeclampsia, about 10 to 20 percent of them will have HELLP syndrome. In about 70 percent of the cases, the condition develops in the third trimester of pregnancy (starting around gestational week 28).
In some cases, the condition may occur in the mother as late as two to seven days after childbirth (known as postpartum preeclampsia). HELLP is a medical emergency requiring urgent treatment. In absence of timely or appropriate treatment, about 25 percent of the women with HELLP will develop serious complications, and a small number of them will even die due to HELLP.

What Causes HELLP Syndrome?
While there is a significant overlap between women with preeclampsia and those who develop HELLP syndrome, the correlation between the two is not as obvious as it was once thought to be. Researchers now believe that maternal and fetal genetic mutations as well as immunological (related to the immune system) factors may have a role to play in the development of HELLP syndrome.
Early onset of HELLP before 28 weeks gestation occurs in about 20 to 30 percent of the cases. This is typically associated with rapid and severe onset of the disease with symptoms that are likely to coexist with intrauterine growth restriction (IUGR) of the baby.
Pregnant women at risk for developing HELLP include women that suffered from preeclampsia in earlier pregnancies. Also, though there has been no scientific answer to this, most women that develop HELLP are Caucasian vs. other ethnicities and most women are over the age of 25.
What are Symptoms of HELLP Syndrome?

Although some pregnant women will develop HELLP syndrome suddenly without any prior symptoms, in most cases, the following signs and symptoms may appear:
- Discomfort, headache, or extreme fatigue
- Persistent or worsening nausea and vomiting
- Pain in the chest or the upper part of the abdomen
- Blurry vision
- Rapid weight gain and swelling in the limbs
- Nosebleeds or bleeding from a wound that won’t stop
- Seizures or convulsions (rare symptom)
How To Diagnose HELLP Syndrome During Pregnancy?
Variability of symptoms, similarity of the symptoms to other conditions, and the lack of consensus among doctors can lead to delayed diagnosis or misdiagnosis of HELLP syndrome. The three major diagnostic criteria in pregnant women suspected to have this condition include the following prenatal tests:

- Blood Smear Test: It will usually reveal abnormalities, such as burr cells (red blood cells with spikes on the surface), schistocytes (irregular fragmented parts of RBCs), and helmet cells (indicating cell membrane damage).
- Complete Blood Count (CBC) Test: Low platelet count or gestational thrombocytopenia is the earliest indication seen in all patients with HELLP syndrome. This is determined with a CBC test.
- Liver Function Test (LFT): A complete metabolic panel will include several liver function tests to assess elevated enzyme and protein levels in the liver, which may indicate hepatic (liver) dysfunction.
Other less conclusive diagnostic parameters for HELLP syndrome used in conjunction with the primary clinical diagnostic criteria include:
- Systolic and diastolic blood pressure measurement to identify de novo (new) manifestation of maternal hypertension
- Urinalysis to identify elevated levels of proteins, leucocytes and uric acid concentrations
- Low hemoglobin and haptoglobin (proteins in blood plasma) levels
- High bilirubin levels (yellowish pigment in the blood) indicating liver damage
- Visual disturbances or blurry vision
Classifying HELLP Syndrome
HELLP syndrome is classified as follows:
- Class I: Most Severe – platelet count of less than 50,000/µL
- Class II: Moderately Severe – platelet count between 50,000 & 100,000/µL
- Class III: Less Severe – platelet count between 100,000 & 150,000/µL
These criteria help identify a major complication of HELLP in pregnant women which is either hemorrhage during pregnancy or labor or uncontrolled bleeding following delivery whether vaginal or c-section.
HELLP Syndrome: Differential Diagnosis
To avoid misdiagnosis, medical providers should differentiate HELLP syndrome from other pregnancy-related disorders with similar characteristics:
- Preeclamspsia: Platelet count and liver enzymes are normal vs. HELLP where they are abnormal.
- AFLP or acute fatty liver of pregnancy: This condition is accompanied by hypoglycemia (low blood sugar level), but it is not found in HELLP syndrome patients.
- TTP or thrombotic thrombocytopenic purpura: Liver abnormalities in this condition are not as pronounced as in the case of HELLP. Patients typically have normal blood pressure (unlike HELLP).
- Lupus flare: In this autoimmune disorder, liver pathology is not present.
HELLP Syndrome: Risks and Complications
According to the American Pregnancy Association, the failure to correctly diagnose or treat HELLP syndrome can lead to life-threatening consequences for the pregnant woman as well as the baby.
Risks for the Mother
- Placental abruption (detaching of placenta from the uterus)
- Pulmonary edema (buildup of fluid in the lungs)
- Adult respiratory distress syndrome
- DIC or Disseminated Intravascular Coagulation (blood clotting disorder that may lead to heavy bleeding or hemorrhage)
- Ruptured liver hematoma (liver rupture)
- Kidney failure (acute renal failure)

Risks for the Baby
- IUGR or intrauterine growth restriction (retarded growth of the baby)
- Fetal Distress
- Placental Abruption or intrauterine bleeding leading to acute fetal asphyxia
- Infant respiratory distress syndrome
- IVH or intraventricular hemorrhage (brain bleeding)
- Birth asphyxia or fetal hypoxia
- HIE or hypoxic-ischemic encephalopathy (which may cause cerebral palsy)
- Cardiovascular problems
- Preterm birth and related birth complications, such as fetal bradycardia, infection, apnea (episodic cessation of breathing) and anemia
HELLP Syndrome Management
Management of women with HELLP syndrome will involve one of the following three major options:
- Immediate Delivery: At 34 weeks of pregnancy or more, immediate delivery is recommended. This could mean a preterm baby before 37 weeks’ gestation. Early birth becomes important because the risks and complications of HELLP for the mother and the baby significantly outweigh the risks of premature birth.
In case of anticipated preterm birth, the medical provider may administer antenatal corticosteroid therapy to support the baby’s lung growth and improve newborn outcomes. Betamethasone and dexamethasone are the commonly used corticosteroids to accelerate fetal maturation.
According to ACOG, a single course of bethamethasone is recommended between 34 and 36 weeks of gestation in this condition, if the pregnant woman has not received an earlier course of antenatal corticosteroids. - Delivery within 48 Hours: Between 27 and 34 weeks of gestation, the medical team may decide on a case by case basis for a delivery within 48 hours after a clinical evaluation, administration of corticosteroid therapy, and stabilization of the maternal condition. In relation to this, the medical providers must carefully weigh the potential benefits from a limited prolongation of pregnancy against the increased risk of complications for the mother and the baby.
The well-being of the baby must be monitored with electronic fetal monitoring during this period of time in order to detect any heart rate abnormalities that might be associated with fetal distress, fetal bradycardia or fetal hypoxia or asphyxia. If abnormalities are discovered an emergency c-section may be required. - Conservative Management: Before 27 weeks of pregnancy, the medical team may consider conservative management therapies for more than 48 to 72 hours. Corticosteroid therapy is typically used in this situation, but the regimens will significantly vary depending on the individual case. Close monitoring of the baby must be done under these circumstances as well.
*Conservative management is not recommended when the pregnant women is diagnosed with the DIC syndrome (which is a frequent cause of an abnormal hemorrhage tendency.)

Multidisciplinary Team Approach to Manage HELLP Syndrome
A multidisciplinary team approach is essential to the management of pregnant women with HELLP syndrome and its related complications. While an obstetrician primarily manages preeclampsia, they can benefit from assistance from other medical specialties when HELLP syndrome is diagnosed. An internal medicine physician can help manage the patient’s blood pressure and gestational diabetes.
Complications such as pulmonary edema will require help from a pulmonologist, while preparing for a caesarian section should involve an anesthesiologist. Continuous intensive care and nursing care will be necessary if the patient is admitted to an ICU. For the baby’s care and potential complications from HELLP syndrome, help from a neonatologist will be required in order to address issues including neonatal resuscitation.
Patient Education and Deterrence
Pregnant women with HELLP syndrome should be provided guidance about the course of the disease. The potential risks and complications to the mother and the baby as well as mortality risks should be informed to the patient and her family. In addition, the patient should be counseled about her risk of developing HELLP syndrome in subsequent pregnancies. Periodic lab tests and thorough prenatal care must be maintained in the subsequent pregnancies.
Is Your Child’s HELLP Syndrome Related Complication the Result of Medical Malpractice?
Parents whose children suffer from HELLP syndrome related complications deserve answers as to how their child developed this condition and whether the complications resulting from it were preventable.
- Were there signs during the pregnancy, labor, and delivery process that HELLP syndrome or its related complication was occurring, but accurate diagnosis, correct treatment, or an emergency c-section was either delayed or not performed at all?
- Was a neonatal resuscitation team not called to delivery in a timely manner to address breathing difficulties?
- Were signs of a fetal distress due to a known complication of HELLP like placental abruption not recognized and responded to in a timely manner?
Our dedicated birth injury lawyers want to help you find those answers and obtain that coveted financial reward necessary to provide care and therapy that can help improve the quality of your child’s life. A lawsuit settlement can improve the quality of life for your child.
If your child has been diagnosed with a HELLP syndrome related injury (including Hypoxic-Ischemic Encephalopathy (HIE) or cerebral palsy), and you suspect this may have been caused in part by medical mistakes, Miller Weisbrod Olesky will thoroughly investigate the facts and hold responsible medical providers accountable by pursuing medical malpractice claims against them.
The compensation our clients receive helps them pay for their child’s current and future medical treatment and devices to help the child adjust to living with a permanent disability, and to be able to pay for these cutting-edge devices.
Sometimes families are hesitant to reach out to a medical malpractice attorney or law firm. It’s also not uncommon for parents to feel overwhelmed by their circumstances and worried that they will not be able to help out in a lawsuit involving their child’s birth injury.
Registered Nurses and Nurse-Attorneys Are a Vital Part of Our Birth Injury Team … and Yours

Most national birth injury law firms will employ one or two nurses to assist the review of cases and medical research. But Miller Weisbrod Olesky offers an unmatched number of nurses and nurse-attorney employees support to both the birth injury attorneys and our clients.
Our team of registered nursing staff and nurse-attorneys bring a deep level of medical and personal insight to every client’s case. Our nursing team includes both an experienced labor and delivery nurse as well as an ICU nurse. Working closely with the rest of the team, they investigate the reasons behind a birth injury and how medical professionals breached their standard of care.
Why Should You Talk with the Knowledgeable Attorneys at Miller Weisbrod Olesky?

The only way to find out if you have a birth injury case is to talk to an attorney who understands birth injuries leading to a delay or failure in developmental milestones including birth injuries that cause cerebral palsy. It’s not uncommon that a HELLP syndrome related complication can be a preventable birth injury, but it takes a detailed expert review of the facts and circumstances of your child’s birth to determine the birth injury was the result of medical malpractice.
At Miller Weisbrod Olesky, a team of committed attorneys, nurses and paraprofessionals uses our detailed medical negligence case review process to assess your potential birth injury case. We start by learning more about you and your child and the status of meeting/missing developmental milestones. Then we gather medical records to determine what happened before, during, and after your delivery. We call in skilled medical experts who review your records and let us know if they think medical errors could have caused your child’s injuries.
If we feel medical negligence caused or contributed to your child’s injuries, we meet with you to discuss how you can receive compensation from the medical professionals who made the errors. Our birth injury attorneys have recovered millions of dollars in settlements for families of babies that have suffered a birth injury.
At no point in our legal intake process will we ask you to pay anything. The medical review of your case and the consultation are free. We only receive payment when you do. Don't hesitate to get in touch with us today to discuss your unique circumstances.
Contact Our National Birth Injury Lawyers
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.