Oligohydramnios
Oligohydramnios During Pregnancy
Oligohydramnios occurs when the amniotic fluid volume (AFV) during pregnancy is lower than expected for the baby’s gestational age. Amniotic fluid envelopes the in-utero baby to cushion their movements in the womb and protect them from complications such as infection or umbilical cord compression. Amniotic fluid is also vital for the development of the baby’s respiratory and digestive systems and is an important component in regulating their body temperature. Pregnant women normally have about 500 ml to 1,000 ml of amniotic fluid.

An abnormally low level of amniotic fluid may affect the baby’s health or could be an indicator of an underlying medical condition, which may create complications at the time of labor or delivery. Oligohydramnios affects about 4% of expectant mothers and is more commonly seen during the last trimester. In post-term pregnancies, the incidence of oligohydramnios is as high as 12% because amniotic fluid volume significantly reduces after 40 weeks of pregnancy.
Risks and Complications of Oligohydramnios
When oligohydramnios occurs in the first or second trimester, it’s usually more dangerous. Complications at this stage may include:
- Premature birth
- Stillbirth
- Miscarriage
- Infection (if the water breaks early)
- Deformities occurring due to in-utero compression
When oligohydramnios occurs in the third trimester (from week 28 to week 40) or later, the following birth complications could occur:
- Restricted fetal growth
- Umbilical cord compression
- Underdeveloped lungs
- Respiratory distress syndrome
- Increased risk of early or cesarean delivery
- Fetal heart rate decelerations
- Infection (if the water breaks early)
- Meconium aspiration
Obstetricians and labor-delivery nurses caring for a mother with known or suspected oligohydramnios must closely monitor the well-being of the baby including using an electronic fetal monitoring device. If warnings signs of fetal distress arise, the medical providers must be prepared to deliver the baby including performing an emergency c-section.
An expectant mother in Houston, Texas was diagnosed with oligohydramnios during her pregnancy. The obstetrician and nursing staff’s physical exam failed to note other conditions that, when combined with the inadequate amniotic fluid, should have indicated a c-section was the proper course. Labor was induced by Pitocin and the nursing staff and physicians failed to recognize and respond to predictable signs of fetal distress. Our young client was born with neurological difficulties. We were able to recover $3,500,000 to aid in her care and therapy despite the physician having very low insurance limits.
Factors that may Contribute to Oligohydramnios

Some of the common factors that may contribute to the occurrence of oligohydramnios include:
- Placental abruption (the placenta detaches from the uterine walls before the baby’s birth)
- Pregnancy that is two weeks past the due date
- Premature rupture of the membranes (PROM)
- Gestational diabetes
- Preeclampsia or maternal hypertension
- Twin-to-twin transfusion syndrome (TTTS, which is a rare condition affecting twins or multiples in the womb)
- Congenital defects affecting the baby’s urinary tract or kidneys (genitourinary tract abnormalities)
- Chromosomal abnormalities (seen in up to 10% of the cases of oligohydramnios in the second trimester)
- Fetal growth restriction (seen in up to 20% of cases of oligohydramnios in the third trimester)
- Dehydration
- Use of certain medications, such as ACE inhibitors during pregnancy (contraindicated during second and third trimesters)
While an expectant mother may not know that her amniotic fluid levels are low, the medical provider should suspect it if the uterus size is small, there is vaginal fluid leak, the mother is not gaining sufficient weight, or the mother does not feel the baby is moving enough. Occurrence of oligohydramnios in a past pregnancy is also a risk factor for low amniotic fluid in subsequent pregnancies.
Diagnosis Of Oligohydramnios
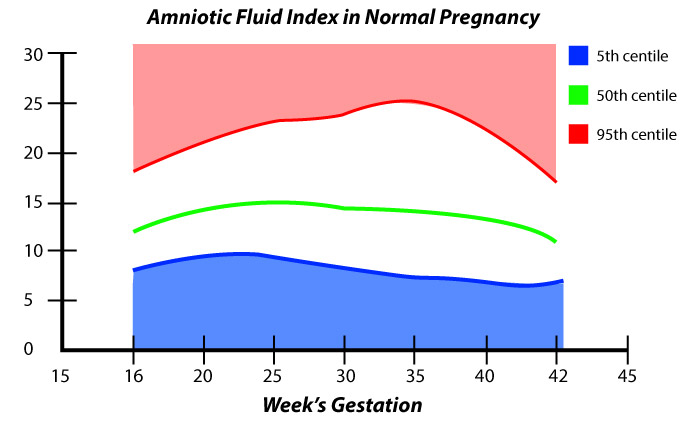
In a normal pregnancy, amniotic fluid volume (AFV) changes over the gestation period, gradually increasing until about 36 weeks of gestation. From this point forward until week 40 (term pregnancy), the AFV should remain constant.
Beyond week 40 (late-term pregnancy), the AFV begins to reduce steadily. These established patterns should enable the medical team to clinically evaluate AFV throughout the pregnancy using ultrasound tests and fundal height measurements (to determine if the baby is small for their gestational age).
At any stage, if the medical provider detects a discrepancy between the gestational age and fundal height measurement, they should order an AFV assessment with a transabdominal ultrasound. This ultrasound AFV assessment may include the use of:
- Amniotic fluid index (AFI) – it is the score given to the amount of amniotic fluid found during the ultrasound exam.
- Maximum vertical pocket (MVP) – it assesses a vertical pocket of maximal depth (deepest pocket) of amniotic fluid (excluding the umbilical cord or other fetal parts).
The normal MVP range is from 2 to 8 cm. When the pocket depth is less than 2 cm, it’s diagnosed as oligohydramnios. On the other hand, an MVP greater than 8 cm indicates presence of excessive amniotic fluid, which is a condition called polyhydramnios.
An alternative assessment using the amniotic fluid index (AFI) can be undertaken after week 20 of pregnancy. The sonographer will divide the uterus into 4 quadrants and determine each quadrant’s MVP. The sum total of 4 MPVs is the AFI. When the AFI is found to be less than 5 cm, the condition should be diagnosed as oligohydramnios.

Patient Education, Deterrence and Professional Teamwork
Medical providers should educate expectant mothers about oligohydramnios and emphasize on the critical importance of receiving regular prenatal care during the course of pregnancy. Appropriate prenatal care will enable the medical team to identify and diagnose conditions such as oligohydramnios. With timely diagnosis, the medical care providers can determine a comprehensive follow-up and monitoring plan to mitigate the risk of birth complications associated with oligohydramnios.
Clinical management of oligohydramnios and its associated conditions requires thorough teamwork and communication between care various medical providers to ensure proper screening, diagnosis, and treatment of these conditions at every stage of the pregnancy, labor, and delivery. When obstetricians or trained midwives perform regular and proper prenatal checkups, they should usually be able to detect oligohydramnios.
Once the diagnosis is confirmed, the obstetrician should consult with neonatologists and fetal-maternal medicine specialists in order to determine an optimal care strategy that will minimize the risk of complications for both the baby and the mother. Apart from focusing on the prenatal and neonatal care, the care plan should include the timing of delivery and advance preparation so there is no delay if a cesarean section is required.
Failure to order or perform a cesarean delivery on time, failure to monitor the baby and the mother during pregnancy for placental insufficiency, decreasing amniotic fluid volume, abnormal heart rate measurements, respiratory distress, fetal distress, as well as failure to address risk factors, such as dehydration, maternal hypertension, gestational diabetes, and use of ACE inhibitors can result in severe health complications or permanent disability like cerebral palsy or hypoxic-ischemic encephalopathy. These consequences can be avoided with diligent medical care and attention.
Evaluation and Management
Once the diagnosis is confirmed with ultrasound, the medical team should focus on making a clinical assessment of the underlying cause of oligohydramnios. This should include the following steps:
Maternal History
The obstetrician or maternal fetal medicine physician should review the detailed family history, maternal history, and medication use in order to identify any underlying conditions that may have contributed to oligohydramnios. The patient should be asked about any signs that indicate membrane rupture (such as underwear wetness or leakage of bloody or clear fluid.)
Physical Exam
The doctor should perform targeted physical exams, including: fundal height measurement, speculum examination (examining the vaginal and cervix health), and tests for fetal membrane rupture. Commercial tests for screening the rupture of membranes are available (such as ROM Plus and AmniSure), which are reported to have a high specificity and sensitivity.
Ultrasound of Fetal Anatomy
Following a confirmed diagnosis of oligohydramnios, the medical team should perform an ultrasound to assess fetal anatomy, including the bladder and kidneys to determine the baby’s growth status. If the fetal growth is normal with bladder and kidneys visualized, the chances of premature rupture of amniotic membrane (PROM) are high. Timely treatment for PROM can lead to favorable outcomes when infection is not present.
Early Term Delivery

Oligohydramnios could be a key indicator of placental insufficiency. Therefore, amniotic fluid volume (AFV) assessment is a part of the fetal biophysical profile (BPP, which is an evaluation of fetal breathing, fetal tone, fetal movement, and amniotic fluid volume).
Considering the risks to fetal health associated oligohydramnios, when the amniotic fluid index (AFI) is below 5 cm or the MVP is below 2 cm, the medical team should be ready to deliver the baby. The American College of Obstetricians and Gynecologists (ACOG) guidelines suggest that an MVP below 2 cm is a more reliable definition of oligohydramnios, and medical decisions should be made on this basis.
An early term delivery might be the safest option in this condition, if the gestational age is 36 or 37 weeks. If oligohydramnios is determined prior to 36 weeks of pregnancy, serial fetal ultrasound monitoring and fetal heart rate monitoring should be recommended.
When the expectant mother has low amniotic fluid during labor, the medical team may sometimes consider a procedure called amniofusion. In this case, a catheter is inserted through the cervix to deliver a saline solution to the uterus. Amniofusion is usually performed if abnormalities are detected in the baby’s heart rate.
Role of Fetal Hydration in Treating Oligohydramnios
Researchers over the years have studied the positive effects of administering water orally to the expectant mother with an aim to “hydrate” the fetus after oligohydramnios is diagnosed. Animal studies have shown a strong correlation between the hydration levels of the mother and the fetus.
In human studies, some researchers have found that increasing the mother’s intravascular volume (volume of blood in the circulatory system) could resolve oligohydramnios. A randomized study showed that orally administering water to expectant mothers diagnosed with oligohydramnios resulted in an increase in their amniotic fluid index (AFI).
As part of the study, the treatment group was asked to drink 2 liters of water within four hours of their AFI testing. Results showed a significant increase in AFI measurement (6.3 cm) compared to the control group (5.1 cm). Researchers concluded that an increase or decrease in oral intake of water can impact the AFI in women with oligohydramnios.
Another research study also showed that maternal oral hydration may be a safe, useful and well-tolerated strategy to increase the amniotic fluid volume in expectant mothers diagnosed with isolated oligohydramnios (IO). Researchers recommended that hypotonic solutions (where the fluid has a lower concentration than blood) are more useful than isotonic solutions (where the fluid concentration is higher than that of blood). Low dose oral administration (about 1,500 ml a day) for about two weeks can be helpful in these cases.
Is Your Child’s Oligohydramnios Related Birth Injury the Result of Medical Malpractice?
Parents whose children suffer from oligohydramnios related birth injury or birth complications want and deserve answers as to cause of their child’s injury and whether mistakes by the doctors and nurses contributed to the injury.
- Were there signs of oligohydramnios during the pregnancy, labor, and delivery process, or presence of risk factors such as preeclampsia, pregnancy-induced diabetes or a maternal infection, which were either not recognized or properly treated?
- Did the medical team fail to order a series of ultrasound monitoring tests to diagnose suspected oligohydramnios in a timely manner?
- Was the decision to perform a cesarean delivery delayed?
- During the labor and delivery, were there clear indications that their baby was suffering from fetal distress, but appropriate actions were not taken by the obstetrician or nurses?
- Did the neonatal resuscitation team delay in providing important breathing support after birth?
- Were serious neonatal conditions like hypoglycemia or jaundice missed or treated incorrectly?
The experienced birth injury lawyers at Miller Weisbrod Olesky will help you determine if mistakes of the medical providers caused a birth injury to your child. Our experienced birth injury attorneys have represented families all over the United States in their time of need after a birth injury. We use our experience and expertise to obtain you and your child a medical malpractice settlement that will help provide specialized medical therapy like speech in order to maximize the quality of life and independence of your child throughout their life.
Sometimes families are reluctant to contact a medical malpractice lawyer. It’s also not uncommon for parents to feel overwhelmed by the responsibilities they encounter in caring for their injured child and worried that they will not be able to help out in a lawsuit involving their child’s birth injury. Our birth injury attorneys and nursing staff will address these hesitations and concerns, so you can focus on your child and maximizing their care.
Registered Nurses and Nurse-Attorneys Are a Vital Part of Our Birth Injury Team…and Yours

Most national birth injury law firms will employ one or two nurses to assist the review of cases and medical research. But Miller Weisbrod Olesky offers an unmatched number of nurses and nurse-attorney employees support to both the birth injury attorneys and our clients.
Our team of registered nursing staff and nurse-attorneys bring a deep level of medical and personal insight to every client’s case. Our nursing team includes both an experienced labor and delivery nurse as well as an ICU nurse. Working closely with the rest of the team, they investigate the reasons behind a birth injury and how medical professionals breached their standard of care.
Why Should You Talk with the Knowledgeable Attorneys at Miller Weisbrod Olesky?

The only way to find out if you have a birth injury case is to talk to a lawyer experienced in birth injury lawsuits. It’s not uncommon that a birth related complication results in a preventable birth injury, including cerebral palsy, but it takes a detailed expert review by a birth injury attorney of the medical records from your child’s birth to determine if the birth injury was the result of medical malpractice.
At Miller Weisbrod Olesky, a team of committed lawyers, nurses and paralegals uses our detailed medical negligence case review process to assess your child’s potential birth injury case. We start by learning more about you and your child and the status of meeting/missing developmental milestones. Then we gather medical records to determine what happened before, during, and after your delivery. We call in skilled medical experts who review your records and let us know if they think medical errors could have caused your child’s injuries.
If we feel medical negligence caused or contributed to your child’s injuries, we meet with you to discuss how you can receive compensation from the medical professionals who made the errors. Our birth injury attorneys have recovered millions of dollars in settlements for families of children that have suffered a birth injury.
At no point in our legal intake process will we ask you to pay anything. The medical review of your case and the consultation are free. We only receive payment when you do.
Miller Weisbrod Olesky
At Miller Weisbrod Olesky, the attorneys, nurses, and staff understand that parents of children with birth injuries feel overwhelmed. So, every client has the attention and support of a team of trained, compassionate professionals. But we don’t just offer compassion.
We offer a process to help you discover whether your child’s birth injury, HIE, cerebral palsy or brain injury was caused by a medical error.
Call our offices today at 888.987.0005 for experienced assistance in a free consultation.
Quick Links
Testimonials
- Lyric C. I feel like our voice was heard in a sense of what can possibly go wrong in a delivery and finding us answers. I feel with our settlement, we are now in a comfortable position to provide for our son.
- Lyssa L. They are not just people that say “hey let's get you money and let's go” The law firm was very thorough with us. It was awesome. I don't want to cry, because I think about and it's amazing that they were able to help me and that we were able to help my son and get the story out there.
- Jay C. Throughout the process, one thing was clear to us, the ultimate interest of our child was the utmost concern of Max and his team and as parents navigating a situation like that, that was refreshing to know we had them firmly on our side. I highly recommend them.